Image source: The Motley Fool.
Privia Health Group, Inc. (PRVA -3.35%)
Q1 2022 Earnings Call
May 12, 2022, 8:30 a.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Good day, and thank you for standing by. Welcome to the Privia Health Q1 2022 conference call. [Operator instructions]. Please be advised that today's conference is being recorded.
[Operator instructions] I would now like to hand the conference over to your speaker today, Robert Borchert, SVP of investor and corporate communications. Please go ahead.
Robert Borchert -- Senior Vice President, Investor and Corporate Communications
Thank you, Gigi, and good morning, everyone. Joining me today are Shawn Morris, our chief executive officer; Parth Mehrotra, president and chief operating officer; and David Mountcastle, our chief financial officer. This call is being webcast and can be accessed from the Investor Relations section of priviahealth.com. Today's press release highlighting our financial and operating performance and the slide presentation accompanying our formal remarks are posted on our IR website.
Following our prepared comments, we will open line for questions. We ask that you please limit yourself to one question and one follow-up, so we can get through the queue in a timely fashion. The financial results reported today and in the press release are preliminary and are not final until our Form 10-Q for the quarter ended March 31, 2022, is filed with the Securities and Exchange Commission. Some of the statements we will make today are forward-looking in nature based on our current expectations and our view of our business as of May 12, 2022.
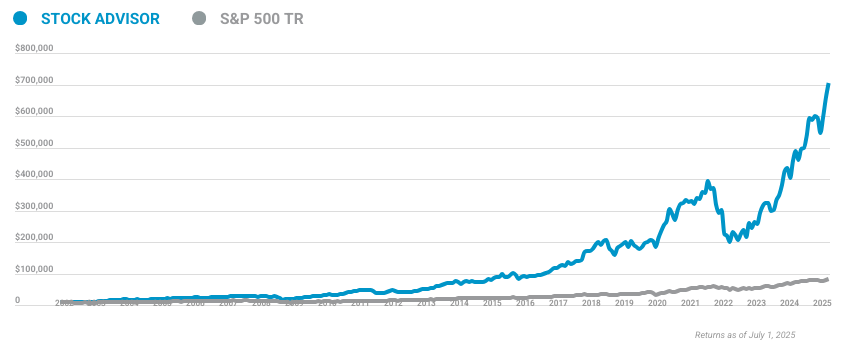
10 stocks we like better than Privia Health Group, Inc.
When our award-winning analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Privia Health Group, Inc. wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of April 7, 2022
Such statements, including those related to our future financial and operating performance and future business plans and objectives, are subject to risks and uncertainties that may cause actual results to differ materially. As a result, these statements should be considered in conjunction with the cautionary statements in today's press release and the risk factors described in our company's most recent SEC filings. Finally, we may refer to certain non-GAAP financial measures on the call, and reconciliations of these measures to comparable GAAP measures are included in our press release and the accompanying slide presentation posted on our website. Now I'll turn the call over to Shawn.
Shawn Morris -- Chief Executive Officer
Thank you, Robert, and good morning, everyone. We are very proud of the success that Privia Health and our provider partners have achieved prior to and since our IPO a year ago. The physician-patient relationship is the cornerstone of our healthcare ecosystem, and we are honored to be one of the nation's leading physician enablement organizations. This past Tuesday, we were excited to celebrate our one-year anniversary as a public company at the NASDAQ marketplace, along with 17 physician leaders, representing our more than 3,300 physicians and providers across eight states and the District of Columbia.
With our continued momentum in the existing markets, Privia Health posted another strong quarter of financial and operating performance in the first quarter of 2022. We remain highly confident in our growth outlook for 2022 and beyond as we continue to organize physicians in the scaled provider networks across our country. This morning, I'll present an overview of the key highlights. Parth will provide a business update, and then David will conclude with our recent financial performance and updated outlook for 2022 before we take your questions.
Privia Health is continuing to execute at a very high level, and our first quarter results clearly highlight this. Our practice collections increased more than 63% year over year, and our operating model is already working at scale. Adjusted EBITDA was a quarterly record and was up over 48%, while we're investing across our enterprise to support this accelerated top-line growth. The business momentum and high forward visibility into our growth metrics is reflected in our updated financial guidance for 2022.
Our growth is being driven by a balanced set of strategic initiatives. This includes continued same-store growth driven by the strength in ambulatory utilization across all of our existing practice locations. This patient volume is a benefit to both our fee-for-service collections, as well as supporting the performance in our value-based arrangements, as we serve patients in lower-cost care settings. As we align with and enable our provider partners and expand our number of attributed lives, our operational execution and clinical performance is continuing to drive strong results across our value-based arrangements.
We generated another solid quarter of new provider additions in existing markets and in combination with the sustained high level of provider retention. In addition, our active business development pipeline remains robust as we look to enter many new markets over the next few years. With that, let me ask Parth to provide more details on market position and expansion.
Parth Mehrotra -- President and Chief Operating Officer
Thanks, Shawn. Privia Health is building one of the largest primary care-centric ambulatory care delivery networks in the country. Our business model has a number of distinct attributes that are replicable across all 50 states, as we partner with all provider types, serve all patients across all reimbursement models, and participate in value-based arrangements in the broadest possible way. Our model offers a tremendous market opportunity for growth in the physician enablement space as we scale nationally and partner with independent providers, as well as health system or other facility affiliated or employed providers.
We introduced Privia Care Partners in the second half of 2021 as a highly complementary partnership model. This is offered to provider practices looking to partner with Privia, but wanting to start first with a risk-bearing entity only such as our ACOs. One advantage of our platform is that we contract across commercial, Medicare, and Medicaid programs. This offers much broader value-based care opportunities for our payer and provider partners in many states.
It also brings balance and diversity to Privia's overall operating and financial profile. A unique component of our growth strategy is our ability to monetize our at-scale medical groups and risk-bearing entities, as we gain density in our markets. We are able to offer a number of these value-added services to our physician and payer partners as part of an integrated ambulatory care delivery system. Underlying our integrated medical groups and risk-bearing entities in each of our geographies is Privia's stack-enabled clinical and management services platform.
This enables us to maximize physician alignment and deliver superior outcomes in value-based arrangements without owning the underlying practice. As Shawn noted, our business momentum has continued to be extremely encouraging across both existing and potential new geographies. Our national footprint now includes 3,370 implemented providers caring for more than 3.8 million patients across our 870 practice locations in eight states in the District of Columbia. As one of the largest provider groups in the country, our scale and geographic density is also defined by a breadth of medical specialties.
While approximately 65% of our practice partners are primary care-focused, including internal medicine, family medicine, pediatrics, and OB/GYNs, we actually partner with more than 50 specialty types. This provides Privia with some unique advantages as we partner with payers to offer a broad ambulatory care delivery network that can improve patient outcomes and reduce costs across the value-based care spectrum. Our operating model and strategy has led Privia to have one of the broadest, most balanced, and well-diversified value-based care platforms in the industry. Our more than 80 at-risk payer contracts now cover approximately 848,000 attributed lives across commercial, Medicare, and Medicaid programs.
This is up 17.6% from a year ago and more than 10% since the end of 2021, giving us a lot of momentum and visibility for the remainder of 2022. We take upside and downside risk in many of our payer contracts covering nearly two-thirds of the attributed Medicare lives across MSSP and Medicare Advantage programs. This thoughtful move to risk continues to provide significant opportunities for top-line and EBITDA growth, as we execute on our goals and earn greater shared savings in the years to come. Now I'll ask David to review our first quarter financial results and updated outlook for 2022.
David Mountcastle -- Chief Financial Officer
Thanks, Parth. Our outstanding first quarter performance highlights that our operating model is already working at scale, and our business momentum continued into 2022. Practice collections increased to $561.9 million, up 63.3% from Q1 a year ago. As we noted last quarter, we will report our capitated revenue as a new line item in our sources of revenue section of our 10-Q.
Capitated revenue was $48.3 million in Q1. Care margin increased 36.4%, and adjusted EBITDA was a record $14.8 million, up 48.8% over the same period last year. Our expected -- as expected, our top line grew faster than EBITDA this quarter due to the new capitated arrangements, as well as investment across our business enterprise to support this accelerating top-line growth. At the same time, you can clearly see the operating leverage in our model as our top line and care margin growth is translating nicely into EBITDA growth and margin expansion.
Our adjusted EBITDA margin as a percentage of care margin increased 180 basis points from a year ago to reach 20.7%. Given our first quarter performance, business momentum, and visibility through the rest of 2022, we have a high level of confidence on our updated financial guidance. We now expect practice collections, GAAP revenue, and care margin to be in the mid- to high end of our guidance ranges with platform contribution and adjusted EBITDA expected to reach the high end. Our guidance for implemented providers and attributed lives are unchanged at this early stage of the year.
We remain focused on continuing to execute on our multiple growth initiatives. This includes growing existing practices, increasing attribution and risk-based contracts, adding new providers, identifying opportunities to expand our platform, and opening new markets over time. Our underlying assumptions are unchanged from our previous 2022 guidance, and I wanted to note that our outlook includes only previously announced new market entries. One of Privia Health's key differentiators is our solid balance sheet and positive annual free cash flow.
We ended Q1 with a net cash position of more than $283 million, with capital expenditures of less than $1 million. We continue to expect more than 90% of our adjusted EBITDA to convert to free cash flow for the full year 2022. This financial flexibility and strength gives us confidence to invest on our growth initiatives and fund all strategic opportunities in the foreseeable future without reliance on any external sources of capital to continue to expand our platform nationally. We continue to grow and expand our business with all types of healthcare providers that are looking to partner with scale financially sound organizations to improve outcomes for their entire patient population.
With that, operator, we are now ready for our first question.
Questions & Answers:
Operator
Thank you. [Operator instructions] Our first question comes from the line of Josh Raskin from Nephron Research. Your line is now open.
Josh Raskin -- Nephron Research -- Analyst
Hi. Thanks, and good morning. Just first numbers question. I think I heard you say -- I think David said we're going to put it in the Q, the practice collection, the 561, how much of that was value-based care? Was that the $48 million that you mentioned? And what was that number a year ago? And if you could just remind us the assumptions you make in terms of accruals for value-based care earnings sort of this early in the year.
Parth Mehrotra -- President and Chief Operating Officer
Thanks, Josh, for the question. Look, you'll see the disclosure in the Q where we'll clearly mention the capitated piece of the revenue -- or the practice collections. There's obviously other shared savings accruals and the care management fee that we've also broken out, so you'll see that in the Q. But roughly, you'll see that accreting much faster than last year because of the capitated arrangements that we -- that started this year.
Robert Borchert -- Senior Vice President, Investor and Corporate Communications
But we stated that revenue from capitation was $48.3 million.
David Mountcastle -- Chief Financial Officer
$48.3 million from the new capitated revenue, correct. And again, there's a table in the Q that's going to break out the revenue.
Josh Raskin -- Nephron Research -- Analyst
OK. But the total value-based care portion of practice collections would be higher than that $48.3 million. Is that right?
Parth Mehrotra -- President and Chief Operating Officer
Yeah, that's absolutely right.
David Mountcastle -- Chief Financial Officer
Correct. Right. So for example, shared savings increased as an example.
Josh Raskin -- Nephron Research -- Analyst
Right. OK. And then of your providers, I'm just curious if you could give us just to sort of look at the pipeline, but how many providers are sold as of today, but not yet in that were as of March 31, but not yet implemented? And maybe if you just have broad comments on that pipeline for physicians.
Parth Mehrotra -- President and Chief Operating Officer
Yeah, definitely. So we don't disclose sole providers. But as you understand our model, it takes about five to six months to implement providers, credential them in our medical groups and so forth. So at this point, sitting in May, we almost have visibility through to the end of the year, and the pipeline is pretty full.
We had a record sales year last year and one of our best first quarters this year. A lot of momentum we continue to see in our existing geographies. And obviously, the business development pipeline is pretty robust. So all of that will translate into the implemented provider growth for the rest of this year and then going into 2023.
Josh Raskin -- Nephron Research -- Analyst
OK. That's helpful Thanks.
Operator
Our next question comes from the line of A.J. Rice with Credit Suisse. Your line is now open.
A.J Rice -- Credit Suisse -- Analyst
Hi, everybody. First of all, I guess, just on the capitated lives, I think at 1/1, you said in Medicare Advantage at about 23,000. Looking at your 106,000 today of 28% are in full risk that puts you to about 30,000. Can you give us a sense of how that's likely to trend over the rest of the year where you have a view of where you'll end the year on capitated MA lives? And is there a seasonality to the additions of those lives?
Parth Mehrotra -- President and Chief Operating Officer
Yeah, sure. So we started with 23,000. Obviously, the intent is to grow that year over year. As we stated previously, we'll be very thoughtful in adding lives to the capitated arrangements once we are certain that the financial profile is appropriate.
So you should see an accretion. And while we're not going to break out specifics, that has trended up from the 23,000 numbers, so your estimate is ballpark right. And then again, as we enter into -- this is -- this should be pretty front-end loaded in the beginning of the year given the nature of these contracts relative to, for example, the commercial or the MSSP attribution. So pretty much, you should see that stable now going into the rest of the year.
And then as we add lives, it'll likely be at the beginning of next year.
A.J Rice -- Credit Suisse -- Analyst
OK. And then maybe just a follow-up, another sort of clarification question. On the Q1 practice collection that came in above the high end of your range, is there any seasonality or step down that occurs in Q2, Q3 that we should think of given the strong start?
OK, great. Thanks a lot.
Operator
Our next question comes from the line of Lisa Gill from J.P. Morgan. Your line is now open.
Lisa Gill -- J.P. Morgan -- Analyst
Great. Thanks very much, and good morning. I just first want to start with cash flow. I appreciate your comment around 90% of adjusted EBITDA for the year.
But cash flow in the first quarter was negative, and it looks like you had a nice increase on the receivable side. Is that just a timing issue? Can you maybe just talk about how the cash flow would be my first question?
David Mountcastle -- Chief Financial Officer
Yeah. Thanks, Lisa. Yes, it's definitely just a timing issue. We're expecting the trend this year to kind of mirror last year.
We do have one unique item in Q1 where we pay our annual bonuses, so that's a relatively large cash outflow in Q1. And then just the timing of our value-based arrangements and when we receive that cash, we expect it to be similar to last year. So Q1 is generally our equal to or negative cash flow quarter. And then it just builds from there.
But we are still expecting sort of 90-plus percent by the end of the year.
Lisa Gill -- J.P. Morgan -- Analyst
OK, great. And then just another question. As we think about just the timing of things, and you had a nice beat, congratulations in the first quarter. And as we think about the guidance for EBITDA for the rest of the year, is there seasonality? Do you have some kind of increased expectations, for example, around rising labor rates? Is there anything you would call out specifically as to how to think about the first quarter beat and the guidance for the rest of the year?
Parth Mehrotra -- President and Chief Operating Officer
Yeah. Sure, Lisa. It's Parth. Look, it's a great start to the year and gives us a lot of confidence.
We gave you our guidance six weeks ago when we are here guiding to the high end on EBITDA and care margin. So -- and platform contribution. So the bottom-line metrics are really showing the operating leverage in the business as top line performs. Our hope is that continues.
Obviously, stuff to predict utilization and things like that, but the EBITDA trend should mirror last year. Again, we should continue to hopefully see that same seasonality. So our hope is that this strength continues into the year, and we'll update the guidance as it goes. But again, it's pretty early in the year, but we're excited to guide toward the high end at this stage.
Lisa Gill -- J.P. Morgan -- Analyst
Great. Thanks very much.
Operator
Thank you. Our next question comes from the line of Ryan Daniels from William Blair. Your line is now open.
Ryan Daniels -- William Blair and Company -- Analyst
Yeah, good morning. Thanks for taking the question. Maybe one financial and one more strategic. Just on the financial, obviously, strong start to the year, but I'm curious what the delta is between the reiteration of lives and at-risk lives and providers and then the revenue and profits.
Are you seeing better utilization? Is that the key driver, a better risk adjustment? Just any color there to give us some feel for that delta would be great.
Parth Mehrotra -- President and Chief Operating Officer
Hey, Ryan. It's Parth. So on practice collections, like I mentioned, it's fairly broad-based beat across both utilization on the fee-for-service, good performance on value-based care, and then provider ads were pretty strong ending last year. We've implemented providers and attributed lives.
Those metrics, it's still Q1 in the year, and we are nicely ahead sequentially from Q4 last year. But it's still early in the year, so we're maintaining our guidance. Our hope is we keep seeing that momentum, and we'll update it. Obviously, the guidance does not include any new markets that we may add during the course of the year.
We have a pretty active BD pipeline. So hopefully, we'll update that as we did last year when we entered those markets. But again, given the visibility and those two metrics move the slowest in terms of just how providers are implemented, how lives are added during the course of the year, so much more stable. But it's great to see the outperformance on both collections and then flowing through the P&L down to EBITDA.
Ryan Daniels -- William Blair and Company -- Analyst
OK. Absolutely. That's helpful. And then a more strategic question, and maybe I'm overthinking this a bit, but your partnership with Surgery Partners seems like an interesting case study for your business model, and that it's in a pretty small state, which I assume you could only move into with your type of multi-payer platform.
And then number two, kind of speaks to the ability to manage a wide number of specialists and maybe downstream and ambulatory care. So can you speak to that a little bit? Again, I know it's not a huge revenue driver, but it seems pretty strategic to the strength of the model. Thanks, guys.
Parth Mehrotra -- President and Chief Operating Officer
Yeah, definitely, I'll start, and Shawn can add. Look, just broadly speaking, if you take a step back, our strategy is to build these very large-scale medical groups focused on primary care providers, and then we surround them with the right specialist. We partner with lower-cost health systems. And then obviously, entities like Surgery Partners and providing these value-added ancillaries as part of this broader ambulatory care delivery system, if you will, this is what we believe is fundamentally going to be a very valuable entity and where the puck is moving.
It allows us to have a very broad access to the TAM, participate in 50 states, all patients, all payers, all reimbursement models. The only other company that does this at somewhat national scale, given the assets they've acquired, is Optum Care, as you know, but very similar strategy. We are a fraction of the size. Obviously, we don't have the balance sheet, but we are trying to do that in a very thoughtful capital-efficient partnership model and -- but we're trying to achieve the same result.
Shawn Morris -- Chief Executive Officer
Yeah, Ryan. The only thing I would add or reiterate, as you mentioned or noted to in Parth's comments is the ability to move into a state like Montana and get there early, teach the doctors of kind of value-based levers. And it really, to you point out, was a company like Surgery Partners kind of -- our strategies aligned really well. I mean, they're a low-cost setting, and we can go out kind of build the medical group as we go, kind of direct that care to the lowest cost setting in our value-based arrangements and move that market over a period of time as we kind of work and align with payers that want to take the market that way.
So it's -- we would, obviously, seek other partners like that. It makes a lot of sense for us to get into a market early and establish ourselves with the relationships with those types of providers.
Ryan Daniels -- William Blair and Company -- Analyst
Perfect. Thanks, and congrats on the momentum.
Operator
Thank you. Our next question comes from the line of Whit Mayo from SVB Securities. Your line is now open.
Whit Mayo -- SVB Leerink Partners -- Analyst
Thanks. I think I just want to start first with the investments that you guys were making coming into 2022. I think given a lot of the growth, the momentum, the new markets, the ACOs, the risk platform, you needed to stand up some infrastructure. Has anything changed on those investments? Do you need to make more or less? Just any early observations or thoughts would be helpful.
Parth Mehrotra -- President and Chief Operating Officer
Yeah. Hey, Whit, thanks for the question. No, they stand, as you stated and as we have communicated at our last earnings call, we're continuing to make those investments. It is obviously great to see the organization execution across the board.
You're seeing that in the financials very clearly as we've outperformed on the top line. And the beauty of the business is, despite those investments, we are outperforming on EBITDA and free cash flow. And I think you're getting this business given our guidance that is now growing 35% this year on the top line and 35% plus on EBITDA, and we're not sacrificing that -- any compression from those investments, it speaks to the scale of the business already and where we are with our margin profile, pretty much halfway there, or more than halfway there from a long-term margin. So we feel pretty good about where we are with the investments.
We obviously -- there's a big TAM out there and we're looking to enter new markets, but we are thoughtfully investing in the business. But the momentum is helping us not sacrifice EBITDA as we make those investments.
Whit Mayo -- SVB Leerink Partners -- Analyst
Yeah. No, that's helpful. And you've sort of alluded to this a couple of times that I wanted to get more directly and specific on the ACO performance in the quarter. I know it's early, but you're getting some feed of data in from CMS that should give you some visibility into sort of how you're tracking versus expectations.
So how are you tracking versus your internal plan there just with the new ACOs and also those that have converted into the extended track? Thanks.
Parth Mehrotra -- President and Chief Operating Officer
Yeah, definitely. So the data we typically get is lagged, as you know. So the data we get now is reflective of our performance in the performance year 2021. It's still early stages for the new ACOs, but all the data we received is reflected in our accruals.
And as we stated, that's a little bit ahead of our expectations, and that's reflected in the financial statements, and then both the top and the bottom line. So I think we've -- we expect to perform pretty well when it's all said and done. By the time August comes, and we get the final true-up, and hopefully, our accruals are reflecting that. As far as the new ACOs are concerned, again, pretty early stage.
We just got started Jan 1, so we'll continue to get that data over the course of this year. And we'll reflect that appropriately in our guidance.
Whit Mayo -- SVB Leerink Partners -- Analyst
OK, great. Thanks, guys.
Operator
Thank you. Our next question comes from the line of Jessica Tassan from Piper Sandler. Your line is now open.
Jessica Tassan -- Piper Sandler -- Analyst
Hi, good morning. Thank you for taking my question. So I just have one quick one on the implemented provider count and then a follow-up. So on implemented providers, you guys announced Montana in early February.
Can you just confirm whether or not those 65 Montana providers are now included in the implemented provider count?
Parth Mehrotra -- President and Chief Operating Officer
Yeah. Hey, Jess. So they're expected to be implemented at some point in Q2, so they'll likely be reflected when we report our Q2 results.
Jessica Tassan -- Piper Sandler -- Analyst
Got it. That's helpful. And then just maybe any comments on fee-for-service volume trends 2Q quarter to date relative to 1Q? And then maybe just on a historical basis, I don't know if we should be thinking about fee-for-service practice collections per provider as normal in 2018 or 2019, but comping 2Q quarter to date relative to historical periods would be helpful. Thank you.
Parth Mehrotra -- President and Chief Operating Officer
So we continue to see the trend with utilization well above our expectations. That continued from Q4 last year into Q1 this year, and nothing's changed in the first couple of months here in Q2. So hopefully, that continues. Again, we like to be conservative.
It's been tough to predict these last 24 months. But hopefully, that momentum continues. But we are well over pre-COVID baselines by wide respect. We think our practices are gaining market share on a same-store basis given the strength of the platform and the strength of these practices during that time.
So I think we see a lot of momentum. And hopefully, that continues.
Jessica Tassan -- Piper Sandler -- Analyst
Got it. Thank you.
Operator
Thank you. Our next question comes from the line of Sandy Draper from Guggenheim. Your line is now open.
Sandy Draper -- Guggenheim Partners -- Analyst
Thanks very much, and good morning. Just -- I think still a clarification here. I'm not quite sure. I think you may have addressed it, but I didn't quite get it, so I apologize.
Looks like in the first quarter, your care margin was about 12.7%. But if you look at your full year guidance, you're -- it applies close to 13.5%. So when we're thinking about that trending up, just remind me, what are the key drivers? And do you expect that to be linear? Or are there any sort of notable quarters where you get true-ups for any of the capitated lives or shared savings where you have a big jump that pushes that up and then it comes back down? Just trying to think about pacing that line and the trajectory going from 12.7% in the first quarter to get to sort of a 13.5% for the year. Thanks.
Parth Mehrotra -- President and Chief Operating Officer
Hey, yeah, Sandy, thanks for the question. So the trend should pretty much mimic 2021 or previous years, where you'll see it's low in the beginning of the year and then ramps up by Q3. The one thing that does get trued up is our estimates for prior periods when we get most of our value-based care results later in the year, sort of if there's a big deviation on the positive side, you should see that care margin as a percentage of practice collections trend up. Obviously, we entered the capitated arrangements this year, so we are accruing for those and not expecting much to flow down to care margin from those this year.
So there will be some anomaly driven by that. But again, that should be the trend, and that's reflected in the guidance.
Sandy Draper -- Guggenheim Partners -- Analyst
Great. That's helpful. And then a follow-up, and this relates to I think some of the questions there at the beginning. One of the ways I look at it is practice collections per provider, and that was up really nicely on a year over year and sequential basis.
Should we generally think about outside of a really big add that, that should be the level you think you saw this quarter of practice collections per provider, should be relatively stable, unless, obviously, if you add a big chunk of providers, you may actually see this state based on the math it dropped down a little bit? Or is there anything that wasn't related to the individual providers? Again, going back to some of the shared savings or other stuff that maybe not be purely provider-based to think about which is buildings that out. Thanks.
Parth Mehrotra -- President and Chief Operating Officer
Sure. So generally speaking, it should be stable accounting for any healthcare inflation or contractual adjustments that we have on the fee-for-service book. I do think it should be important that you separate out the capitated revenue and then calculate that number from the practice collections because that started this year. So there will be a big jump in practice collections due to those capitated arrangements.
So I think once you normalize for that, you should see a fairly stable trend ticking upwards slightly. But hopefully, that should remain fairly stable over time.
Sandy Draper -- Guggenheim Partners -- Analyst
OK. Yeah, that's helpful. So I guess we'll wait for the queue and make those adjustments and do that going forward. Thanks, Parth.
Operator
Thank you. Our next question comes from the line of Adam Ron from Bank of America. Your line is now open.
Adam Ron -- Bank of America Merrill Lynch -- Analyst
Hey, thanks. Going back to the discussion about multi-specialty groups and the comparison to Optum Care, you, too, I guess, are one of the only ones that I cover at least in value-based care that are connecting, both primary care assets and specialists. And you mentioned that it creates some synergies in value-based care. But to me, I still don't really understand how exactly that works.
Like it makes a lot of sense on the commercial side to add scale and get negotiating leverage and higher unit costs. And you mentioned utilization being stronger than you expected. So how exactly is it creating efficiencies on the value side? And do specialists get any of the shared savings, for example?
Parth Mehrotra -- President and Chief Operating Officer
Yeah. Good question, Adam. So I'll start, and Shawn will add. So look, fundamentally, what we recognize is in any value-based arrangements, 80% of the cost downstream from a primary care provider are largely fee-for-service.
So whether it's the specialist, it's facilities, inpatient, outpatient, and obviously, the drug spend. And the strategy is, therefore, to have a broad delivery system that can impact some of that cost trend with alternative site of care strategies, lower-cost, higher-quality specialists, and so forth. But then, more importantly, play a value-based theme, where the primary care provider may not be fully at risk in pools like the commercial pool that we have or even in upside-only MSSP, where the primary care provider doesn't need to take full risk, but you're impacting enough of the cost trend that is accruing to the payer of healthcare. I think that's our strategy going in.
And then obviously, we do participate in bundles, in programs like that, where appropriate, where the specialists can really impact with an alternative site of care strategy. It's something we're looking closely with our partnership with Surgery Partners, as an example. So obviously, that helps us participate much more broadly than most.
Shawn Morris -- Chief Executive Officer
Adam, this is Shawn. So if you think about kind of just at a high level what we do, we build medical groups. They're always primary care focused. That's where the attributed lives come from, over 80 value-based arrangements.
But at the end of -- and primary care focus that's what we're always going to be. But at the same time, as we build these medical groups, we're very strategic about when we begin to see density in a market, in a state, what type of providers should we be adding, depending on the level of risk we're taking and what that cohort of patient looks like. And I'll give you an example of Medicare Advantage. As we get dense and build density in a certain geography, the -- you'd say there's five to six specialties that you really want to -- you want to, I guess, get the right volume to the right providers, think about sites of service and ambulatory surgery, all those type of things that are the levers of just traditional -- any kind of traditional managed care.
But our primary care physicians have compact, as what we say, with these types of doctors. And then we are kind of looking to add those specialists to our group. So you're beginning to manage the professional risk. And then you have a huge input, I guess, outcome then on the institutional pools.
And so that's when we really -- when we talk about taking risk in a thoughtful manner, that's what we're talking about. We -- maybe it's primary care risk initially, but then we're moving upstream to professional and then 50-50 and really starting to kind of think about how we impact that institutional pool. And we've been very open about -- we think, the best long-term, most sustainable arrangements are where the payer is accepting risk with us, and they have incentives to build the right benefit structure for their patients. They have incentives to go out and get the most competitive arrangements with the acute care facilities and so on.
So that's what we -- I mean, we're in the business of building highly aligned, primary care-focused medical groups that can take care of every type of patient, regardless of the type of program they're in. I hope that's helpful.
Adam Ron -- Bank of America Merrill Lynch -- Analyst
Yeah. No, it is. Appreciate it. And then one more follow-up to what you said earlier.
You said that you wouldn't expect practice collections per doctor, I think, to rise over time, aside from cost inflation. But my understanding was that you were helping the doctor build out their patient panels and maximize revenue and lift their rates. So why wouldn't that number trend up significantly over time?
Parth Mehrotra -- President and Chief Operating Officer
Yeah. Over two- or three-year period, you should expect that to happen, absolutely. On a quarter-by-quarter basis, you would not see that kind of movement. And again, you'll have to, as I mentioned, to Sandy, separate out the value-based components.
So if you're looking at just the fee-for-service line, obviously, there's a good uptrend when the doctors join us, and then it stabilizes and then accretes up with better productivity and with any contract adjustments that we have. Again, at our size, with 3,300 providers, it's a much more stable metric now than it was a few years ago. But again, it's impacted by specialty mix and the maturity of each of our markets.
Adam Ron -- Bank of America Merrill Lynch -- Analyst
OK, got it. Thanks.
Operator
Thank you. Our next question comes from the line of David Larsen from BTIG. Your line is now open.
David Larsen -- BTIG -- Analyst
Hi. Congratulations on the good quarter. Can you talk a bit about the nature of the value-based care deals that you're working in? We've heard from Washington, there's a little bit of exhaustion from legislators around like the provider relief fund and sending dollars to providers. There's sequestration where, I think, there was a 1% thing in April.
There's another 1% thing in July, and there's less sort of tolerance for upside-only risk deals. How is that impacting your book, if at all, or your provider clients? Is it a headwind? Or is it actually a tailwind? Thanks.
Shawn Morris -- Chief Executive Officer
David, thanks. This is Shawn. I mean, we talk a lot about -- it's important and the type of providers that are attracted to Privia. They want value-based arrangements across their whole panel.
And I mean, when that gets into the 80-plus, it gets into -- today, if you look at these, kind of breaking those pools out, commercial tends to be across the country upside. And I can tell you, if you're any sophisticated provider and you're doing well, you're wanting to move upstream. And so payers are coming to you and say, "Hey, how can we share risk in certain corridors or in some way in the commercial?" So that -- there's discussions about that. We have those discussions.
So then you take -- you start breaking down the other Medicaid. Medicaid tends to be upside. It's very state-specific, what opportunities you have, what -- how you can affect that. Then you get into the Medicare population.
You break that out into two buckets. Obviously, we've been in the government business a long time. The team here at Privia has a lot of experience in government programs. We like them.
We break those out, and then we participate in MSSP. A lot of discussion about the success recently by CMS being pretty vocal about kind of stopping, doing as many programs that they don't feel they're getting shared -- or getting savings for the taxpayer and doing more of the programs that are being successful. We've been in MSP, I guess, since the beginning, seven years ago, really successful, have the No. 1 out of the top 100 ACOs in the Mid-Atlantic and in the shared savings percentage.
So a lot of success there. Medicare Advantage team has a lot of that. We've moved into that. But I think what you -- and this is me speaking, I don't want to speak for CMMI and CMS.
But they're narrowing their programs. We support that the -- because these programs are built over decades. They're not built over two or three years. And we think that, as these programs continue to improve, you'll see us in those programs.
We're going to do analysis. And should we move our positions in from one program to the next, we do that with our doctors. They're sharing risk with us. They're putting enough money, and they have skin in the game.
So we're very thoughtful in how we move from program to program, and we were measuring the headwinds and the tailwinds when we make those decisions. So -- but we're pretty supportive of the decisions that's coming out of CMS now, and that we be very thoughtful, be very supportive, continue to improve upon the programs. I think the other thing I haven't mentioned is there -- I think you'd agree what they're saying is they'd like to see more, I guess, similar -- the payer -- the commercial payers doing programs such as they are. And I think you're going to start seeing some of that where there are programs -- I don't want to say the quality metrics are the same, but they're going to be upside.
And CMS has -- you're seeing they want -- they start off upside, but they want you to move to risk. And to your last question, I think that's exactly what we're built to do. We're very thoughtful about it. And maybe we're kind of monotonous in our discussions, but we -- that's what we believe.
The worst thing you can possibly do is take risk too soon and fail, and you set yourself back with doctors and they lose confidence. So this is -- we're very supportive of what they're out there saying and the way they're taking the programs.
David Larsen -- BTIG -- Analyst
OK, great. Thanks very much. And then just one more quick one. There's a lot going on in the market with inflation, labor costs, rising interest rates and a slight pullback in the stock market, which I imagine is impacting the physician groups that probably have their capital invested in the market.
How is that impacting volumes to your practices and your cash collections? And like how our April -- March, April, May volumes, how do they compare to January? Did you get a bump up from COVID in January, and that's what drove the sort of cash collections upside? Or are you just sort of seeing continued strong volumes as we progress through the year?
Parth Mehrotra -- President and Chief Operating Officer
Yeah. I think it's two things for us. One is, obviously, we continue to see utilization much higher than what we expected. So as the world normalizes, and we're seeing that come in much, much stronger, we said that last quarter, we see the same trend continuing.
So that's obviously helping on the fee-for-service book. We also think our practices are gaining market share on a same-store basis, and that's reflective of how well they're doing with us, with our platform. We're able to enhance productivity, and they're able to add patient panels and so forth, add other providers to the same practice. So I think that's helping us on a same-store basis.
And then, look, the model today is really set up well where we're seeing this flywheel effect with our existing physicians asking their colleagues to join an entity like Privia, where there are all these challenges, complexity of value-based programs, the infrastructure, the technology stack and so forth. And I think independent physicians are realizing our model of being best of both worlds, where they bought something bigger, yet maintain their autonomy and are supported by a bigger entity from all of these things and have a real governance structure around our singleton medical groups. It gives them this best of both worlds dynamics, which is hard to get relative to selling their practice to somebody, whether it's a health system, whether it's a private equity entity, and so forth. So I think we're seeing all that momentum our way in terms of -- and that's all reflected in the growth in the financial statements.
Shawn Morris -- Chief Executive Officer
Yeah. Parth's last point was what I was going to kind of add on, was -- I mentioned in my prepared remarks, we spent -- I spent time at the NASDAQ with 17 of our physicians we invited. And there's no -- no one is immune to what's going on in the inflationary markets we are seeing. But it does -- it's reflecting on kind of, I think, our growth where physicians are -- they're seeing pressures that they probably haven't seen in the last few years.
And our physicians have performed really well. They understand value-based care is in their market. They want to perform better. Their peers are seeing them being successful, and they're telling their peers about it.
And a lot of our pipeline is full of where our providers have spoken with their colleagues about joining. So they're not immune to it. And I guess, in an odd way, it's driving some and fueling some of the -- I guess, some of our growth, if that's helpful.
David Larsen -- BTIG -- Analyst
Great. Thanks very much. Congrats on a good quarter.
Shawn Morris -- Chief Executive Officer
Thank you.
Operator
Thank you. Our next question comes from the line of Richard Close from Canaccord. Your line is now open.
Parth Mehrotra -- President and Chief Operating Officer
Richard, the one thing I'll add is we offer something to also health systems and other facility affiliated or employed providers, as we mentioned. And as you know, they are facing a lot more of these pressures in a much more acute manner than the -- in the community independent doctor practices. So if you -- obviously, the staffing issues, inflationary pressures in the hospitals, and so forth. I think 40%, 50% of the providers are in that ecosystem in the country today.
And our ability to offer and partner with health systems and entities, like Surgery Partners as an example, is also really positive for our business as we go through this period.
Shawn Morris -- Chief Executive Officer
That's a good point, Parth. It's just -- these discussions have really grown over the last 18 months. And I think the pressures of COVID and now the inflationary factors we're seeing are going to continue that momentum.
Richard Close -- Canaccord Genuity -- Analyst
Do you think that if valuations come down from the perspective of selling your practice that ultimately, that benefits you guys in terms of deciding to partner with someone like yourself? Is that a tailwind for you?
Parth Mehrotra -- President and Chief Operating Officer
I think, in summary, it should be. We've obviously shied away from buying practices, as you know, in our model. We think that misaligns interest. So obviously, as physicians -- those who were looking to sell or are on the borderline and are not getting what they expected, I think it's a tailwind for us.
Richard Close -- Canaccord Genuity -- Analyst
OK. Thank you.
Operator
Thank you. Our last question comes from the line of Taji Phillips from Jefferies. Your line is now open.
Brian Tanquilut -- Jefferies -- Analyst
Hey, guys. It's Brian Tanquilut. All our questions have been answered. Thank you so much.
Appreciate it.
Parth Mehrotra -- President and Chief Operating Officer
Thanks, Brian.
Operator
Thank you. At this time, I'm showing no further questions. I would like to turn the call back over to Mr. Morris for closing remarks.
Shawn Morris -- Chief Executive Officer
Thank you, operator. I want to thank everybody for joining and listening in today. We're excited, as you can tell. We're looking forward to continue to execute at this high level through the remainder of '22, and we look forward to speaking to you again at the next quarter.I appreciate your continued interest and support of Privia.
Enjoy the rest of your day. Thanks.
Operator
[Operator signoff]
Duration: 50 minutes
Call participants:
Robert Borchert -- Senior Vice President, Investor and Corporate Communications
Shawn Morris -- Chief Executive Officer
Parth Mehrotra -- President and Chief Operating Officer
David Mountcastle -- Chief Financial Officer
Josh Raskin -- Nephron Research -- Analyst
A.J Rice -- Credit Suisse -- Analyst
Lisa Gill -- J.P. Morgan -- Analyst
Ryan Daniels -- William Blair and Company -- Analyst
Whit Mayo -- SVB Leerink Partners -- Analyst
Jessica Tassan -- Piper Sandler -- Analyst
Sandy Draper -- Guggenheim Partners -- Analyst
Adam Ron -- Bank of America Merrill Lynch -- Analyst
David Larsen -- BTIG -- Analyst
Richard Close -- Canaccord Genuity -- Analyst
Brian Tanquilut -- Jefferies -- Analyst