Image source: The Motley Fool.
Amedisys, inc (AMED -0.42%)
Q3 2021 Earnings Call
Nov 3, 2021, 11:00 a.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Greetings, and welcome to the Amedisys Third Quarter 2021 Earnings Conference Call. [Operator Instructions] As a reminder, this conference is being recorded. It is now my pleasure to introduce your host, Nick Muscato, Senior Vice President of Finance. Thank you. Please go ahead.
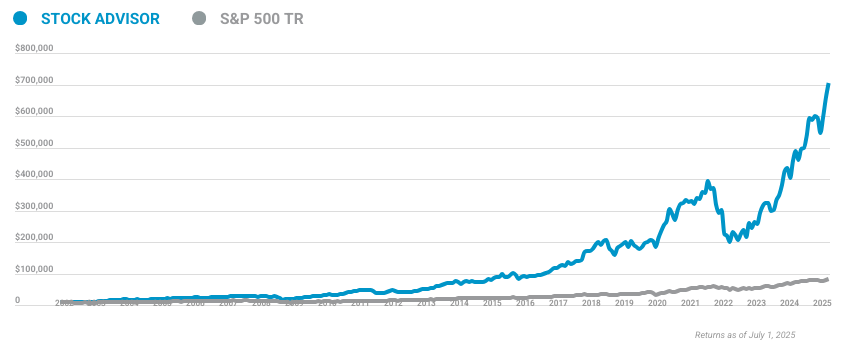
10 stocks we like better than Amedisys
When our award-winning analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Amedisys wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of October 20, 2021
Nick Muscato -- Senior Vice President of Finance
Thank you, operator, and welcome to the Amedisys investor conference call to discuss the results of the third quarter ended September 30, 2021. A copy of our press release, supplemental slides and related Form 8-K filing with the SEC are available on the Investor Relations page of our website. Speaking on today's call from Amedisys will be Paul Kusserow, Chairman and Chief Executive Officer; Chris Gerard, President and Chief Operating Officer; and Scott Ginn, Executive Vice President and Chief Financial Officer. Also joining us is Dave Kemmerly, Chief Legal and Government Affairs Officer. Before we get started with our call, I would like to remind everyone that statements made on this conference call today may constitute forward-looking statements and are protected under the safe harbor of the Private Securities Litigation Reform Act. These forward-looking statements are based on information available to Amedisys today. The company assumes no obligation to update information provided on this call to reflect subsequent events other than as required under applicable securities laws. These forward-looking statements may involve a number of risks and uncertainties, which may cause the company's results or actual outcomes to differ materially from such statements. These risks and uncertainties include factors detailed in our SEC filings including our Forms 10-K, 10-Q and 8-K. In addition, as required by SEC Regulation G, a reconciliation of any non-GAAP measures mentioned during our call today to the most comparable GAAP measures will also be available in our Forms 10-K, 10-Q and 8-K. Thank you. And now, I'll turn the call over to Amedisys' Chairman and CEO, Paul Kusserow.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Thanks, Nick, and welcome to the Amedisys 2021 Third Quarter Earnings Call. We have a lot to discuss on today's call. But before we dive in, I want to express my sincerest appreciation to all 21,000 plus Amedisys employees. Whether you are at a patient's bedside or supporting those providing the industry's best in class care, at Amedisys, we put quality before everything. And the unwavering dedication of our entire employee base has been delivering great patient care and this dedication to quality continues to be my greatest point of pride and largest source of inspiration. COVID-19 continues to change the dynamics of all of healthcare and how it is provided, yet you all remain resolute in putting patients first and delivering industry-leading metrics. For that, I thank you. Before I turn the call over to Chris and Scott, I'd like to say how proud and excited I am by our performance. This has been a tough, if not brutal year. The incoming that's come at us, we could not have imagined. I have a favorite quote from Teddy Roosevelt, which best describes how we are dealing with the COVID era: "Do what you can with what you have, where you are." I've modified it a bit for us: Do the best you can with all you have, hold strong and take ground. That's our motto. Amedisys did all that and more. A good company maximizes on what it can control. A great company responds to uncontrollable forces better than everyone else, and where possible, turns them into opportunities.
For controllables, we built up our BD heads, we reduced our clinical turnover by 15%, we saw the labor issues in our industry and accelerated recruiting, increasing our hiring 40%. And we kept driving our quality ratings higher, 4.6 STARS by our latest estimate. What we can't control is accelerated death rates due to COVID, hospitals closing units due to labor shortages, hospitals cutting electives to make room for COVID beds, nurses out on quarantine due to COVID, and clinicians choosing not to be vaccinated. In hospice, there's faster death rates due to COVID, which is affecting our ADC, but we're taking share and we're growing admissions. Our admissions are up when others are down. When ADC normalizes, which we're just starting to see signs of now, our revenue will grow at rates we have typically seen. In home health, we lost visits due to quarantine clinicians and hospitals cutting back on electives, but we again gained share and managed to grow. These results are hard fought and hard won. We are a company that wins on controllables and pivots best on uncontrollables. Can we do better? We always try to. Have we made mistakes? Absolutely. But so far, it's been a remarkable year of performance in a tremendously turbulent time. Now I'd like to discuss Contessa's performance during the quarter. Our newly formed high acuity care segment, or Contessa, experienced continued positive momentum in Q3, offering home-based recovery solutions for patients in need of acute level care. Total admissions were 234 for the two months since the closing of the acquisition, an increase of 8.3% from our original forecast, pretty good for a company that joined us just two months ago. Demand for home-based acute services is extremely high across Contessa's existing joint venture markets and continues to grow. We are working with Contessa's leadership team to think through innovative ways to access more home nursing so that they can continue to capitalize and capture on this demand. The results so far are very promising as we have largely eliminated all of their vacancies. Contessa continue to demonstrate its ability to drive value to marquee health systems with the closing of its joint venture with the Henry Ford Health System. This partnership, which is expected to launch in Q4 '21, will combine all three Contessa clinical models, including hospital at home, SNF at home, and palliative level care in the home. In addition to the Henry Ford partnership, Contessa just inked another substantial deal we'll be announcing in a week or so, and is actively evaluating partnerships with 13 additional health systems.
This will create an opportunity to more than double its footprint. In terms of partnerships in operation, we're way ahead of our growth goals for 2021 and 2022, which is very encouraging. Finally, Contessa continues to add payer sources, thus increasing our market's total addressable lives with the addition of the Medicare fee for service waiver in two markets, while also finalizing managed care contracts for the SNF and palliative clinical models in various markets. We are very pleased with the High Acuity segment's performance, and we are excited by the new opportunities and capabilities Contessa brings to the table, namely the ability to take care of sicker and more acutely ill patients in the home, the ability to provide this care taking full risk, and having the ability to incorporate and coordinate all this multiplicity of care across a single platform. We have doubled our addressable markets with Contessa's capabilities, and we can drive better profits for our hospital and payer partners in these arrangements and deliver better outcomes and higher satisfaction to patients who want hospital and SNF level care in the home at a lower cost. I'd like to thank and congratulate our Contessa partners on the great start. Before I turn it over to Chris, I'd like to note that as of the timing of the recording of our prepared remarks, the final 2022 home health reimbursement update has not been released. Though we do not expect much, if there is any deviation from the proposed rule, upon the final rules released, we will analyze the Amedisys specific impact and update everyone accordingly. I'll now turn the call over to Chris to give us a rundown of our core business performance during the quarter. Chris?
Christopher T. Gerard -- President and Chief Operating Officer
Thanks, Paul. Before we get into our segment level results, I want to review how much the operating environment has changed as we exited the second quarter and contrast that with the operating environment today. As we exited the second quarter, elective procedures as a percent of our total episodes had recovered to 7.5% compared to 9% of total episodes pre-COVID. We made no assumption about improvements in this number in our revised guidance per Q2 call. The percentage of our clinicians on quarantine had dropped to 0.7%. In hospice, our average discharge length of stay was 96.8 days, and our median length of stay was 25.3 days, and there was no conversation about a vaccine mandate. And we were only seeing labor pressures in certain pockets of our footprint. As we report our Q3 earnings today, here's how the environment has changed. Elective procedures as a percent of our total episodes dropped from 7.5% in Q2 to 6.5% in Q3. Electives are now starting to come back slightly, which is encouraging. The percentage of our clinicians on quarantine reached 3%, up from 0.7% in Q2. The number of clinicians on quarantine has peaked, and entering Q4, we're seeing the number decline rapidly to less than 1%, which is also encouraging. Our hospice discharge average length of stay fell to 94.5 days from 96.8 days, and median length of stay dropped to 24.3 days from 25.3 days. These decreases were driven by an increased percentage of death on census. We're encouraged that we are seeing early signs of this rebounding. The proposed vaccine mandate was released, and we started to see some systemwide labor and wage pressures. But being named a great place to work by Modern Healthcare and intensely focusing on our people, our labor issues are not as bad as others are seeing. As you can see, the environment remains very fluid and hard to predict with significant levels of accuracy. Though COVID continues to impact our business, I, like Paul, am very pleased with how we have continued to make forward progress during this turbulent time. We've got good metal. Now let's dig into our Q3 home health segment performance. Home health grew total admissions and total volume by 1%. As I discussed, home health growth was impacted during the quarter by a decrease in elective procedures and an increase in the number of clinicians on quarantine, which led to an increase of nearly 3,700 missed total admissions or an anticipated missed growth opportunity of 4%.
For the quarter, we performed 13.8 visits per episode, down 0.4 visits sequentially and down 0.6 visits year over year. We remain very comfortable with our VPE levels as we've seen strong increases in our quality scores by our estimates, now 4.6 STARS. As a reminder, we consistently stated we will never do anything to impact quality scores. And given our continued improvement in home health quality scores, along with our decreased visits per episode, we are delivering on that promise. On clinical mix, in Q3, we achieved 47.9% LPN utilization and 53.3% PTA utilization, both at the highest levels since the start of PDGM. Clinician turnover has declined year over year by 15%. We're pushing to do better as we continue to steal market share, and we need to retain and grow our clinical labor force to service increased levels of demand. Now moving on to hospice. For the quarter, we grew Hospice total admits by 1% over a 9% Q3 '20 comp and ADC was down 5%. As we discussed last quarter, the drop off in hospice growth had been largely driven by turnover in our BD staff. We knew that hiring and retention were activities in our control, and as such, we outlined a plan to recover the staff and have executed upon it. During the quarter, we added 39 BD FTEs and ended the quarter with 523 hospice BD FTEs. We continue to work toward exiting the year over 550 hospice BD FTEs and have another 19 hospice BD FTEs that have accepted offers that will be starting in the coming weeks. Very encouraging. What we're not seeing recover completely, but are starting to see some hopeful signs, is hospice ADC. Despite a 5% sequential increase in admissions due to a continued increase in deaths on census, which is reflected in the drop in our average length of stay and medium length of stay, our ADC has declined. Year over year, deaths on census has increased 8%.
This is another uncontrollable COVID impact as patients are entering our hospice care much later in the dying process and staying on service for a shorter length of time. The increase of deaths on census is materially impactful to the hospice segment performance as a 1% change in discharge rate is equivalent to approximately 130 ADC, which over the quarter, would have added to, added approximately $2 million to the bottom line. Though predicting behavior is more an art than science, we do think that the increased death rate is a short term issue, and over time, will return to normal. Whenever behavior returns to pre-COVID normal and patients access healthcare like they did pre pandemic, we will see ADC increase. And as we continue to hire and retain our BD staff and grow admissions, ADC growth will follow. In summary, both home health and hospice continue to be impacted by COVID-19 issues and their subsequent shake out. Many challenges presented in our current operating environment are out of our control, but we've pivoted quickly. Those issues that are within our control have been systematically evaluated and quickly embraced by our teams as a new reality. The results we have delivered in spite of these challenges, I'm proud of. Our teams, for what they have accomplished and will accomplish, is extraordinary, and none of us will truly be satisfied until we return to the growth levels our company is used to delivering. Pre-COVID norms or new norms, either way, we will deliver. With that, I'll turn it over to Scott, who will take us through a more detailed review of our financial performance for the quarter and our projections for the remainder of the year.
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
Thanks, Chris. For the third quarter of 2021 on a GAAP basis, we delivered net income of $1.37 per diluted share on $554 million in revenue, a revenue increase of $9 million or 2% compared to 2020. During the quarter, we did not have any CARES Act funds available to offset increased costs related to COVID-19 due to the expiration of the use of provider relief funds on June 30. For the quarter, our results were impacted by income or expense items adjusting our GAAP results that we have characterized as non core, temporary or one time in nature. slide 14 of our supplemental slides provides detail regarding these items and the income statement line items each adjustment impacts. In previous quarters, these adjustments included both the provider relief funds and COVID-19-related costs. With the expiration of provider relief funds, only COVID-19-related costs are included as adjustments. For the third quarter, on an adjusted basis, our results were as follows: revenue grew $9 million or 2% to $554 million. EBITDA decreased $3 million or 4% to $72 million. The acquisition of Contessa drove the decline over prior year as our legacy EBITDA was flat. EBITDA as a percentage of revenue decreased 80 basis points to 13.1% and EPS decreased $0.71 or 32% to $1.53 per share. As a reminder, adjusted EPS was positively impacted in Q3 2020 by a $0.72 income tax benefit related to an executive stock option exercise. The continuation of the COVID-19 pandemic, in particular, the surge in cases during Q3 related to the Delta variant, impacted volumes, hospice, discharge rates and labor costs. We estimate the impact to our financial results were as follows: Our home health volumes were impacted by decrease in elective procedures and an increase in clinicians quarantine, which resulted in a loss of 3,700 emissions, resulting in an approximate $2 million impact to EBITDA. In hospice, the discharge rate for Q3 was 2.4% higher than our expectations, as the rate was significantly higher than our already elevated 2020 rates, which impacted EBITDA by approximately $4 million. The lower ADC has resulted in numerous care centers having unused capacity based on our staffing model. The cost of maintaining this level of staffing and anticipation of normalization and discharge rates is approximately $3 million.
And both home health and hospice combined for additional raises, final and retention bonuses, which added $2 million to the quarter. Now turning to our third quarter adjusted segment performance. Keep in mind, segment level EBITDA is pre-corporate allocation. In home health, revenue was $339 million, up $13 million or 4% compared to prior year. Revenue per episode was up $83 or 3%. The increase in revenue per episode is a result of a 1.9% increase in reimbursement, an increase in the functional impairment of our patients, and a change in the source and timing and geographic dispersion of our patients. Our implementation of Medalogix Care has led to a reduction of 0.6 visits per episode, while we continue to improve on our quality scores. Overall, our business per episode is down two visits since Q1 2020. Our gross margin decreased 90 basis points as a result of a 6% increase in cost per visit. The increase in cost per visit was driven by planned wage increases, an increase in new hire pay, a significant increase in the utilization and rates of contract clinicians driven by growth in COVID-19, and higher health insurance costs. G&A increased approximately $4 million, mainly driven by lower spend in Q3 2020 related to COVID-19, raises the addition of resources to support growth and higher recruiting fees, which was partially offset by lower incentive comp. Segment EBITDA was $68 million with an EBITDA margin of 20.2%, which is down from 21.3% in 2020. Our 3% increase in revenue per episode and the decrease in business per episode were not enough to overcome labor pressures. Sequentially, segment EBITDA was down $11 million on lower admissions and an increase in cost per visit, which was driven by raises, new hire pay and an additional holiday. Now turning to our hospice segment results. For the third quarter, revenue was $198 million, down $2 million over prior year.
Net revenue per day was up 4%, driven by a 2.4% hospice rate increase that went to effect October 1, 2020. As Chris discussed, hospital admissions grew 1% and ADC declined 5% as COVID-19 continues to accelerate hospice discharge rates. Hospice cost per day increased $7.14, primarily due to planned raises, additional retention raises, hiring and retention bonuses, higher utilization of contractors, higher business performed by hourly employees as prior year was impacted by access restrictions due to COVID, and higher transportation costs. EBITDA was $42 million, down approximately $8 million. G&A increased $2 million due to planned wage increases, additional business development resources, higher recruiting fees and higher travel costs. Sequentially, admissions increased 5% with ADC remaining relatively flat due to higher discharge rates. Segment EBITDA increased $2 million, primarily due to lower revenue adjustments offset by annual raises as well as additional bonuses and raises to increase employee retention. Turning to our total general and administrative expenses. On an adjusted basis, total G&A was $176 million or 31.8% of total revenue was decreased 50 basis points over prior year. Sequentially, G&A is up $5 million, of which $4 million is due to the addition of Contessa. We continue to generate impressive cash flow in the third quarter, producing $62 million in cash flow from operations. Year-over-year, our DSO increased 3.5 days, driven by the elimination of RAP payment effective 1/1/21. As a result of our continued strong cash flow, our net leverage ratio at the end of the quarter was 1.2 times, inclusive of the funding of the Contessa acquisition. As a reminder, our Q4 cash flow from operations will be impacted by approximately $28 million due to repayment of deferred payroll taxes. Turning to M&A. We closed on the certificate need purchase expanding our home health services in Charlotte and Raleigh, North Carolina. These two care centers will essentially be de novos that will ramp in size and profitability throughout 2022. We continue to focus on our inorganic growth efforts on home health acquisitions and continue to work assets through various stages of diligence. Though industry consolidation has not happened as we originally expected in 2021 due to the extension of sequestration and CARES Act funds, we believe that M&A activity will pick up as we enter 2022, and Amedisys remains well positioned to capitalize on inorganic growth opportunities.
As you can see on page 16 of our supplemental slide deck, we are updating our guidance ranges for 2021. This updated guide reflects the impact of the Delta variant in our Q3 volumes which will carry over to Q4 along with accelerated labor pressures. Our guidance ranges are adjusted revenue of $2.2 billion to $2.05 billion, adjusted EBITDA of $296 million to $298 million, and adjusted EPS of $5.88 to $5.93. The emergence of the Delta variant in Q3 significantly changed our view on the remainder of the year versus our expectations coming out of Q2. As such, COVID-19 continues to impact the operating metrics typically used to forecast growth and cost assumptions for both core Amedisys and Contessa. We're basing our guidance on our current operating environment. Any future regulations or government interventions, spike in clinicians and BD staff in quarantine, unforeseen impacts of the vaccine mandate, reduction in elective procedures, change in patient behavior and further decline in senior living occupancy could impact our ability to achieve this guidance. Some of the items impacting our sequential performance from Q3 to Q4 are as follows: a full quarter of Contessa ownership will impact performance by $2 million. Health insurance cost increases of approximately $6 million. While there is a seasonality impact, Q4 2021 is elevated due to lower than expected Q3 claims. An additional month of raises adds approximately $2 million in costs. Finally, I'd like to reiterate the tailwinds and headwinds that impact our 2022 outlook. Positive rate updates in both home health and hospice offset the impact of the expiration of sequestration relief and leaves us in a modeling net positive position. Incremental EBITDA impact of Contessa which will be approximately $10 million, continued wage pressures, normalization of growth rates and the impact on hospice as length of stay recovers and COVID-19 costs, which have been covered by CARES Act funds through Q2 2021.
Though there are headwinds facing us until we enter 2022, we are optimistic that we can grow EBITDA as our investment in business development resources mature, and we continue our focus on being an efficient provider of high quality care. Additionally, we remain confident in our ability to deliver on our M&A strategy. However, we do not believe that current Street consensus for 2022 properly reflects the impact of the surges of COVID-19 in Q3 and which has brought additional uncertainty to the timing of hospice length stay recovery and given the realtime changing labor dynamics. We will continue to provide color on 2022 as we see trends change. I'll now turn the call back over to Paul to conclude. Paul?
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Thanks, Scott. As you can see, we effectively fought and muscled our way through another very turbulent quarter as the effects of COVID-19 continued to manifest themselves in new and unpredictable ways. As we enter what, to date, is looking like a calmer Q4 and look toward 2022, we are acutely focused on driving consistent growth. We recognize we cannot control the death and discharge rates in hospice nor can we control the pressures on the U.S. nursing workforce from the great resignation as well as clinicians who choose not to be vaccinated. What we can do is to think differently, act definitively and continue to innovate to maximize our clinical capacity, attract new nurses to home health and hospice and retain our hard to find clinical staff. We have assembled a differentiated group of assets within Amedisys, and we'll continue to look for new ways to deploy all of these lines of business as we continue to disrupt and expand the traditional ways care is delivered in the home. The short term headwinds currently beating at us have changed nothing about the long term tailwinds that Amedisys is advantageously set up to capitalize on. These include: demographics, which are strongly in our favor with the baby boomers, creating a potential surge of patients in the coming year with more people turning 65 years old than ever before. The outsized growth in the 70 plus market, coupled with an ever-increasing unsustainable healthcare costs, put us in a very advantageous position as a differentiated at home aging in place company, delivering the highest quality of comprehensive care at the lowest cost to seniors. Next, psychographics. With nine out of 10 baby boomers wanting to age and die at home, we, as the industry leader in quality with national scale and the most comprehensive offerings, are best positioned to serve these patients who want to age in place. Regulatory. As we discussed earlier in the call, we have positive rate updates in both home health and hospice. This is a trend that we see continuing for the next five plus years. Market share. Though consolidation has been slow to occur, our annual cash flow, low leverage and scale put us in a better position than any company in our space to consolidate our highly fragmented industries, and we expect to continue to capture and grow our market share inorganically in 2022 and beyond as the effects of PDGM and regulatory reform kick in for real. And finally, our unique and diversified asset base, including home health, hospice, personal care and Contessa. Hospital at home, SNF at home, palliative at home and primary care at home have strategically differentiated Amedisys from the rest of the industry. Our goal has always been to drive innovation into care in the home, and Amedisys now sits poised to change the game. We will continue to take steps toward higher acuity in home, risk taking care models and comprehensive care platforms to drive innovation in both how we provide care and how we are reimbursed for it. Where there's change, there's opportunity. These are exciting times. This ends our prepared remarks. Operator, please open the line for questions.
Questions and Answers:
Operator
[Operator Instructions] Our first question is coming from Brian Tanquilut of Jefferies.
Brian Tanquilut -- Jefferies -- Analyst
My first question, just for Scott. So as we think about the guidance adjustment, right? So I get that top line was challenging during the quarter. But maybe you can walk us through how you're thinking about the bridge from maybe the old guidance to the new guidance, some of the moving parts? And any incremental expenses that you would call out? And also kind of like the stage off point going from Q4 into next year, I mean you called out positive EBITDA growth expectation for next year. Maybe like anything you can walk us through in terms of the operational side of that? How do you gain confidence that you can grow EBITDA in 2022?
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
Sure, Brian. I think some of the, just to kind of starting with your first question around change in our update to our guidance. I think clearly, and as we called out in some of our prepared comments, the impact to hospice discharge rates would be the biggest issue that really flows through it. As hospice goes, being off of 2.4% on a higher discharge rate, higher than we even saw in 2020. It was a $4 million impact to EBITDA, which is pretty close to what the revenue drive, impact was because most of that's on a fixed cost basis. So that feeds into Q4. So that's moving over there. Chris had highlighted the fact that we missed out on roughly 3,700 admits. That's probably another $2 million-ish in EBITDA and another, if you think about somewhere around four-ish in, let's call it, in revenue. So all of those feed into Q4. That's one thing that every quarter builds on each quarter from us from a census perspective. It matters very much how we end each quarter. So that's kind of the pressure moving forward that kind of propelled this kind of adjustment to Q4 and where we ended from a census perspective. Still saw nice sequential increases in hospice from Q2 to Q3 from an admin perspective at plus 5%, but just barely grew census. So not really enough to meet where we thought we would be heading in out of Q2, so to speak. If we, thinking about coming from Q3 to Q4, just to resummarize that, there's really three issues that are really driving that number, that $6 million in health insurance costs and some of that's elevated because Q3 has Delta impacted most of our business. It also probably impacted that claims activity as well. So there's another $6 million incremental going from Q3 to Q4. As I said, $2 million, Contessa. We're happy with Contessa's EBITDA. They're slightly better than we thought, but there will be another $2 million drag on our performance into Q4. And then $2 million for a full quarter of raises, Q3 only has two months. So if you look at that number, the implied guidance gets you from an EBITDA perspective, Brian, somewhere around 62-ish or 63-type number. And health insurance is still large. So when I look at that number versus using a 63 to build off of kind of back out what the normal health insurance costs are to kind of normalize the health insurance spend, which is roughly $110 million a year, and we're going to spend roughly $34 million, $35 million in Q4 based on these projections, that gets me closer to a $69 million type of an exit rates, which you're looking at a 274, 275 type starting point. And with the new home rate getting about an 80 bps better outcome, we're excited about that. And as I said in my comments, look to grow EBITDA in 2022.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes. And Brian, we're seeing some good trends we've been seeing in the last two to three weeks. So as COVID has been dissipating in the country, I'll have Chris explain it, but we've started to see some really good ADC numbers, and that's going to be very key for next year. But the other thing is we're, so we've been growing our BD staff very nicely. We're ahead of where we expected to be on both home health and hospice. And then on the hospice side, we've been carrying, because the labor market is tight, we've obviously done a really good job on turnover and recruiting. And so we're actually carrying, we're about flat in staffing on a deficit of about 700 ADC in hospice. So we've got enough staff. We're starting to see some sprigs of hope out there. And so we think in general, things are really starting to turn, fingers crossed, but the COVID piece hit us that is pretty hard last quarter. But the key is for 2022 is going to be how well can we position ourselves going into the year with building up ADC, and that's what Chris and his team are really focused on.
Christopher T. Gerard -- President and Chief Operating Officer
Brian, I want to kind of add a couple, a little bit of color to kind of what happened throughout the quarter to set the, that kind of drove the reset for Q4. A couple of key developments. One is we gave updated guidance last quarter. We were somewhat normalized on our medium length of stay in our discharge rate. But sequentially throughout Q3, our median length of stay went from 26 days in July down to 24 in August, 23 in September. That was a material impact on how we exited, ADC-wise. We were actually right on top of our admissions number that went into our updated guidance. But because of the decline in the median length of stay and the increase in discharge rate that also increased sequentially throughout the quarter, that kept us from growing our ADC as we expected. If we would have kept the same 26-day median length of stay as we were expecting, we would exit the quarter right on top of our ADC. And then what we saw happen materially throughout Q3 was the impact to our staff from quarantines related to the Delta variant. And it accelerated quickly through August and peaked at the end of August at 3% of our staff. That caused us to miss a lot of potential admissions on the home health side that would also carried into our start off into Q4 and put us in a different position. So the good news is, as we look into, we're early in November, October, started off kind of similar, but it has improved materially over the last couple of weeks. So we're seeing good signs now in terms of stabilization across all of those metrics, and particularly, our staffing inability to take on new patients. So those things are encouraging, but it's got to build. It's got to maintain and it's got to build throughout this quarter. But those are, that's kind of how, that's what really impacted kind of the reset that we set for Q4.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes. And on the quarantine rates, Chris, they've gone from 3% to what's that we're...
Christopher T. Gerard -- President and Chief Operating Officer
Less than half of a percent now.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes, less than half. So we got our people back. Our BD folks are starting to kick in once the length of stay normalizes. The other thing that I think I'd add to that, Brian, is when we looked at the growth of where the fast length of stay, the discharges were, it was mainly in lung disease or COPD, which means, which was pretty much we correlate that to COVID pushing those results.
Brian Tanquilut -- Jefferies -- Analyst
Got you. And then my follow-up question, just Paul, as we think about labor, there's a lot of focus on that, obviously. Maybe if you can just share with us what your thoughts are and what the right inflation number should, we should be thinking about? And maybe some levers you can pull to manage that, whether it's, I know you give raises every Q3, but the other offsets like mix and other things that you can call out, the temp staffing or anything like that?
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes. I'm going to have, I'm going to punt that to Chris.
Christopher T. Gerard -- President and Chief Operating Officer
Yes, Brian. So yes, you're exactly right. Every year, we're looking at about a 2% to 3% labor wage increase. We did give raises in August of this year, like we do every year for our employees. But we also saw kind of increased demand for either retention bonuses or market adjustments that we have had, we had implemented throughout the quarter. I do think that will tick up the traditional year over year increase for 2022 because a lot of the dollars we gave out in terms of rate changes was to our home health aides and hospice and home health aides and home health, kind of lower wage earners that really needed to be brought up to market. But also with our kind of our clinicians out there, our nurses and therapists, we got more creative around multiyear retention bonuses so that basically we weren't rating the base. So it'll be a little bit of a blip there. In terms of levers, it still comes down to, we feel like we still have opportunity around our LPN RN mix. We're going to get real aggressive on that as well as our PTA PT mix. Every time we move that needle is significant to the bottom line, it can drive down the cost per visit. And again, we're running around 4% of our business are performed by contractors, which there's considerably higher costs than our staff. So retention and recruitment and productivity areas that we'll focus on and continue to be able to replace that high-cost contract business with our own W-2 staff. So I expect that we're going to be able to offset some of those headwinds just by basically executing on those "core strategies".
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes. And I think as I said in my remarks before, Brian, we've made great strides in terms of clinician turnover, and the recruiting is going well. Chris has been leading that effort and with Sharon Brunecz and our people group. And we're excited about, we're moving and innovating in some new areas. Obviously, we talked about predicting turnover. Some of the other things that we're looking at is flexible scheduling, getting more utility out of our PRN pool, recruiting out of our alumni base. So we're in the labor business in the staffing business, and we're building really good tools to make sure we have the right staff because we're going to see an increase in the business from all the BD folks that we have are kicking in. We're definitely going to need to make sure that there's staff there to take care of the referrals that come our way.
Operator
Our next question is coming from Matt Larew of William Blair.
Matt Larew -- William Blair -- Analyst
You discussed, doing OK. You discussed that the environment deteriorated much more rapidly from kind of when you gave guidance in early August to now and obviously it's been related to Delta. But obviously, last November, December and then this January, we saw huge surges in cases. So just kind of curious as you're moving now into the traditional kind of infectious disease season, what your guidance, and Scott, your comments about 2022 take into account from another potential wave of cases, maybe another inflection of quarantine. Just trying to get a sense for how conservative and what kind of worst scenarios if taken into account.
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
Yes. I mean, fortunately, for 2022, if you think about we're sitting here, from the home health side of the business, the way we recognize revenue and so forth, it would take something really significant to greatly change that outlook going forward, pretty comfortable how we're thinking through that. I think the biggest issue that could impact more would be that there's any other blip in the discharge rate. We have left that in our assumptions at a higher elevated discharge rate, so we haven't taken that down. So I think if that discharge rate improvement, that could be a good guide, a positive for us. But I still think we've got high enough to protect us going into the rest of the year. I think if you move into next year, I think the biggest thing to watch for and how it can be impactful is what happens around any additional costs around COVID. I mean we're going to, right now, we've been using CARES Act funds. We've been using, and we've adjusted some items out, but we've kind of got roughly a $3 million run rate between quarantine pay, additional contractor surcharges that we're going to have to overcome into next year. So those are kind of the things that I'm thinking about as we look forward to 2022.
Matt Larew -- William Blair -- Analyst
Okay. And then just on Contessa, you alluded to the EBITDA headwind. But do you still feel comfortable with kind of the original revenue outlook you provided for Contessa for 2022? I guess just remind us the portion of the growth you're anticipating to come from existing partners that are ramping versus the addition of new partners?
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
We think, in general, I've been out on the road with them, Matt, and have just been extremely encouraged. So we're sticking by our guidance, and so expected to deliver the quadrupling of the revenue up to $60 million. We actually are ahead of the game in terms of we'll be announcing something, hopefully, next week, another partnership. So we believe with some of the size of the systems that are out there, it's wonderful hunting grounds within our catchment area. So our belief is that within this area, we can just continue to expand and we are expanding within our original partners. But we're also bringing on new partners. So I think we feel very good about where we are. And I think they're ahead in terms of their new business development efforts. I don't know, Scott?
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
Yes. No, I think, yes, so we feel good about the 60 going into next year, just kind of thinking where we are relative to kind of our capture rate. Did, if you look at our revenue right now, we're slightly behind where we thought we'd be, but EBITDA is ahead. That's really driven by the same labor pressures we dealt with in the other pieces of the segment. We feel great about where we are right now. A lot of effort went to that during the quarter to get some folks hired to help us increase those capture rates. So we feel good pivoting forward into next year and a great pipeline that they had that they bought to it. And we've kind of helped them accelerate that going forward.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
So we're excited.
Operator
[Operator Instructions] Our next question is coming from Justin Bowers of Deutsche Bank.
Justin Bowers -- Deutsche Bank -- Analyst
I'm just going to pretend that Matt's, I'm going to combine my 1.5 with Matt's, just a follow-on. Can you just give us a refresher on the TAM for Contessa, and then if there's a permanent waiver on the fee for service side, how that changes? And then my other question is just, can you give us a little more context on how the hospice discharge rates changed throughout the year? And then it sounds like you have extra capacity right now with all the BD adds and you've kind of stymied turnover there. So like where, given where you are now or what you're projecting for year end with your BD adds, what's kind of the run rate ADC capacity that you could absorb with that staffing mix?
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Well, we, I think we said that there was, our staff is fundamentally, our staffing levels are fundamentally flat, and we're operating now with 700 less of ADC. So Chris has been focusing on finding out where we have capacity and then we've been doubling down on our BD efforts to make sure that we push those efforts to take extra capacity. So in these areas, we've been stealing share. So we're happy with that. We call it pitching and catching. Our BD folks pitch and our clinicians catch. So we feel that we're, our balance is very good. We're building up the BD side where we did have a deficit. And we're ahead on that. And the key thing is on our labor side. That's why we've been so focused. We knew the BD functions, we're going to be increasing tremendously. And therefore, we believe we have the labor in place. There are tight spots, for sure, since we're in 40 states, largely urban, but we've been working through those pretty well. On the TAM, I'm going to let Nick talk about that.
Nick Muscato -- Senior Vice President of Finance
Yes. Justin, we think that the acquisition of Contessa and the contemplation of expanding their business into new lines of services, which I think Paul talked about on the call, beefing up SNF at home, expanding into primary care at home and palliative care at home essentially doubles our TAM, gets us somewhere between $70 billion and $80 billion TAM as we do expand those lines of business. I think the other part of your question was around the Medicare fee for service waiver and what that looks like and what that does with the financial profile of Contessa. We've modeled no expansion of that beyond the public health emergency. So as we talked about our growth rates into 2025 and 2026, I think we put out in our original investor deck, a revenue CAGR that got us to close to $500 million in revenue in 2025, 2026, depending on if that fee for service waiver were to be expanded, that could easily add another $150 million in revenue to that number in a seasonally attractive margin profile as well. So it really would change the game. Ex that, though, we still remain very excited about Contessa's revenue growth potential and have been very pleased with, from a business development perspective, the number of partners that have come to the table and the process that we made there with new JV partners.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes, high quality partners, but we'd be very lucky if there was an expansion. I think Dave is telling us that it's unlikely, but we're trying very hard to make sure that we have an opportunity there.
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
I'd add one thing to that, Justin. As you know, the hospital at home labor programs are tied to the public health emergency. And we see that being extended throughout most, if not all, of 2022. So I think we've got some runway there for that waiver program through 2022, and there are legislative pushes a foot to make those waivers statutory. So let's go through 2022, and we'll keep pushing.
Christopher T. Gerard -- President and Chief Operating Officer
Justin, I want to circle back to the discharge rate throughout the year. January was a high watermark for us, by far. It was 39% of our, beginning of the month since us had discharged throughout the month. And that's also the month that we saw the 18 day median length of stay. So significant other COVID impact there. It ticked down and bottomed out in June at 31.3% and then climbed significantly throughout Q3. And we have built in our model for the rest of this year an additional elevation through Q4. There's traditionally some seasonality, hard death rates in November, December and January than other parts of the year, mainly around the holidays. But, so I feel good with what we have built into our Q4 kind of updated guidance. And what we did see though as we came out of Q2, we thought we were at a good safe place, but it did elevate throughout the quarter, and it elevated sequentially.
Justin Bowers -- Deutsche Bank -- Analyst
Yes, I would just, it's interesting because if you look at some of your peers, the length of stay, had increased sequentially 3Q over 2Q, which I guess is kind of counterintuitive in the current environment, but it points to you guys as a bit of an outlier.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes.
Operator
Our next question is coming from A.J. Rice of Credit Suisse.
A.J. Rice -- Credit Suisse -- Analyst
Just maybe to think about any updated thoughts you have on the organic growth outlook for the two businesses stepping into '22 and beyond. It sounds like the labor dynamics or most, a fair amount of it's short term, the quarantine issue and so forth, but it also sounds like there's a little bit more challenging environment. There could be a constraint on your growth. So I just wondered if you could give us your updated thoughts on where you see the organic growth for the two businesses sort of lining up.
Christopher T. Gerard -- President and Chief Operating Officer
A.J., it's Chris. I think that given our exit rate with our BD FTEs on the hospice side as well as we've grown it on the home health side, our ability to retain staff and have clinical capacity, which is a little bit of a wobble for us in Q3, but we're making great progress in Q4. We see that we're, we should be getting to a more normalized environment for 2022. So I think it's fair to look at mid to upper single digits on organic growth on both lines of business. Probably more challenged on the home health side, just from a Medicare fee for service, which is the better payer of the plans out there in terms of Medicare Advantage, you're still seeing kind of a decline in the actual total market out there of Medicare beneficiaries. So I'd say it's safe to look at mid single digits on both lines of business if we execute on our plan.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes. And assuming there's no new, no new variants that are coming through. But again, I think what we've been doing, particularly in hospice because it's a fixed cost model, is we've just been holding on to staff. We think it's really prudent and safe to maintain the staff we have going into what we anticipate is going to be normalized growth rates.
Operator
Our next question is coming from Sarah James of Barclays.
Sarah James -- Barclays -- Analyst
I just wanted to understand a little bit better the context of the labor trend that you gave us, you said it was increasing at about 3% unit cost. What is it normally for you guys? And then are you seeing that change reflected in the rates that you're getting from the payers for, I guess, the rates that you've negotiated for '22, are you seeing it factored in?
Christopher T. Gerard -- President and Chief Operating Officer
Yes. So we're, the 3%, we're 2.5% to 3% pretty much every year just through planned raises. We think for 2022, it's going to be north of that, maybe even more up possibly 5% total wage inflation. The market has reset in some areas. We think we're going to have to work through that. And again, the levers that we have to offset that, that we feel very good about being able to pull will be lower cost caregivers, LPNs and PTAs versus RNs and PTs, as well as us with our retention and building up clinical capacity, internally driving down the contractor utilization. So we think we can keep that down in that 3% range if we're able to execute on pulling those levers. What was the second question?
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
I think we're good.
Sarah James -- Barclays -- Analyst
Whether or not that's being reflected in...
Christopher T. Gerard -- President and Chief Operating Officer
Yes. Yes. No, we're not, unfortunately, Medicare Advantage plans are not quick to say, yes, we see that you're troubled, so we're going to give you more money. So we are basically trying to build in our new cost structure on new rate proposals when we have updated plans or plans are going through contracting. Obviously, access to our caregivers and our care is important to them. So there is an alignment there. But right now, it's such a new phenomenon. I mean the rate inflation, the wage inflation has really only picked up its steam in the last probably 60 to 90 days. So there'll be a while before that flushes out. We did see in the new final rule for Medicare rates, a 80 bps kind of increase in the final rule versus the proposed rule, which is inflation-related, which is, we see that as a good sign.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes, that should cover some of it. But I think in general, we, Chris and Dave Kemmerly, have done a really nice job of getting, moving us to risk as much as possible where we can get some gain share risk with the MA payers and the conveners. We're still working through a lot of this, but we're very hopeful that we can move more to risk and outcomes to grow our level of reimbursement there. We're very willing to bet on our performance.
Sarah James -- Barclays -- Analyst
And just to clarify, you guys mentioned higher signing bonuses for multiyear retention contracts. Are you expensing all of that right away or allocating it over the multiyear retention period?
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
The multiyear retention period. That's the reason we're doing it. We're not trying to take all the hit now and also give the employees kind of reasons to stick through some of this. So it can be paid over '21, '22, and sometimes up into '23.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
We see the longer we keep people, the longer, the better the chances, the less the turnover occurs. So part of the plan, why retention bonuses are a good thing is you can defer the cost and they have some incentive to stay. And once they build their relationships with their patients in the care centers, they tend to stay longer and be better in terms of turnover.
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
And just to be clear on the, in my comments, I called out about $2 million of additional costs that was outside of the planned wage increases, about $1.2 million, I would call it as permanent, that was raises mainly, as Chris said, around home health aide and some other hourly people. The other 800 was related to bonus retention and sign on bonus expense.
Operator
Our next question is coming from Frank Morgan of RBC Capital Markets.
Frank Morgan -- RBC Capital Markets -- Analyst
Just a question here. Interested in your comments you made about consolidation. It seemed like you might perhaps be more aggressive in M&A next year. And I'm just curious, am I reading that right? And if so, what kind of magnitude of, should we expect there in a perfect world? And then maybe also from a mix standpoint between home healthcare and hospice.
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
Yes. I think we plan to be more aggressive into next year. We're trying to be aggressive this year actually. It's just, unfortunately, we got a bad start to some deals that we thought we'd get over the finish line that just didn't meet our standards from, in our review procedures. So we spent $275 million to date. That does include Contessa. Walking into the year, we had said we'd like to send somewhere around $300 million, somewhere around kind of what a year's cash flow would potentially have looked like. But we'll still continue to push, I'd say would be heavier at home health. But I wouldn't, we'll spend what we need to get done. And so we can always, we've got a lot of availability on the balance sheet to do a lot of things in order to get deals. So I think we'll kind of take a reassess of where we are. I think you will see us, and we will be active and aggressive. We're active every day in this market. It's just what we can get across the finish line. So I'm hoping for bigger 2022 from the home health side. I think we talked about the CARES Act money, the sequestration going away. Those two have been dynamics, and now you have these labor pressure dynamic which is going to affect everyone in the industry. But I think our balance sheet has set us up very well to take, when there's availability, we can do some more acquisitions.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes. And I'd add to that, Frank. I've been out on the road with Contessa and I think there's tremendous opportunity there, particularly in some of the geographies and the partners they're working with. There's been a lot of conversations about finding better ways to partner, including joint ventures, with some of these big systems and outright purchases. So I also think that Contessa's really added to that. And there's a lot of folks out there now, particularly in the home health world, that are starting to look at next year significant concern. So we're starting to hear the phone ring a lot more.
Operator
Our next question is coming from Whit Mayo of SVB Leerink.
Whit Mayo -- SVB Leerink -- Analyst
I'll be quick. Just how much more room do you guys think you have to push on visits per episode? And Medalogix has acquired some new capabilities. Just curious if you can maybe talk about that. And any tools that help enable this change on LP and PT opportunities that you keep referencing.
Christopher T. Gerard -- President and Chief Operating Officer
Yes. It's Chris. On, in terms of BP, we do see there's still, the Medalogix analytics suggest that there still is opportunity for fewer visits without compromising care and quality of the patients. We're now really starting to expand some use of telehealth within our markets and with our programs that we think will help in some of those areas as well as, again, focusing on the LPN and PTA utilization. Actually, HomeCare HomeBase has a smart scheduling module that we started project, we started piloting this year. In the markets where we have done it, we've seen significant movement in our PTA and LP utilization. So we're expanding that across the rest of our organization as we speak. And then as far as the Medalogix's new tools, with Muse, a hospice product that they had in place, which was not really on our radar earlier this year, has been a phenomenal tool. So we piloted that starting in September, and we've accelerated rollout of that. We will be fully rolled out by the end of this year. That gives, helps us with the actual clinical capacity on our hospice side and gives us growth capacity within the organization and better efficiency as well as improves the care that's delivered at the last days of life. So we're encouraged by all of that. We've got a lot in play right now, but between smart scheduling, employee retention, launching of Muse, I think that, that's going to help us with our capacity for next year. As far as how much more we can go lower in business per episode, the data suggests it's probably up to another full visit if we were 100% optimized, but we're just basically continuing to protect the model and starting to launch some new tools like the news for research as well as intra episode capabilities that Medalogix is working on today. So I think over time, you'll see it just get kind of get into that right spot. It will likely be a little bit lower than where it is right now.
Operator
Our next question is coming from Matthew Borsch of BMO Capital Markets.
Matthew Borsch -- BMO Capital Markets -- Analyst
So my question, I think you did really start to address it there was about how the M&A landscape may be changing relative to some of the pressures that we've been through PDGM. And now everything with COVID, it's been quite a ringer. But let me refine that just a little bit. The hospice valuations have been pretty elevated for quite a while. And I'm curious where there's maybe been more impact on that business, if you have any sense that maybe some of the hunt for those companies from private equity or wherever has come off a bit.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
We haven't, no, we haven't really seen that, Matt, up to this time. They're still pretty elevated, their deals are getting done at 20 plus times EBITDA. We, these, I think people believe that, like we believe, that this is a short term bump, that reimbursement is going to be good, that the demographics behind people wanting to die at home is huge. So what we're seeing is, I'd say private equity is willing to go and invite toehold. So very strong regional players. And then overpay for them and hopefully amortize that through smaller deals or de novos around those areas. But those have been very successful strategies thus far for private equity folks who are doing it. Big national plays, haven't seen it.
Nick Muscato -- Senior Vice President of Finance
Yes, and that's what's driving it. Right now in hospice, we're trying to value some of these deals when you have this discharge rate disruption and fluidity, and that certainly can be challenging. So home health seems like the right place for us to focus early. We got some stability there in the back half of next year. You could probably see us take a look at some more hospices that makes sense for us.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Yes. And there's a dichotomy that exists in home health. If they're under our license area, it's easy to do because we don't have to absorb the license, invest the liability. In CON states where we don't have coverage and in other places where we're moving to get coverage, we have to do a lot of diligence, so we make sure we know what we're getting. But, so we also anticipate significant shakeout. Sequestration's coming back in, the payroll taxes due, the receivables that people borrowed is due, CARES Act monies done. So, and then there's been some significant issues with quarantine and labor costs for smaller players. So we're anticipating this is the year. We've been saying that for a while, but hopefully, we'll be right early in the year.
Operator
Our next question is coming from Joanna Gajuk of Bank of America.
Joanna Gajuk -- Bank of America -- Analyst
I guess a lot of questions were asked. But I guess, so one thing I have here, I appreciate that the comments you made on the organic growth outlook long term for both businesses, right, in mid-single digits. So still, you seem quite positive and maybe a little bit lower than what you were talking before. So just want to clarify that. And I guess on the hospice business, I guess, building on the latest comments here. But are there any structural changes in this business? I mean we obviously understand the aging demographic, the inclusion penetration and the growth in reimbursement, but anything could be said in terms of just some of the pressure, pressure of some of these referral sources and the hospice carving in into like MA, like anything to be said about those things? And I guess, just to summarize how does this mid single digit compare to how you were thinking about the growth rates for these businesses before?
Christopher T. Gerard -- President and Chief Operating Officer
Yes. I'd start off with, the one thing that's materially different from what we were talking about a year ago on the growth rates in hospice is the pull-forward of death and acceleration of death that COVID has actually caused. I think if you step back and you look at 2021, actually, the hospice utilization market declined versus an expected growth, and it's still going to be negatively impacted next year from accelerated death. So basically, the market is shrinking a little bit or not growing at the pace that we were expecting when we rolled out our 2021 plan. In terms of the carve-in. We're utilizing we're having carve-in access through some of our plans right now, very, very little volume today. It doesn't look like there's going to be a tremendous amount of pickup and take-up of it in 2022. So it really has not impacted the traditional go from MA to traditional Medicare or hospice transitions. What we do think we have an opportunity around is just basically identifying our patients to transition from home health to hospice a little bit earlier in the dying process.
We do a decent job of transitioning those patients when appropriate. But the length of stay has been relatively low. So we're working some programs, particularly Medalogix's products on that to help us kind of identify those patients a little bit earlier. And then on the home health side, growing that market, particularly with, again, the shrinking Medicare fee for service enrollment population and the aggressive growth of the Medicare Advantage population. We still have kind of a rate gap that we're still trying to kind of close as much as possible. And clinical capacity on home health will probably be much more challenged for us even with our lower turnover rates and our performance around unlocking new capacity, just by virtue of the way the industry is. So we think that mid-single digits in home health is a good place for us to pay for next year. Could we outperform it? Absolutely. Are there things out there that we think are going to be wobblers or just really structurally, structural headwinds? Not really. I would say that caution has to be built around the mandate, the vaccine mandate that's coming out because it really likely will not impact us in 2021. But the mandate is impactful to the business, then that can create a slow start to 2022.
David L. Kemmerly -- Chief Legal and Government Affairs Officer
Chris, to add one piece of color. Joanna, it's Dave. On the VBID, our hospice component for 2022, there are only 13 MA plans participating in the hospice component, whereas there were nine in 2021. So not a lot of uptake there, so it hasn't significantly impacted us.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
And I think what we'll see, Joanna, is potentially deferred care as these hospital beds free up. We are, we're watching to see who fills those beds and to understand if this is delayed care, if they're going to be sicker. So that's what we'll be watching for in the next quarter or two.
Operator
Our next question is coming from Andrew Mok of UBS.
Andrew Mok -- UBS -- Analyst
Wanted to follow up on some of the hospice comments. It sounds like there's some countervailing forces between admissions and length of stay. So as trends in length of stay normalize at the patient level, there also might be a moderation in admissions due to excess mortality. Can you talk about the interplay between admissions and ADC and how you see that playing out over the next 15 months?
Christopher T. Gerard -- President and Chief Operating Officer
Yes. So on the admission side, we feel like we're squarely in a market share taking position today and actually adding our BD FTEs and identifying new referral sources. We added 1,100 new referral sources in Q3, which is exactly what our strategy is to do and continue to do. So we think that also using data to understand where, kind of where the right targeting is from a length of stay perspective is helping us to look at some stabilization there. Pandemic aside, there should be a distinct correlation between emission growth and ADC growth, even though the ADC growth lags a little bit as you do that. We've had years of tight correlation in the past of X percent of admission growth equals Y percent of ADC growth over time. We think we're going to get to that point. What we are seeing even happen today is our admission growth volume is equally, is pretty equal between the Northern states and the Southern states. And right now, we see median length of stay and discharge rates stabilize in the southern states since the pandemic has kind of moved through there up north. And so even though equal growth rates that we're seeing between both regions, we're seeing distinct ADC build happening in the southern states, which is what we would expect to see. So I think there's still going to be these pockets of and blips that are out there. We're cautious around that. It's hard to predict. We can't predict discharge rates. We are not changing the segmentation of where we're getting our referrals from. So I feel like there's going to be some sense of normalcy that should start to materialize, and we're starting to see it happening in the south right now.
Operator
Our last question today is coming from Gary Taylor of Cowen.
Gary Taylor -- Cowen -- Analyst
Just one clarification one and one question. When you were talking about the growth in EBITDA for 2022 versus the revised '21 guidance, I think Scott said you would be absorbing some of the COVID costs that you had been calling out in the '21 adjusted EBITDA. And I just wanted to make sure that I had that correct. Or would you still be anticipating adjusting out some of the COVID costs in '22, if there are any?
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
Yes. Yes. That's a great question. Just as everything, I'd say everything is fluid. But as of right now, I'm assuming we stay at the pace and things without a new variant that really accelerates things, I would say we're going to have to consider these costs as kind of normalized operating business going forward. So right now, my thinking is it goes into 2022, and I'm not adding that cost back and run kind of exiting kind of Q3 at somewhat of a $3 million range on that. And we'll continue to work that down. But that's just something that as it stands today, that's where we think it will be.
Gary Taylor -- Cowen -- Analyst
And then just going, my question then is just going back to the possible healthcare employee mandate, a vaccine mandate, do you have any updated thoughts on the timing? Obviously, that was proposed in September. We've heard from various sources imminent and we were hearing that a few weeks ago. So any thoughts on timing? And can you update us on your employee vaccination rate. I think you had said on the 2Q, was just over 50%.
David L. Kemmerly -- Chief Legal and Government Affairs Officer
Yes. Gary, I can take the time, and it's Dave. The vaccine mandate rule cleared OMV earlier this week. So it's sitting back at CMS. So we truly believe it's imminent this week. We expect that to be released. But probably didn't get released today since the home health rule payment update we released yesterday. So I think it will be literally in the coming days.
Christopher T. Gerard -- President and Chief Operating Officer
Yes. And we're right now around 67% fully vaccinated and probably another 5% to 6% that are either partially vaccinated or have stated they intend to get vaccinated. The last piece I'd say though is we've seen some state mandates come into play already, that we've noticed kind of acceleration of vaccination rates in those states as the deadlines quickly approached. And in fact, it hasn't negatively impacted us in those states where the mandates have come into effect for the most part. I'd say only on the personal care side, Massachusetts was probably the biggest challenge for us so far. But we are continuing to educate and focus on getting our employees to do the right thing and get vaccinated, say, for their own protection and the patient's protection. But the mandate could be, as the southern states, the lower vaccinated states are starting to come online. That's where we're going to have to really be close to it.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
And we're trying to be as proactive as possible there with estimating where there's going to be issues and start to build up our recruiting there.
Operator
Thank you. I would now like to turn the floor back over to Mr. Kusserow for closing comments.
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
All right. Thank you. I want to thank everyone who joined us on our call today. I'd also again like to thank all our caregivers who delivered yet another great quarter of results despite the trials and tribulations that have been caused by COVID. Please keep doing what you're doing. First things first. Keep taking care of the people who need us the most. If we continue to do that, we'll always thrive. We hope everyone has a wonderful day, and we look forward to updating you on our ever evolving progress and purposeful work on our next quarterly earnings call early next year. We're excited, and we hope you are too. Until then, take care.
Operator
[Operator Closing Remarks]
Duration: 79 minutes
Call participants:
Nick Muscato -- Senior Vice President of Finance
Paul Berthold Kusserow -- Chairman and Chief Executive Officer
Christopher T. Gerard -- President and Chief Operating Officer
Scott G. Ginn -- Executive Vice President and Chief Financial Officer
David L. Kemmerly -- Chief Legal and Government Affairs Officer
Brian Tanquilut -- Jefferies -- Analyst
Matt Larew -- William Blair -- Analyst
Justin Bowers -- Deutsche Bank -- Analyst
A.J. Rice -- Credit Suisse -- Analyst
Sarah James -- Barclays -- Analyst
Frank Morgan -- RBC Capital Markets -- Analyst
Whit Mayo -- SVB Leerink -- Analyst
Matthew Borsch -- BMO Capital Markets -- Analyst
Joanna Gajuk -- Bank of America -- Analyst
Andrew Mok -- UBS -- Analyst
Gary Taylor -- Cowen -- Analyst