Image source: The Motley Fool.
eHealth (EHTH -2.60%)
Q2 2020 Earnings Call
Jul 23, 2020, 5:00 p.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Ladies and gentlemen, thank you for standing by, and welcome to the Q2 2020 eHealth, Inc. earnings conference call. [Operator instructions] Please be advised that today's conference is being recorded. [Operator instructions] I would now like to hand the conference over to your speaker today, Ms.
Kate Sidorovich, vice president of eHealth investor relations. Thank you. Please go ahead.
Kate Sidorovich -- Vice President of Investor Relations
Thank you. Good afternoon, and thank you all for joining us today either by phone or by webcast for a discussion about eHealth, Inc.'s second-quarter 2020 financial results. On the call this afternoon, we'll have Scott Flanders, eHealth's chief executive officer; Tim Hannan, chief revenue officer; and Derek Yung, chief financial officer. After management completes its remarks, we'll open the lines for questions.
As a reminder, today's conference call is being recorded and webcast from the IR section of our website, and a replay of the call will be available on our website following the call. We will be making forward-looking statements on this call that include statements regarding future events, beliefs and expectations, including statements relating to our expectations regarding our Medicare business, including Medicare enrollment growth, consumer demand, our competitive advantage, our carrier relationships and our expectations regarding online enrollments; our plan to invest in the Medicare business, including marketing initiatives and enhancements to our technology platform; our Medicare growth strategy, including our customer acquisition and demand generation strategy, customer retention efforts, online engagement, agent productivity and talent acquisition strategy; our expectations regarding our direct-to-consumer platform, the benefits of our customer care agent remote model, the profitability of our business, seasonality, churn, lifetime values, operating expenses, including fixed and variable costs, and the impact of COVID-19 on our business; and finally, our member estimates revised 2020 full year guidance; our outlook for the third and fourth quarters of 2020; and our revised five-year financial plan and the contents of such guidance and growth plans. Forward-looking statements on this call represent eHealth's views as of today. You should not rely on the statements as representing our views in the future.
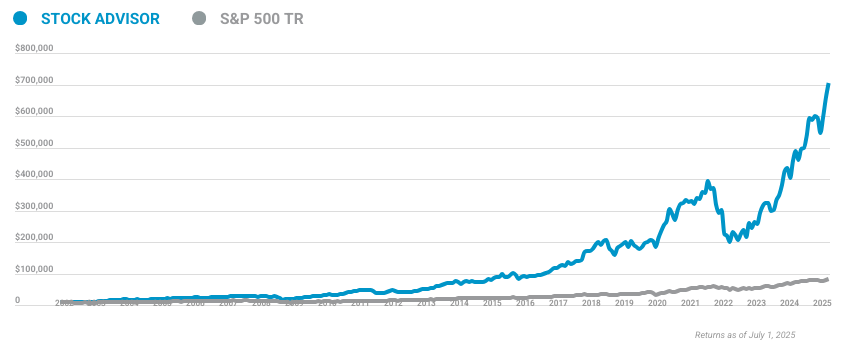
10 stocks we like better than eHealth
When investing geniuses David and Tom Gardner have a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
David and Tom just revealed what they believe are the ten best stocks for investors to buy right now... and eHealth wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of June 2, 2020
We undertake no obligation or duty to update information contained in the forward-looking statements, whether as a result of new information, future events or otherwise. Forward-looking statements are subject to risks and uncertainties that could cause actual results to differ materially from those projected in our forward-looking statements. We describe these and other risks and uncertainties in our annual report on Form 10-K and quarterly reports on Form 10-Q filed with the Securities and Exchange Commission, which you may access through the SEC website or from the investor relations section of our website. We will be presenting certain financial measures on this call that are considered non-GAAP under SEC Regulation G.
For a reconciliation of each non-GAAP financial measure to the most directly comparable GAAP financial measure, please refer to the information included in our press release and in our SEC filings, which can be found in the About Us section of our corporate website under the heading Investor Relations. However, we have not reconciled our projected EBITDA in 2024 to our projected GAAP net income because we cannot reasonably predict certain items in the reconciliation such as stock-based compensation expense and provision for income taxes. And the reconciliation is not available without unreasonable effort. And at this point, I will turn the call over to our CEO, Scott Flanders.
Scott Flanders -- Chief Executive Officer
Thank you, Kate, and welcome, everyone. We continue to operate in unprecedented and challenging times. Access to the proper healthcare is critical, and our mission to connect every person with the highest quality, most affordable health insurance for their life circumstances is more relevant and important than ever. This is especially difficult time for eHealth's customers who are mostly seniors, a group that is disproportionately impacted by the ongoing pandemic.
I'd like to thank our team for their hard work and dedication to helping those customers and continuing to fulfill our mission. We're going to use this call to discuss our second-quarter results, provide you with our updated 2020 annual guidance and the key points of our revised five-year financial plan. We will also discuss the strategies we are implementing to position the business for continued profitable growth. In the second quarter, eHealth delivered strong revenue and Medicare enrollment growth.
Consumer demand on our platform remained robust, and our agent productivity increased compared to a year ago driven by internal initiatives and favorable market dynamics. The number of second quarter Medicare-approved members grew ahead of our expectations. This includes a 65% year-over-year growth in approved Medicare Advantage members. We achieved this enrollment growth while also reducing our total acquisition costs per approved Medicare member, allowing us to once again exceed our internal forecast for revenue and earnings.
It's also worth highlighting that 30% of our second-quarter applications for Medicare major medical products were submitted by our customers online compared to just 11% a year ago. This includes unassisted and partially agent-assisted online enrollments. On an absolute basis, the total number of applications for Medicare major medical products submitted online grew over 300% compared to the second quarter of 2019. Later, I'll talk about some of the initiatives we have under way to continue exploiting our online opportunities.
Total revenue for the second quarter was $88.8 million, a 35% year-over-year increase. Our adjusted EBITDA was $1.7 million and our GAAP net loss was $3.4 million. Medicare revenue of $80.4 million grew 54% compared to a year ago. During the quarter, we completed our operational planning for the upcoming annual enrollment period and updated our financial forecast for the year.
We are anticipating a strong, fast paced AEP with robust Medicare Advantage plan selection and an acceleration in market share gains by tech-enabled direct-to-consumer platforms. This year, we're building on our success and knowledge gained over the last two AEPs with significant enhancements planned across all key functions. First, our Medicare agent productivity is expected to increase significantly this AEP by 10% compared to a year ago. This will be driven by new technology deployment, enhanced lead ranking allocation systems and a larger percent of in-house agents, including our remote agent force.
Second, we plan to further increase our online enrollment penetration. With online Medicare enrollments coming in substantially ahead of our forecast in the second quarter, we are increasing our full year 2020 targets for online enrollments from 34% to 37% of total applications for Medicare major medical products. This includes for unassisted and partially agent-assisted online enrollments. And in combination with higher agent productivity, it is expected to drive a significant year-over-year reduction in our customer care and enrollment costs per approved member.
Third, we will continue our strong multichannel demand generation strategy with increased reliance on data analytics and a growing contribution from our strategic partner channel, including a number of important new partners. We believe our partner channel is a major differentiator for eHealth. It will be one of the drivers to improve our marketing cost of acquisition forecasted for this AEP. Fourth, we plan to enter AEP with deeper carrier relationships and a better than previously expected contribution for Medicare advertising revenue.
Finally, going forward, we plan to place a stronger operational focus on member retention and recapture. Ahead of AEP, we are launching an important new technology platform, the Customer Center. It is built around our customer and their data in order to personalize customer experience across all points of interaction with eHealth to enhance post-enrollment interaction and deepen our relationships with our members while increasing brand awareness. Based on the strength of our business, stronger expected growth in our online Medicare enrollments and the capital raise we completed in March, we are increasing our financial guidance for the full year ending 2020.
Derek will share the details of our updated guidance later on the call. Turning now to our longer-term strategic plans. The Medicare market environment is highly favorable with significant demographic and regulatory tailwinds. We expect for all major direct-to-consumer comparison platforms in our space to do well in the near term, continuing to gain market share away from the traditional broker channel.
Of these platforms, we believe that eHealth is best positioned for market leadership because of our differentiated and personalized consumer-oriented technology platform. Let me expand on that some more. Technology and e-commerce have been in the DNA of eHealth since inception. Our focus and investments in technology and innovation have established a best-in-class e-commerce platform in our industry.
Our technology provides consumers with a superior user experience, broader product choice and advanced plan selection tools. A critical aspect of this platform is our software and data-driven analytics that support both the licensed agent force and customers shopping on their own online, providing a unified and flexible approach to selecting and purchasing a Medicare plan. These technology investments contrast with those of our peers, which have been predominantly focused on call center technology and not on the complex issues to optimize the consumer experience and relationship. While we believe these investments provide us with durable competitive advantages, they do have a dampening effect on near-term margins.
This is deliberate. Derek will expand upon the financial dimension more in his remarks. The last months have accelerated the shift to digital, which was already under way. This shift has been evident across many industries in the recent months, particularly among seniors who are looking for a safe consumer environment.
We are clearly seeing this trend on our platform, and given our long-standing focus on e-commerce, we are in a strong position to take advantage of it. In addition to providing omni-channel flexibility and convenience to our customers, online enrollments are more profitable, provide superior operational scalability and are characterized by higher member persistency. By growing online penetration, we are not only enhancing consumer value relative to other market participants, but we are also creating a foundation for a more profitable, more scalable model. Driven by the strength of our execution, we are currently tracking significantly ahead of the five-year financial plan that we provided at our Analyst Day in May of 2019.
Given our significant outperformance to date and our revised outlook, we are updating our five-year financial plan. Under the revised five-year financial plan, we forecast to generate $1.5 billion in revenue by 2024 with an adjusted EBITDA margin of 38%. The high case of the revised plan calls for $2.1 billion in revenue with a 41% adjusted EBITDA margin in 2024. Importantly, we now plan to start generating positive cash flows from operations in fiscal year 2022 under both scenarios.
Our enrollment growth has been exceptionally strong in the past 12 months and is expected to remain strong throughout our five-year financial plan. In addition, our member profitability is expected to be unchanged or even favorable this year compared to 2019, driven by greater acquisition cost efficiencies. That said, in the first half of this year, we saw increased levels of Medicare Advantage plan churn compared to our historic observations. We took action as soon as we identified this dynamic and moved retention initiatives that were already in the works to the top of our strategic and operational priorities.
Let me provide some more color on this. Over the last four years, we've been executing a transaction-driven strategy, which was aimed at optimizing consumers' enrollment experience and driving scale and market share. This was a deliberate strategic focus and it delivered significant results. However, as we look ahead to the next five years, we're making a strategic decision to increase our focus on member retention and recapture.
We have assembled a dedicated team led by Tim Hannan, eHealth's chief revenue officer, to identify the key drivers of elevated churn and to develop a comprehensive action plan to address it. The team determined that the recent increase in churn has been driven by a combination of macro factors and some factors that are specific to our business model that we should be able to effectively control. On the macro side, consumers are faced with broader plan choice and multiple enrollment opportunities throughout the year, which is benefiting the broader MA market and increasing the market share of MA plans. At the same time, these dynamics have also led to more shopping and more switching by MA members.
In this environment, we need to have a robust member retention and recapture strategy in place and are implementing a number of critical initiatives in time for AEP, which Tim will describe in detail. One thing that I'd like to emphasize is the importance of our online strategy to these retention efforts. Increasing online enrollments, both in absolute numbers and as a percent of total Medicare enrollment, is a critical element of our business. Our online users have persistency that is significantly higher compared to those that engage with us telephonically.
This spread further widened in the last two quarters, in which most of the elevated churn was driven by telephonic enrollments. As a result, online users have higher LTVs while also requiring lower acquisition costs, both providing for superior member economics. In closing, we are pleased with our results for the quarter. We have a robust outlook for the remainder of 2020 and beyond, which we are reflecting in our revised 2020 guidance and the five-year financial plan.
In the near term, we are working with urgency to address churn and are confident that we are taking the right actions to build on our strengths and market-leading position. Finally, let me conclude by saying that, four years ago, I shared our strategy for growing our business and building market share of our consumer-centric platform. Simply put, we have delivered on those plans. Our recent results reflect the underlying strength of our business model and the strategic actions we have made to grow our omni-channel offering.
I am confident that we have many years of growth ahead. And with this, I'd like to turn the call over to Tim Hannan, our chief revenue officer.
Tim Hannan -- Chief Revenue Officer
Thank you, Scott, and good afternoon, everyone. As Scott shared, our goal is to create the most compelling omni-channel shopping experience for Medicare consumers and deliver expanding margins in the process. At the beginning of 2020, we saw that we could improve upon the extraordinary performance we saw in 2018 and 2019 by bringing our marketing and sales teams together in one organization under the revenue function. During Q1, we conducted a thorough review of our sales and marketing practices with the help of external consultants and identified a number of critical initiatives that would allow us to reduce our variable cost per member.
These included a smarter way to plan agent force expansion, an improved process for managing agent licensing and appointments, and a marginal investment model for future marketing investments, to name a few. We recently expanded on those improvements with the launch of a new agent performance management model and an upgrade to our call routing system that better accounts for both agent skill and call quality. We also rapidly expanded our work-from-home capabilities given the COVID-19 crisis. Some of these initiatives have already yielded meaningful results in the second quarter with an increase in agent productivity and a 7% decline in total cost per approved Medicare member compared to a year ago.
But the full impact of these changes will be felt in the fourth quarter. Regarding our retention initiatives, as Scott outlined, we mobilized our leadership team to address the elevated churn levels when they became apparent after the Medicare Advantage open enrollment period that runs through the first quarter. While there are a number of environmental factors that contribute to churn, which Scott shared, we believe there are factors that are within our control and which we are already working to remedy for this AEP. Our primary opportunity is to improve the quality of our telephonic sales process, and we have a number of levers to achieve better performance.
The recent increase in churn levels occurred most significantly in our telephonic enrollment. Our analysis has shown that we experienced deteriorating retention on the telephonic enrollment completed by less tenured agents, particularly those from our vendor partners. For this year's AEP, we are shifting to a healthier balance of internal and vendor agents. Our remote staffing model that was launched in March affords us greater flexibility and cost effectiveness in expanding our full-time agent force.
We are also changing the performance management model, including the compensation structure of our agents to better align it with our member retention goals. Additionally, we are bringing our data science and technology to improve the telephonic experience with enhanced call scoring and planned recommendation algorithms to better position our agents for success. On the customer relations side, our focus historically has been on enrollment growth and providing a best-in-class shopping experience to consumers rather than on retention and post-transaction experience. We are now planning to place a much stronger emphasis on retention and the post-transaction experience going forward.
Ahead of AEP, we are expanding our retention sales team and launching a new technology platform to enhance the quality of our communications with new customers after the initial enrollment. Given the seasonal cycle of our enrollments in churn, the positive impact of these initiatives on our LTVs will not be reflected in our financial results until Q1 of next year and therefore, is not assumed in our 2020 guidance. The positive impact is incorporated into the long-range plan that Scott discussed. In addition, as we continue to grow contribution of our online enrollments, it should also have a positive impact on our overall churn rates given that our Medicare Advantage members who enrolled online during AEP tend to retain the product longer with first year retention rates higher by approximately 25% to 30% compared to members who enrolled telephonically.
We are now in the midst of our AEP preparations, and I expect it to be another success, building on our experience and achievements of the last two years. We have substantial enhancements planned across all of our key functions ahead of this important selling season. With these improvements, we plan to deliver a better experience to our customers, lower our variable costs and leverage our technology investments. And now I'd like to turn the call over to Derek Yung, our chief financial officer.
Derek Yung -- Chief Financial Officer
Thanks, Tim, and good afternoon, everyone. Second quarter financial results exceeded our expectations driven by strong consumer demand due in part to the COVID-related special enrollment period for Medicare beneficiaries introduced during the quarter, strong online enrollment growth and continuing productivity gains by our agent workforce. Growth in Medicare revenue and enrollment was accompanied by a year-over-year reduction in total acquisition costs per approved Medicare member, reflecting the initial impact of measures under way aimed at achieving enhanced cost effectiveness of our demand generation and fulfillment. In our Medicare business, our second-quarter revenue of $80.4 million grew 54% compared to a year ago due primarily to a 65% year-over-year increase in approved Medicare Advantage members and a 69% growth in Medicare carrier advertising revenue.
The Medicare segment generated a profit of $13.4 million, 120% growth compared to the second quarter of 2019. Second-quarter 2020 revenue from our Individual, Family and Small Business segment was $8.4 million, a decline of 38% compared to a year ago. A positive impact from an 86% increase in approved members on major medical IFP policies was offset by lower new enrollments in ancillary products, including short-term plans and a decline in IFP tail revenue compared to a year ago. The Individual, Family and Small Business segment remained profitable with a $2.6 million profit for the second quarter.
Our total revenue for the second quarter was $88.8 million, an increase of 35% compared to the second quarter of 2019. As we continue to generate significant top line growth, our goal is to maintain attractive member economics with an emphasis on the ratio of lifetime value to total acquisition costs, including marketing and agent-related expenses. Our technology-driven and online strategies have multiple levers to drive our acquisition costs to match our growth and profitability targets. In the last two years, lifetime values in our Medicare Advantage business have been increasing driven by growth in broker commissions and favorable commission collections relative to our estimates.
This allowed us to aggressively pursue enrollment and market share growth by investing in marketing and customer care. However, in the first half of the year, we have observed churn levels in our Medicare Advantage business that were elevated relative to historical levels. This had a negative impact on our second quarter MA LTVs and our estimates for the full year 2020 LTVs. As Tim discussed, the increase in churn had a more pronounced impact on our newer member cohorts and our telephonic enrollments while online enrollments continued churn at lower levels.
Although we don't yet have full visibility into the second-quarter churn given the significant amount of time after end of the quarter before we observe it, we expect that it was also elevated compared to historical Q2 levels, especially because of the COVID-related special enrollment period that was in effect for a large part of the quarter. We currently project for MA LTVs to decline up to 10% in the fourth quarter of 2020 and by mid-single digits for the full year, which has been reflected in our revised 2020 annual guidance. At the same time, our acquisition costs per approved Medicare member is forecasted to decline by approximately 13% in the fourth quarter of 2020 and 10% for the full year 2020 compared to 2019. As a result, our Medicare member profitability, as reflected by the LTV to total acquisition cost per member ratio, is expected to remain favorable and could actually improve for the full year 2020 compared to a year ago, which will have a positive impact on our overall profitability.
In addition, as Tim described, we're in the process of implementing a number of high priority initiatives aimed at enhancing our member retention and eventually lifetime values of our members. Due to specifics of our enrollment and accounting cycles, the impact from our retention programs will take longer to flow through our member economics compared to cost-related initiatives. We currently expect to get back to 2019 LTV levels for our MA product for the full year 2021. Outside of Medicare Advantage, we are also seeing higher levels of churn in the PDP product driven primarily by growing popularity of MAPD plans versus stand-alone PDP plans.
At the same time, we observed favorable persistency trends in our Medicare Supplement book of business with a significant year-over-year increase in MS lifetime values in the second quarter. The estimated number of our revenue generating Medicare members was approximately 716,000 at the end of the second quarter or an increase of 37% compared to a year ago. Turning to profitability metrics. GAAP net loss for the second quarter of 2020 was $3.4 million compared to GAAP net loss of $5.8 million for the second quarter of 2019.
Adjusted EBITDA for the second quarter of 2020 was $1.7 million compared to $0.8 million for the second quarter of 2019. We calculate adjusted EBITDA by adding stock-based compensation expense, change in fair value earnout liability, depreciation and amortization, amortization of intangible assets, other income, and benefit from income taxes to our GAAP net loss. Our second-quarter cash flow from operations was negative $21.3 million compared to negative $11.5 million for the second quarter of 2019. As of June 30, we had $211 million in cash, cash equivalents and marketable securities, and we had no debt outstanding under our line of credit.
Our balance sheet also reflected significant commissions receivable balance of $583 million. We are increasing our annual guidance for the second time this year to reflect our second-quarter outperformance and growth opportunities provided by capital raised through our equity offering in March of this year. I will now provide guidance highlights, and you can find the full revised guidance ranges in our earnings release issued earlier today. We're now forecasting revenues for 2020 to be in the range of $630 million to $670 million compared to prior guidance range of $600 million to $640 million.
We expect GAAP net income for 2020 to be in the range of $79 million to $94 million compared to prior guidance range of $70 million to $85 million. We expect 2020 adjusted EBITDA to be in the range of $140 million to $155 million compared to the prior guidance range of $125 million to $140 million. Within these numbers, there are some dynamics related seasonality to be mindful of when thinking about quarterly outlook for the remainder of the year. Specifically, in the third quarter, we expect a sequential decline in our revenue, driven primarily by seasonally low Medicare enrollment volumes.
On the operating side, we expect a significant sequential increase in our third quarter costs. This expected increase in costs will be driven primarily by our customer care enrollment expense as we ramp up agent hiring and training ahead of the fourth quarter annual enrollment period. Given that Q3 is a seasonally low volume quarter and because it takes several weeks for new agents to become productive, we anticipate a significant increase in third quarter customer care costs per approved member and a large sequential drop in EBITDA. The fourth quarter is expected to be the largest quarter in terms of enrollment volume, revenue and profitability driven by AEP.
For the full year 2020, we expect to deliver another increase in EBITDA margins with 23% margin at the midpoint of our annual guidance compared to a 20% margin a year ago after excluding the impact of the $42.3 million tail revenue adjustment in the fourth quarter of 2019 from 2019 EBITDA. In addition to the seasonality dynamic, there are some important context when thinking about our EBITDA margins. The 23% EBITDA margin at the midpoint of our guidance is attractive but is deliberately below the margins of our peers due to investments we are making in technology to further differentiate our platform. During 2020, our operating expenses are expected to include technology investments of approximately $64 million or 10% of revenue at the midpoint of our guidance range.
Over the next several years, these investments will become less significant as a percentage of revenue, which we expect to drive meaningful margin expansion starting in 2021. This provides a nice segue for me to review the highlights of our updated five-year financial plan that reflects our significant outperformance to date and our strategic and financial plan for the next several years. As you recall, we previously expected to generate $425 million in 2020 of revenue under the base scenario and $448 million revenue under the tailwind scenario. The midpoint of our revised 2020 guidance of $650 million represents a 53% upside and a 45% upside, respectively, to the base case and tailwind scenarios of the old plan.
We are tracking well ahead of our EBITDA targets. Stronger than previously expected enrollment growth combined with better agent productivity and higher contribution from online enrollments have all contributed to our outperformance to date. Going forward, we expect to continue to drive strong enrollment growth while significantly increasing the contribution from online enrollment. The updated five-year financial plan also reflects a more disciplined approach to growth with an emphasis on high ROI marketing channel and stronger operational emphasis on member retention.
The forecast period in the five-year financial plan has 2019 as the base year after excluding the impact of the $42.3 million tail revenue adjustment in the fourth quarter of 2019 and projects our performance through 2024. Under the revised base case scenario, we expect revenue CAGR of 27% getting us to $1.5 billion in 2024, an EBITDA CAGR of 45% with approximately $570 million EBITDA by 2024 or 38% margin. Under the base case scenario, we also expect that, by 2024, online enrollments will represent 53% of total Medicare major medical applications. Under the revised high case scenario, we expect revenue CAGR of 35%, getting us to $2.1 billion in 2024 and EBITDA CAGR of 57% with approximately $850 million EBITDA by 2024, a 41% margin.
Under this scenario, we expect that, by 2024, online enrollment will represent 57% of total Medicare major medical applications. As Scott mentioned, under both scenarios, we expect to generate positive cash flows from operations in fiscal year 2022. And finally, both scenarios assume that, by 2021, we get back to 2019 levels of Medicare Advantage LTVs and stay roughly at these levels for the duration of the forecast period after a mid-single-digit decline we expect to see this year. I want to remind you that these comments in our guidance are based on current indications of our business and our current estimates, assumptions and judgments, which may change at any time.
Our actual results may differ as a result of changes in our estimates, assumptions and judgments. We undertake no obligation to update our comments or our guidance. Let me turn the call back to Scott for closing remarks before we open the call for questions.
Scott Flanders -- Chief Executive Officer
Thank you, Derek. Before we open for questions, I want to emphasize three key takeaways from our conversation today: First, eHealth is differentiated by our unique consumer-centric platform that provides a strong foundation to drive key online enrollment growth and to win in the market as health insurance distribution continues to evolve; Second, we have had a strong second quarter and our increase in guidance to reflect the investments we are making and the opportunities we expect to capture in the upcoming AEP; Third, we are taking decisive actions to address our churn levels. We have resources dedicated to it and a plan in place to tackle the issue. Finally, we are very excited about the future of eHealth.
Building on our success over the last four years, we are moving forward with a five-year plan that will enable us to capture organic growth opportunity in the Medicare market, increase profitability and deliver enhanced value to our shareholders. With that, let's open the floor to Q&A. Operator?
Questions & Answers:
Operator
Thank you. [Operator instructions] Our first question comes from Jailendra Singh with Credit Suisse. Your line is now open.
Jailendra Singh -- Credit Suisse -- Analyst
Hi. Thanks. Hello. Just a quick follow-up on your long-term outlook comment.
So you expect online enrollment percentage to almost like double from what you did in 2019, and you also said that the retention rate on online sign-up is, of course, trending much higher. Then all the investments you are doing should benefit retention rate as well. Just wondering why you guys don't expect your MA LTV to improve from what you did in 2019 of like 1,050, I mean compared to some of the other competitors are like more 1,200. Just trying to understand like what is the offset in your LTV assumption.
Scott Flanders -- Chief Executive Officer
Well, we think our LTVs are very conservative. We have built into the long-range plan is just a 1% CAGR in both the base case and the high case off of the '19 level. So this year, we've dipped down. We'll stabilize back to '19 levels in 2021 and then grow modestly single-digit rate above 2021.
So it is an element of conservatism in the plan, and it's likely to overperform.
Jailendra Singh -- Credit Suisse -- Analyst
OK. And then my follow-up is around the churn rate, and I'm sorry if I missed this comment. But can you comment on did you see churn rate improve or not improve sequentially from Q1 to Q2 for your Q4 2019 cohort? And if you can parse out whether you saw spike in churn once SEP was put in place or even before SEP was announced, the churn was trending higher. Just give us some perspective intra-quarter and especially for Q4 2019 cohort.
Scott Flanders -- Chief Executive Officer
Right. Derek, I'd ask you to take that.
Derek Yung -- Chief Financial Officer
Yes. So Jailendra, we saw churn tick up in the OEP period, and it's a combination, obviously, from a more senior taken opportunity to switch plans, not just our platform but generally what we observed in the industry. And also with the full visibility of the data coming in through the OEP and AEP period, we did see that there was a slightly higher elevated churn than our initial estimate for the 2019 AEP enrollments.
Jailendra Singh -- Credit Suisse -- Analyst
Because like just trying to understand, is it Q1 — even Q2 churn was higher than Q1 churn?
Derek Yung -- Chief Financial Officer
We don't have full visibility in the Q2 churn yet, but quarter to date, we have not seen churn to be higher, which seasonally makes sense because we don't have OEP in Q2. Even though we had a special enrollment period, we had not seen the uptick in terms of member switching at the levels we saw in Q1 with the OEP.
Jailendra Singh -- Credit Suisse -- Analyst
Because the reason I ask — I know, I'm sorry, it's the third question. But the reason I ask is that if I look at your LTV assumption for second half, I mean, you do expect like LTV absolute dollars similar to Q2 but year-over-year, it implies decline. But technically, I mean, LTV generally improves as churn rate improves in prior year, right, from Q2 to Q3 to Q4. Just trying to understand like what are you? I mean why is LTV — how are we thinking about LTV for second half versus what you have seen in first half?
Scott Flanders -- Chief Executive Officer
Jailendra, just specific to your question was from Q1 2019 to Q2 2019, did we see churn sequentially increase, and the answer is yes. So it went up about the same percentage amount Q1 to Q2 '19, Q1 to Q2 '20.
Jailendra Singh -- Credit Suisse -- Analyst
Thank you.
Operator
Our next question comes from George Sutton with Craig-Hallum. Your line is now open.
George Sutton -- Craig-Hallum Capital Group LLC -- Analyst
Thank you. You specifically referenced the telephonic enrollment as being one of the items that you thought was having an impact on your churn rate. I'm wondering if you've done some diagnosis and can explain why is this the case in your view.
Scott Flanders -- Chief Executive Officer
That's definitely correct, George. Tim, why don't you take that?
Tim Hannan -- Chief Revenue Officer
Sure. Yes. So we spend a long time diagnosing the telephonic sales process and really identify opportunities to improve it at every stage. So we can do — at the front end, we will have a healthier mix of internal versus vendor agents.
So we can see that newer agents are not as effective as older agents and vendor agents are not as effective as internal agents. And so we've been scaling up our workforce rapidly. This has led to probably — definitely to an increase in churn. Then once somebody is in the shopping process, we saw that we could provide better tools.
So as Scott mentioned, there's a broadening of plan selection. We are bringing better algorithms this year for our agents to use to make better recommendations to the telephonic customers, whereas in online, there's that research themselves. We're also better aligning our compensation with our agents to paid apps. So a couple of years ago, we paid on submitted.
Then we moved to approved. Now we're moving to a framework where we'll pay on approved but keep basically a draw and pay it out later to our agents if they put people in the right plan. Basically, they get paid when eHealth gets paid. So there are a number of these sorts of steps that we think work ...
Scott Flanders -- Chief Executive Officer
George?
George Sutton -- Craig-Hallum Capital Group LLC -- Analyst
Yes. I'm here. I wasn't hearing Tim. One follow-up if I could.
Obviously, we're very focused on churn, but you are meaningfully guiding higher. So it sounded like stronger partner relationships and stronger position with carriers was a reason behind that. And I wondered if you can go into a little bit more detail in terms of what you meant there.
Scott Flanders -- Chief Executive Officer
Well, the strategic partner channel, we launched three years ago and is — just in the second half of last year, started to really gain momentum, has been a bright spot for us through the first half of the year and start — is off to a very good start already through the first three to four weeks of July. And that we expect that to be a real differentiator for us long term. A lot of those relationships are with hospitals and our 3-year exclusive deals. We have a lot of pharmacy relationships that are — they were soft in the first half, not surprisingly, given COVID and being overwhelmed with the issues they faced.
But again, starting just about a month ago in mid-June, the pharmacy channel started to gain momentum as well. So the partner channel, very important. What was the other part of your question, George?
Tim Hannan -- Chief Revenue Officer
Scott, I'm back by the way.
George Sutton -- Craig-Hallum Capital Group LLC -- Analyst
Related to the position with the carriers.
Scott Flanders -- Chief Executive Officer
Yes. So yes, look, the carriers are increasingly dedicating resources and focus and attention to the telephonic distribution channel, of which we are a part. We think we're a differentiated model slightly, but we're part of that broad sector, which includes GoHealth and SelectQuote and Transact and others. And the carriers are realizing that this channel is very efficient for them.
In many cases, in most cases, it's cheaper, even fully loaded with commissions and other advertising revenues that they support the channel with than their own fully loaded captive sales forces. In addition, the captive sales forces are facing challenges this year with respect to securing face-to-face appointments with seniors because of their concerns over personal safety, understandably. And so my discussions with the carriers would suggest that they are investing heavily in the third-party distribution channel as a hedge against their captive channels underperforming. So we think this is a real positive for us, and it's reflected in us increasing in our guidance, our expectation for advertising revenue coming from the carriers.
George Sutton -- Craig-Hallum Capital Group LLC -- Analyst
Perfect. Thank you.
Operator
And our next question comes from Tobey Sommer with SunTrust. Your line is now open.
Tobey Sommer -- SunTrust Robinson Humphrey -- Analyst
Thank you. With respect to your revised long-term forecast, could you talk about the — from a growth perspective, does that reflect what you think the market could offer you in terms of growth? Or are you planning or feeling to constrain it somehow for other reasons?
Scott Flanders -- Chief Executive Officer
Well, let me take it in two parts. I mean we thought it was incumbent upon us, Tobey, to revise our five-year plan. Given though we just first presented a five-year plan in May of last year, we have so outrun the tailwind case that we felt that it was meaningless to sell-side analysts as well as investors. And so that's what is driving the five-year plan revision.
The base case, in our mind, is a worst case, and the high case is not the highest case that management seeks to deliver. It's the high case that we wish to commit to. And so we do believe that the market could present greater opportunity than even the high case. Just to benchmark it for you, in terms of the macro environment, the base case is predicated upon an assumption that MA would be 49% of the total Medicare-eligible market in 2024, and that's assuming no expansion of age eligibility, which is in the Biden health plan to take Medicare down to age 60.
That's in no — none of our projections. The high case assumes what I believe is still conservative, what Humana would regard as conservative, is a 57% MA penetration by 2024. In terms of the deltas between the two, it's a $600 million difference between base case and high case. A lot of this is improved online.
We've got tremendous momentum in online and we — it's a fairly narrow range, but we assume that between assisted and unassisted, we'd be at 53% in 2024 in the base case and 57% combined in the high case. Embedded in that, however, is the unassisted, which has very high margins and very high persistency. And the base case is 17% of total enrollments online versus 21% total online in the high case. So we think that's imminently achievable.
We have 19 million unique visitors to our site, and we enrolled fewer than 100,000 online in the last 12 months. So it's a very low conversion rate. And what's significant that we didn't highlight significantly today because we wanted to spend a lot of time on the financial metrics and the persistency initiatives we had is this rapid momentum that we're experiencing in online and the fact that the Customer Center is really the tip of the iceberg in terms of the functionality and improved user experience that we're launching this year and even further improvements that are, right now, being engineered that we'll launch next year. And so we think that the most conservative piece of this plan is the financial leverage we're going to receive from our online consumer platform.
Tobey Sommer -- SunTrust Robinson Humphrey -- Analyst
If I could ask a follow-up, what does, in ranges or rough terms, the LTV look like for fully independent online enrollment versus online assist? Thank you.
Scott Flanders -- Chief Executive Officer
I'll punt that to Derek.
Derek Yung -- Chief Financial Officer
Yes. Tobey, we commented on that in our prepared remarks that the persistency, as we saw from the enrollments in AEP in 2019 for online enrollments, was about 25% to 30% better than telephonic enrollments, and that has a direct correlation to LTV differences.
Tobey Sommer -- SunTrust Robinson Humphrey -- Analyst
Thank you.
Operator
Our next question comes from Dave Styblo with Jefferies. Your line is now open.
Dave Styblo -- Jefferies -- Analyst
Good afternoon and thanks for the questions. I just wanted to explore a little bit more about the churn within the telephonic channel and better understand, as you guys look back through AEP and OEP, what was new and why did this suddenly happen? Do you think maybe it was a function of just the rapid growth and having to add so many new agents as you approved? Your approved count doubled in the fourth quarter. Or was there also some noise from the special enrollment period? Just curious, as you look back, are there learnings of, hey, maybe that growth was too aggressive and we had too many new folks in the door and how to use an outside vendor versus we need to change how that is next time? And then just maybe from a guidance perspective of what we should be thinking, how should we be thinking about the churn numbers in the third and fourth quarter? Are they going to stay elevated, do you think? Or should they start to improve now that things are starting to quiet down?
Scott Flanders -- Chief Executive Officer
Yes. Taking your last question first, we definitely expect churn to abate, Dave. But speaking to your first, I think you said it well that our growth goal was the No. 1 goal of the company.
My watchword was let's be effective first and we'll be efficient later. And we grew well ahead of our expectations and well ahead of our internal staffing, and we opened Indianapolis as a physical call center in just a year ago, was very successful for us last year in the AEP. But we still had more calls to answer, and that caused us to expand our third-party vendor agents. And again, what we've seen, and this is with the benefit of lag and a bit of hindsight, which I know you're not being critical, you're just asking, is that on that marginal vendor agent, we had elevated churn.
And so what you're seeing as we guide to the balance of the year, as we are slowing our growth rate down to almost half of what it was last year, you'll see that we're significantly increasing that mix of enrollments that will be closed and converted by our in-house agent. Another way to think about it, we have about 50% Medicare enrollment growth built into this guidance, which I note we believe to be conservative, on only a 37% total agent count increase. So that's just another way to do the math on the increased productivity that we're seeing and further expecting through the balance of the year.
Dave Styblo -- Jefferies -- Analyst
OK. Got it. And no real noise from the special enrollment period, Derek?
Scott Flanders -- Chief Executive Officer
Oh, a little. Derek, what would you say about that?
Derek Yung -- Chief Financial Officer
Yes. I mean, Dave, we did see enrollment volumes pick up a bit due to the special enrollment period but certainly nowhere near what we saw with the open enrollment period. So there is some marginal impact relative to revenue growth that we got from it but not significant, which also meant that what we observed in a market perspective, there are just fewer people looking to switch during that period.
Dave Styblo -- Jefferies -- Analyst
OK. And then just a follow-up would be on the longer-term outlook if we're looking out to that end year. I think in the past, you've given us some sense of what commissions receivable would look like at a specific level. Curious if you guys are willing to talk a little bit about that or the kind of the bars there.
And operating cash flow, obviously, you're talking about getting to that profitability. But again, sort of what that looks like from a numeric standpoint in the out year?
Scott Flanders -- Chief Executive Officer
Yes. Dave, it's about $2.5 billion in the base case and about $3 billion in the high case. That's with the conservative LTVs assumptions.
Dave Styblo -- Jefferies -- Analyst
$2.5 billion. Well, I'm talking about commissions receivable.
Scott Flanders -- Chief Executive Officer
That would be our balance, yes. At the end of 2024, we expect about a $2.5 billion commission receivable balance on our balance sheet on the base case, and Derek will correct me if I'm wrong, about $3 billion on the high case.
Dave Styblo -- Jefferies -- Analyst
Thank you.
Operator
And our next question comes from Jonathan Yong with Barclays. Your line is now open.
Jonathan Yong -- Barclays -- Analyst
Thanks, guys. Just going back to the LTV for a minute. I understand you guys are putting in all these initiatives to try to help improve the LTV, but traditionally, you've kind of told us and led us down the path of assume flat LTVs kind of moving forward. So I guess how much confidence do you have in improving the LTVs to get back to 2019 levels in 2021 given the elevated levels of churn that you're kind of experiencing now? Because my understanding is the more immediate churn levels have a bigger impact on LTV, so I just want to get some better understanding on that.
Scott Flanders -- Chief Executive Officer
Well, you're absolutely right that the churn has been driven by recent cohorts, and there is virtually no impairment to our commission receivable balance prior to three-year enrollments. But we have an extremely high level of confidence that we minimally get back to 2019 levels in 2021. The opportunity is much greater than that. Tim, perhaps you should express your level of confidence and the reason for that confidence.
Tim Hannan -- Chief Revenue Officer
Yes. I think that's right, Scott. We have very high confidence. I think as you described before, us slowing down our growth rate so we can handle our telephonic enrollments with our own internal agents, that is a big step in the right direction.
Then you layer on all of the additional initiatives that we're putting in place and grow the online component of enrollments. We feel very confident that there's upside beyond what we have there, but as a goal, getting back to the 2019 levels was what was appropriate for 2021.
Jonathan Yong -- Barclays -- Analyst
OK. And your comment about that the external telephonic agents were leading to higher churn, I mean, I guess given what you're doing with your internal agents, would it make more sense for you guys to add even more internal agents under your new compensation structure and not rely on the external agent structure? Just your thoughts on that. Thanks.
Scott Flanders -- Chief Executive Officer
Tim, I'll let you take it.
Tim Hannan -- Chief Revenue Officer
Sure. So I think that's where we're heading. I mean we're already shifting this year. We had never had any sizable remote workforce before March of this year, and we moved everyone to work from home in a matter of seven days.
And seeing how successful that was, it led us to be much more aggressive in recruiting our own remote workforce and give us a lot more flexibility in where we recruit from. That said, our vendor partners are an important part of our mix. There are many of those agents who perform on par with our internal agents. And as we get better at giving them tools, training, etc., they can do better.
They were just too large a part of our mix, and we do like the flexibility they provide us in ramping up in Q4. So I think going forward, we will have a more internally focused workforce but that our vendor partners will remain a part of that mix going forward.
Jonathan Yong -- Barclays -- Analyst
Thank you.
Operator
And our next question comes from Elizabeth Anderson with Evercore. Your line is now open.
Elizabeth Anderson -- Evercore ISI -- Analyst
Hi. Thanks for the question, guys. Can you just help me bridge the change in the cash flow guidance for the year and sort of talk about why you have increased confidence in the 2022 breakeven number?
Scott Flanders -- Chief Executive Officer
Derek?
Derek Yung -- Chief Financial Officer
Yes. On the change in the operating cash flow number guidance over guidance, there is a large portion of it, the majority, super majority of it is due to higher investments in sales and marketing to drive the additional revenue in the increased guidance. And just as a reminder, for our AEP enrollment, we incurred sales marketing expenses within the quarter, and typically, we do not receive any — the commissions related to those enrollments until Q1 the following year. There's also an increase in fixed cost guidance over guidance that's also built into operating cash flow and then between those 2 items that make up the difference.
Elizabeth Anderson -- Evercore ISI -- Analyst
Got it. OK. Thank you. That's very helpful.
Derek Yung -- Chief Financial Officer
And then just on your second part of your question in terms of our expectation, the current cash flow breakeven in 2022 under both the base case and tailwind, the high scenario and our revised long-range plan, given our unit economics, when growth rates stay flat or decline year over year, we do expect to turn cash flow positive by the third year. So based on why we're seeing where we'll end up this year, that tracks to that timing.
Elizabeth Anderson -- Evercore ISI -- Analyst
Great. Thank you.
Operator
Our next question comes from Greg Peters with Raymond James. Your line is now open.
Greg Peters -- Raymond James -- Analyst
Good afternoon. Thanks for squeezing me in. First question, with the movements in LTVs, I'm just curious why there wasn't any movement in your constraint assumptions.
Scott Flanders -- Chief Executive Officer
Derek?
Derek Yung -- Chief Financial Officer
Yes. So Greg, good question, and as a reminder, we apply a constraint of the lifetime value as a matter of conservatism to handle the volatility that we have seen in estimates from quarter-to-quarter as we move through the life of the cohorts of our Medicare members. And what you are seeing, Greg, is the constraint at work given that we have higher churn and expectations of LTV to decline is still within our constraint. So the constraint though is something that does get evaluated periodically to see whether the volatility has increased in a manner by which we need to update it.
And this quarter, that has not been necessary for Medicare, has not been necessary for Medicare.
Greg Peters -- Raymond James -- Analyst
OK. I'll take my follow-up on that offline. The second question I had, Scott, in your prepared comments, you mentioned the outlook for better Medicare revenue in the balance of the year. And with the recent IPOs of some of your competitors and Transact out there, I'm just curious if you feel like eHealth is getting as much financial support from the carrier partners as some of these competitors are.
Scott Flanders -- Chief Executive Officer
Well, the answer is we are not, and the reason is that we have a consumer-centric model, Greg, that does not direct seniors to specific carriers the way that some of our competitors constrain their carrier choice. And both models are viable. We still receive substantial support from most of the major carriers, a majority of them, but we could receive greater advertising support if we were to constrain the consumer offerings. But that's not our model.
I mean we're consumer centric, and we want to put the seniors in the very best plan for them.
Greg Peters -- Raymond James -- Analyst
Right. And then so just trying to reconcile that with your comment about better Medicare revenue in the back half of the year, where's...
Scott Flanders -- Chief Executive Officer
Greg, I understand. We're expecting our advertising revenue to nearly double this year while our enrollments and commissions are not doubling. So it's growing as — it's growing faster, the carrier support, as evidenced by the advertising dollars, is growing at a much faster rate than the underlying business this year.
Greg Peters -- Raymond James -- Analyst
Got it. Thanks for the answers.
Operator
Our next question comes from George Hill with Deutsche Bank. Your line is now open.
George Hill -- Deutsche Bank -- Analyst
Hey. Good afternoon, guys, and thanks for taking the questions. I guess, Scott, I'm going to ask the churn question in a different way, which is can you talk about any initiatives around brand building and such that when members churn, they continue to come back to eHealth to make sure that they're making their carrier selection. And then I have a quick follow-up for Derek.
Scott Flanders -- Chief Executive Officer
Yes. So we under-index other e-commerce businesses with recapturing the churning member. Right now we recapture only 10% of the seniors that churn out of our book, which is very low, especially considering that these seniors, unless they pass away, are enrolling in another Medicare Advantage plan almost certainly, well over 95%. And part of the Customer Center technology that we're launching in September will enable us to have continual online engagement, be able to submit updates as different plans change.
And so we do know that we have to make this a bigger priority. It hasn't been. We have been transaction oriented. We've not been retention oriented, and we've not been recapture oriented.
And just as we achieved our plans that we set out to grow fast over the last 2 years, we will achieve our plans now that we've set to improve, recapture and retention.
George Hill -- Deutsche Bank -- Analyst
OK. Thanks. And then maybe the quick follow-up for Derek. And Derek, this is a follow-up on Elizabeth's question, is what I'm trying to understand is you guys have kind of raised the revenue guide, the EBITDA guide, the GAAP income guide, but the cash flow guide is going the wrong way.
I guess just a little bit more of the crosswalk there because I would have expected that if the GAAP net income guide was going up, the cash flow guide would go positive. Are you guys capitalizing some of the SG&A expense? Is this just the timing between kind of receivables and payables? I'm just trying to — like it's probably — maybe it's better taken offline, but I just kind of wanted a more detailed walk-through if you're willing to do it.
Derek Yung -- Chief Financial Officer
Yes. Well, I can give just a bit more precision to expand on that since you're asking as well. So I think for guidance over guidance, the operating cash flow breakeven is about another $27 million loss, right? And then of that, about $19.5 million of it is related to higher sales and marketing expenses to drive AEP enrollments, and then there's another about $4 million and $5 million — $4 million to $5 million of increased fixed costs. So that gets you almost all the way there in terms of the guidance-over-guidance difference.
George Hill -- Deutsche Bank -- Analyst
OK. I think I have a couple more questions, but I'm happy to follow up offline. Thank you.
Operator
Our next question comes from Frank Morgan with RBC Capital Markets. Your line is now open.
Frank Morgan -- RBC Capital Markets -- Analyst
Thank you. I guess, first, a clarification. I wanted to go back to Dave's earlier question about your answer to make sure I understood. You said you thought that churn would moderate both in the third and fourth quarter, so if we're looking at this 42% number in the second quarter, you're saying that, that number on the third and fourth quarter will go down.
So that's my clarification first.
Scott Flanders -- Chief Executive Officer
That's my belief, Frank. Derek?
Derek Yung -- Chief Financial Officer
Yes. Frank, the increase in that particular metric is a combination of what we have commented on in terms of increase in churn in the cohorts that newly enrolled and also adding a larger number of members into our overall membership base. And older members churn at much lower rates, so when you are at a larger share of new members and member base, it will drive the number up. And since our Q3 enrollments are typically lower, it will bring that percentage down.
That would be our expectation.
Frank Morgan -- RBC Capital Markets -- Analyst
Got you. And then I know in the very opening remarks, you commented that it was really industry/macro factors along with company-specific factors, but it really sounds like it's more of a — just to clarify, more company specific. Would you care to attribute a weighting to how much do you think that this is company specific and within your control versus how much of this is an industry issue?
Scott Flanders -- Chief Executive Officer
Look, we can't be precise about it, but as Tim said, Frank, did bring third-party consultants in. And it's their view that the macro factor is only about 100 basis points. My gut tells me that it's more than that. But they believe that well over 90% of the elevated churn is addressable by specific operating initiatives that we've already launched that will have impact this fall.
Tim, what's your reaction?
Tim Hannan -- Chief Revenue Officer
Yes. I would just phrase it a little bit differently. I think the macro environments mean we pay more significant price for our deficiencies. So where customers have more plans to choose from and more opportunities to switch, if we don't do a good job in the sales process and we don't follow up effectively, then they will switch at higher rates in a way they may not have in previous years.
So I do believe it is exacerbated by the macro factors but that it is primarily driven by elements that we control.
Frank Morgan -- RBC Capital Markets -- Analyst
Thank you. And then in terms of the mix of internal versus vendor agents going into this AEP, obviously, it sounds like that's a big part of the problem. So what will that mix look like? And how has that changed between internal and vendor?
Scott Flanders -- Chief Executive Officer
Right. We were about 70% at peak last year third-party external agents, and this year, that number will be well under 60%. And that really understates it as well because that's just raw numbers. We will be allocating more calls to internal agents because we've grown our internal sales force faster than our external sales force.
Frank Morgan -- RBC Capital Markets -- Analyst
OK. Thank you.
Operator
Our next question comes from Stephen Tanal with SVB Leerink. Your line is now open.
Stephen Tanal -- SVB Leerink Partners -- Analyst
Hey. Good afternoon, guys. Thanks for taking my questions. I just wanted to follow up on two areas that we've been talking about here today, MA LTV and then online persistency as well as cash needs.
So I appreciate that one of the drivers of getting LTV back to 2019 levels is the higher persistency of online enrollees. But do you feel you have enough of a sample size of those numbers at this point that have sort of been with you for more than, let's say, three years or so built into the overall MA LTV to know for sure that their duration is longer? Maybe like what percent or maybe a number that's past that mark would be helpful. And kind of like related to this, you mentioned in the 2019 AEP the online enrollees are 25% to 30% higher than telephonic on persistency, but I guess I just want to better understand that as well. Like how do you measure that when you're a few quarters out from AEP? Just would be helpful to understand.
Scott Flanders -- Chief Executive Officer
Tim?
Tim Hannan -- Chief Revenue Officer
Yes. The big difference among these enrollees and where we're focusing our attention is in basically short-term retention. So those that go approved that either don't go paid or only go paid for a short amount of time and then switch, so we do have a great deal of visibility into how that is playing out. In terms of long-term history on online enrollments, I do think we have a sufficient sample size, and I'd turn to Derek for that one for any additional commentary.
Derek Yung -- Chief Financial Officer
We do. So yes, so we have observed a spread, a difference between online persistency versus telephonic persistency the last four years. What we have also noticed is that spread has increased significantly this year on the telephonic side getting worse. So — and yes.
while it's still a small percentage of overall enrollments, we are tracking to a number of hundreds of thousands of enrollees here. So from a statistic significance perspective, it's meaningful. And maybe one more thing to add too is the reason why we can confidently articulate the trend for the cohorts that just enroll in AEP is the first 90, 100 days of churn for first year enrollment makes up for almost the entirety of churn for almost a whole year. So that's a dynamic that — with every new enrollments, not just with eHealth.
So we have been looking at that on a post-100-day basis, and we've seen this trend enable to describe it and identify it.
Stephen Tanal -- SVB Leerink Partners -- Analyst
Great. That's super helpful. And then maybe just to follow up on the cash side. The midpoint of 2020 guidance suggests the operating cash and capex will be a use of about $114 million at the midpoint, and looking at that number for the first half.
It's about $17 million, so the implied cash needs for the back half or something in the order of $97 million, again to 2Q around $77 million. So am I missing anything major there? And if not, how do you guys plan to fund the difference? And I guess, thinking about your preferred cash cycle kind of Q1 to Q1, do you expect those have to be positive through the 12 months through Q1 '21? And any thoughts there?
Derek Yung -- Chief Financial Officer
Yes. So I do not expect us to be cash flow positive in Q1 '21, although that is the better cash cycle to look at than the fiscal year one, so you're correct on that because we get so much of cash collections in Q1 from MA enrollees, which we typically get all the annual commissions in Q1. In terms of funding, obviously, we have access to capital from the equity raise in March and the intention from doing that raise was to drive more growth in Q4, and that's what you're seeing here. The other thing is, as Scott commented on, is we are seeing a disproportionately higher growth in carrier advertising revenue, which is cash that we get in year, which we will look to redeploy to sales and marketing investments, which will help our back half of the year in terms of cash flow.
Stephen Tanal -- SVB Leerink Partners -- Analyst
Thank you.
Operator
Our next question comes from Daniel Grosslight with Citi. Your line is now open.
Daniel Grosslight -- Citi -- Analyst
Hey, guys. Thanks for taking the question. I want to go back to that 10% recapture rate. How high do you think you can drive that in the next three to four years? And when folks are churning off of eHealth, do you have any data on where they're going? Are they going to other DTC platforms? Are they going directly to the carrier? How does that kind of flow through the system?
Scott Flanders -- Chief Executive Officer
Yes. So last first, it's both, and we're losing to the other direct-to-consumer brokers as well as some seniors convert to plans on a carrier platform and then we're no longer broker of record. We have a conservative forecast here. In both the base case and the high case, we are only assuming we reach a 20% recapture rate.
That is very likely to prove low with the Customer Center that we're launching and increased retention team, etc. We think that, that is the bare minimum to achieve over the next — we probably ought to double it in the next two years. But for the conservatism of the plan, we just assumed that it could double. Tim, would you add more to that?
Tim Hannan -- Chief Revenue Officer
Sure. Well, I think the main point I would make is our 10% recapture rate now is essentially driven by us reacquiring a customer. So we don't have a significant retention effort, which is why we think there's so much opportunity here. So we're recapturing these people because they call back in.
They might have an email. They see a TV ad. It's a function of our transaction growth, not a function of any designated retention efforts. So as we get better at communicating with them, following up with them, making better recommendations to them, just having a better sales process, we can do significantly better than 10%.
And I think the 20% that Scott mentioned is conservative.
Daniel Grosslight -- Citi -- Analyst
Got it. Thanks. And maybe just one follow-up. As you look to recruit and hire more internal agents, obviously, there's a finite pool of productive agents out there.
Now you have a bunch of folks competing for them, both from the well-capitalized peers and the carriers you're moving more toward the telephonic channel. Do you see recruitment as an increasing challenge because of the increasingly competitive environment? And do you think you'll have to really boost up salaries to compete here?
Scott Flanders -- Chief Executive Officer
No. I don't think so. We're highly competitive on both base salaries as well as commission bonus opportunities, and we are industry leading in terms of medical and other benefits. Look, this is a very big country, and there are a lot of eligible candidates for these roles.
We're also quite nicely geographically distributed in our physical call centers. And now with work-from-home capability, we're not even limited to our geographic footprint. And so anecdotally, as I talk to our peer competitors and we are all friendly competitors, none of us are having a hard time. Admittedly, we've benefited from the unfortunate unemployment levels that have probably caused this year to be an easier year for recruitment than what hopefully next year will be.
But we think the pool of college graduates, people with sales experience that are attracted to these jobs, that offer a great deal of independence, the opportunity to help seniors a lot, there's a lot of personal satisfaction, and there's a real opportunity, double-digit percentage of our agents make into the six figures. So we think we can continue to increase the share of enrollments that we drive from internal agents, while we are also even more significantly increasing the share that we enroll online.
Daniel Grosslight -- Citi -- Analyst
Thank you.
Operator
And I'm showing no further questions in the queue at this time. I'd like to turn the call back to speakers for any closing remarks.
Scott Flanders -- Chief Executive Officer
Well, I know we've gone over. I thank you all for your well-considered questions. We look very forward to the balance of this year and delivering very exciting results for our consumers and our shareholders. Thank you.
Operator
[Operator signoff]
Duration: 83 minutes
Call participants:
Kate Sidorovich -- Vice President of Investor Relations
Scott Flanders -- Chief Executive Officer
Tim Hannan -- Chief Revenue Officer
Derek Yung -- Chief Financial Officer
Jailendra Singh -- Credit Suisse -- Analyst
George Sutton -- Craig-Hallum Capital Group LLC -- Analyst
Tobey Sommer -- SunTrust Robinson Humphrey -- Analyst
Dave Styblo -- Jefferies -- Analyst
Jonathan Yong -- Barclays -- Analyst
Elizabeth Anderson -- Evercore ISI -- Analyst
Greg Peters -- Raymond James -- Analyst
George Hill -- Deutsche Bank -- Analyst
Frank Morgan -- RBC Capital Markets -- Analyst
Stephen Tanal -- SVB Leerink Partners -- Analyst
Daniel Grosslight -- Citi -- Analyst