Image source: The Motley Fool.
Elevance Health (ELV 3.19%)
Q4 2022 Earnings Call
Jan 25, 2023, 8:30 a.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Ladies and gentlemen, thank you for standing by, and welcome to the Elevance Health fourth quarter earnings conference call. [Operator instructions] I would now like to turn the conference over to the company's management. Please go ahead.
Steve Tanal -- Vice President, Investor Relations
Good morning, and welcome to Elevance Health's fourth quarter 2022 earnings call. This is Steve Tanal, vice president of investor relations. And I am joined this morning on our earnings call by Gail Boudreaux, president and CEO; John Gallina, our CFO; Peter Haytaian, president of Carelon; Morgan Kendrick, president of our commercial and specialty business division; and Felicia Norwood, president of our government business division. Gail will begin the call with a brief discussion of some of the highlights of the quarter and year before turning to our recent announcement of the acquisition of Blue Cross and Blue Shield of Louisiana, and a number of other updates on key strategic initiatives.
John will then discuss our financial results and outlook for 2023 in greater detail. After our prepared remarks, the team will be available for Q&A. During the call, we will reference certain non-GAAP measures. Reconciliations of these non-GAAP measures to the most directly comparable GAAP measures are available on our website, elevancehealth.com.
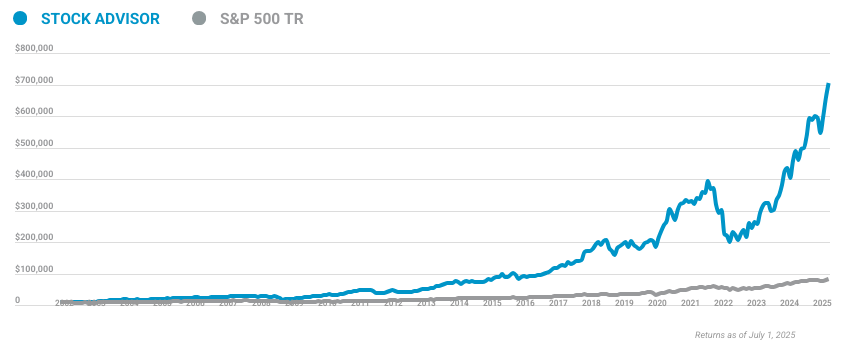
10 stocks we like better than Elevance Health
When our award-winning analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Elevance Health wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of January 9, 2023
We will also be making some forward-looking statements on this call. Listeners are cautioned that these statements are subject to certain risks and uncertainties, many of which are difficult to predict and generally beyond the control of Elevance Health. These risks and uncertainties can cause actual results to differ materially from our current expectations. We advise listeners to carefully review the risk factors discussed in today's press release and in our quarterly filings with the SEC.
I will now turn the call over to Gail.
Gail Boudreaux -- President and Chief Executive Officer
Thanks, Steve, and good morning, everyone. Today, we're pleased to share that Elevance Health delivered strong fourth quarter results, closing out another year of growth consistent with our long-term targets and considerable progress in our transformation to become a lifetime trusted health partner. In the fourth quarter, Elevance Health delivered GAAP earnings per share of $3.93 and adjusted earnings per share of $5.23. For the full year, we reported GAAP earnings per share of $24.81 and adjusted earnings per share of $29.07, reflecting growth of 15% year over year from our adjusted baseline of $25.20 in 2022.
2022 marks the fifth consecutive year in which we grew adjusted earnings per share within or above our 12% to 15% long-term target growth rate. This reflects the focused and sustained execution of our strategy to optimize our health benefits businesses, invest in high-growth opportunities, and accelerate capabilities and services. Elevance Health ended 2022 serving more than 47.5 million medical members of nearly 2.2 million members year over year, including more than 1 million new commercial and over a million new government members. Investments in enhancing the customer experience; delivering innovative, customized whole health solutions; deepening digital engagement; and prioritizing health equity all helped to deliver strong growth across customer segments.
Membership growth, coupled with expansion in both the scope and scale of Carelon's business with our health plans, helped to propel double-digit growth in CarelonRx and Carelon services. In total for the year, Elevance Health produced nearly 14% growth in operating revenue and double-digit growth in adjusted operating earnings. Now, I'd like to discuss a number of recent developments, including the acquisition of Blue Cross and Blue Shield of Louisiana that we just announced on Monday. Like our Anthem Blue Cross Blue Shield family of plans, Blue Cross and Blue Shield of Louisiana is deeply rooted in its local community, serving Louisianans for almost 90 years.
And like our health plans, Blue Cross and Blue Shield of Louisiana is committed to improving the health and lives of the people of Louisiana. Our organizations are well aligned in our mission and purpose, and have worked together in partnership through our Healthy Blue alliance, serving Medicaid and dual special needs plans in Louisiana for a number of years now. Upon closing, Blue Cross and Blue Shield of Louisiana will be our 15th Blue state, providing us with deep local roots and a new market, while we bring national scale and access to our portfolio of innovative solutions and capabilities to support the community. We're looking forward to accelerating Blue Cross and Blue Shield of Louisiana strategy to make an even greater difference in the health and lives of the 1.9 million individuals they serve.
Blue Cross and Blue Shield plans are at our best when we collaborate. Together, the blue system provides health benefits to nearly 115 million consumers across all 50 states. There are many untapped opportunities to leverage our unique scale. One recent example is Synergie Medication Collective.
Earlier this year, we became a founding investor in this new contracting organization founded by a group of Blue Cross and Blue Shield-affiliated companies. The collective focus is on improving affordability and access to medical specialty drugs that are injected or infused in a clinical setting. Synergie will seek best-in-class medical drug pricing, leveraging our collective industry-leading specialty drug spend to enhance affordability and drive toward value-based care, representing another example of Blues partnering for progress. Inside Elevance Health, we are also directly addressing fast growing areas of cost trend.
In November, we announced the acquisition of BioPlus, the largest independent specialty pharmacy provider, offering a complete range of specialty pharmacy services for patients living with complex and chronic conditions. BioPlus will enhance our ability to deliver on our whole health promise and enable us to leverage our resources and scale to deliver greater affordability and access to critical medications. Over time, it will allow us to bring specialty pharmacy fulfillment for our members in-house at what is a dynamic time in this field, given the anticipated growth of biosimilars. Upon closing BioPlus will become part of CarelonRx, our pharmacy services business that we rebranded at the beginning of this year.
With the addition of specialty pharmacy, we will expand the scope of the services and capabilities inside of Carelon and, by extension, the proportion of overall healthcare spending that we manage or address. The acquisition of BioPlus furthers our commitment to scaling healthcare services to address the needs of health plans, beginning with our own. Of Carelon's nearly $41 billion of revenue in 2022, approximately 60% came from partnering with our health plans. Meanwhile, in 2022, Carelon achieves the goal we set at our March 2021 investor conference of managing at least 20% of our consolidated benefit expense by 2025.
This is three years ahead of schedule, a testament to the growing suite of capabilities within Carelon. Carelon has made significant progress since our last investor conference, and we look forward to providing shareholders an update on our long range planning at our next investor conference, which will be held on Thursday, March 23, 2023, in New York City. Increasingly, we are evaluating and growing our enterprise through two primary businesses, health benefits and healthcare services. And we're continuing down the path of scaling Carelon by addressing the needs of our commercial Medicare and Medicaid health benefits businesses.
Beginning with the first quarter of 2023, we will evolve our external reporting to better align with this approach and begin to report Carelon split between CarelonRx and Carelon services, while we combine our commercial and government health benefits operations for reporting purposes into a single health benefits segment. Our new reporting structure will allow stakeholders to more clearly track the progress we are making against our enterprise strategy and better reflect how we evaluate our business results against our enterprise strategy today. John will discuss this more in his remarks, and you can also find a pro forma view of quarterly and full year 2022 results, the new reporting structure as a supplemental table in this morning's press release. Now, I'd like to touch on a few recent highlights before discussing our outlook for 2023.
During the fourth quarter, we were pleased to become the first managed care organization in the nation to earn the full three-year health equity accreditation from the National Committee for Quality Assurance for all of our own Medicaid health plans, covering nearly 90% of our Medicaid membership. This recognition demonstrates that focus and resolve yield results. We have long been dedicated to countering health inequities across our enterprise and through partnerships with care providers. We continue to work toward health equity through policy and practice in pursuit of better outcomes and experiences for all, and ultimately to improve the health of humanity.
Our Medicaid team is prepared to uphold that commitment by ensuring access to care for underprivileged populations through continuity of coverage for all beneficiaries eligible for Medicaid who will be subject to the eligibility redeterminations this year. We look forward to working alongside state partners to help minimize loss of coverage due to administrative challenges and to ensure beneficiaries no longer eligible for Medicaid understand their coverage options. Our ACA exchange plans are now being offered in almost every county in our 14 Blue states. We remain committed and prepared to ensure seamless transitions of those Medicaid members as they move into exchange plans or employer-based coverage.
Across our health plans, we are optimizing our businesses. The pandemic brought with it substantial uncertainties that resulted in margin compression in our commercial and Medicare health plans in 2021 that we didn't recover in 2022. It has since become apparent that COVID costs are not going to zero. And as we discussed last year, we've been repricing our risk in our commercial business, and we are enjoying improved reimbursement rates, risk adjustment revenue, and star-quality bonus payments and our Medicare Advantage business in 2023.
With January 1st renewals behind us in Commercial and the 2023 Medicare Advantage plan year underway, we remain confident in the margin recovery previously discussed and for the improvement in our commercial and Medicare businesses to more than offset anticipated member attrition in our Medicaid business when redeterminations begin on April 1st. Our confidence in operating our Medicare Advantage business, solidly inside our long term 3% to 5% target margin range, has been underpinned by our bid strategy in which we took a balanced approach. While the AEP proved to be somewhat more competitive than we expected, we still expect to grow Medicare Advantage membership relatively close to our prior targeted growth rate in 2023. Turning now to our outlook for 2023.
We expect adjusted earnings of greater than $32.60 per share, reflecting growth of over 12%. Our guidance reflects double-digit growth in operating earnings in each of our health benefits and Carelon businesses that will be driven by the focused execution of our enterprise strategy to optimize our health benefits business, invest in high-growth opportunities, and accelerate capabilities and services. Our outlook contemplates a range of outcomes on Medicaid redeterminations, coverage shifts and retention, and our expectation for commercial and Medicare margin recovery from pandemic era lows. John will discuss our assumptions in greater detail.
The strong growth we achieved in 2022 would not have been possible without the hard work and dedication of our more than 100,000 associates. Our collective determination to improve lives and communities is unwavering, and we look forward to making a meaningful difference at Elevance Health. I would like to thank them for the important work they do and the impact they make every day. Now, I'd like to turn the call over to John for more on our operating results.
John?
John Gallina -- Executive Vice President and Chief Financial Officer
Thank you, Gail, and good morning to everyone on the line. We are pleased to have delivered solid fourth quarter financial results, closing out another strong year of growth for Elevance Health. The focused execution on our enterprise strategy continues to drive progress against our stated long-term targets. Fourth quarter adjusted earnings per share of $5.23 was ahead of our expectations and drove full year adjusted earnings per share to $29.07, reflecting growth of over 15% year over year, off of our adjusted 2021 baseline of $25.20 and above our long-term 12% to 15% annual earnings-per-share growth target.
We ended the year with 47.5 million members, up 2.2 million or nearly 5% year over year, with organic growth having comprised more than 85% of our overall increase. In the fourth quarter, medical membership grew by 248,000 members, led by growth in Medicaid, driven in large part by the ongoing suspension of eligibility redeterminations and the acquisition of Vivida Health, which added 29,000 Medicaid members. For the full year, we had a 1.1 million net new commercial members and 1.1 million net new government members. Total operating revenue for the year was nearly $156 billion, an increase of approximately 14% over the prior year, reflecting solid growth in our health benefits businesses and continued momentum in Carelon.
We are pleased with the progress made to accelerate our service capabilities during the year as CarelonRx and Carelon services grew revenue by 12% and 27% over 2021, respectively. The consolidated benefit expense ratio for the fourth quarter was 89.4%, a decrease of 10 basis points over the fourth quarter of 2021. The strong performance includes an improvement in commercial underwriting margin and also benefited from the reclassification of certain quality improvement expenses. These improvements were partially offset by the Medicaid business, which carries a higher benefit expense ratio than our commercial and Medicare health plans.
Elevance Health's SG&A expense ratio in the fourth quarter was 11.5% and 11.4% for the full year, reflecting an improvement of 20 basis points in the fourth quarter and full year. These positive results include the negative impact on the SG&A ratio related to aligning certain volume improvement expenses with CMS guidelines. The overall improvement was driven primarily by expense leverage associated with strong growth in operating revenue. In 2022, we produced another year of strong operating cash flow of $8.4 billion, representing 1.4 times net income, which was significantly better than our outlook to start the year and was driven by stronger risk-based membership growth and maintaining a prudent balance sheet.
Additionally, relative to our initial guidance, a shift in the timing of certain payments to state-based partners added over 500 million to the fourth quarter operating cash flow that we now expect that we will pay in the first quarter of 2023. We ended 2022 with a debt-to-cap ratio of 39.9%, in line with our expectations and within our targeted range. During the fourth quarter, we repurchased 1.1 million shares of our stock for $567 million. For the year we repurchased 4.8 million shares for $2.3 billion, exceeding our initial outlook for 2022, as we took advantage of the volatile periods in the market and opportunistically repurchase shares.
Consistent with our approach throughout the pandemic, we maintained a prudent posture with respect to reserves. Days and claims payable ended the year at 47.7 days, an increase of 2.5 days year over year and stable with the third quarter. Medical claims payable grew over 15% year over year compared to premium revenue growth of 13.5%. In summary, 2022 was a very strong year.
We grew adjusted earnings per share by over 15%. We grew operating gain by nearly 13%. We grew membership by 2.2 million, and we grew revenue by nearly 14%, all with a stable medical loss ratio, a 2.5 day increase in days and claims payable; and operating cash flow of 8.4 billion or 1.4 times net income. Before turning to our 2023 outlook, I would like to provide more detail on our decision to adapt our external segment reporting to better align with our enterprise strategy.
Beginning with the first quarter of 2023, we will begin to disclose Carelon as a separate business division and provide operating revenue, operating gain, and operating margin information separately for Carelon services and CarelonRx. Carelon offers a diverse suite of services across behavioral health, advanced analytics and services, complex care, pharmacy services, and digital assets. And we remain committed to expanding the scale and scope of services Carelon provides to our own and third-party health plans. As we continue down the path of scaling Carelon by addressing the needs of our commercial Medicare and Medicaid health benefits businesses, it's become increasingly apparent that the similarities between our health plans have evolved to outnumber the differences.
And we have also decided to combine our employer, individual, Medicare and Medicaid health plans and products into a single health benefits division. The remaining segment, corporate and other, will include a small amount of revenue and earnings from non-Carelon nonhealth benefits businesses, as well as our corporate unallocated expenses. The new health benefits segment will combine the same group of businesses that currently comprises the commercial and specialty and government business divisions. And the Carelon services segment reflects the same group of businesses that comprised the diversified business group, now Carelon services, which has historically been included as part of our old other segment.
We are excited to begin disclosing the performance of our two primary and distinct businesses in a manner more consistent with how we will grow our enterprise for years to come and to be doing so at a time of strength for our organization. As you can see, our commercial health plan margin recovery is well underway and will extend into 2023, which is reflected in our health benefits segment margin guidance provided in our press release this morning. To ensure a smooth transition to our new reporting structure, we have also included a supplemental table in this morning's press release showing our quarterly and full year 2022 results, pro forma for the new reporting structure, alongside new supplemental performance metrics for CarelonRx and Carelon services that can be used to model revenue for each business. Our commitment to elevating whole health and advancing health beyond healthcare is unwavering.
And our new segment reporting structure will allow our stakeholders to more clearly track the progress we're making against our enterprise strategy. Now, I'd like to discuss our outlook for 2023 in greater detail. We are pleased to have provided initial earnings per share guidance of greater than $32.60, reflecting growth of over 12% year over year, putting us on track to produce a sixth consecutive year of growth in adjusted earnings per share, consistent with our long-term 12% to 15% compound annual growth rate target. 2023 will be a year of optimization, but we will also demonstrate the balance and resilience of our health benefits businesses as we execute the planned recovery of our commercial and Medicare health plan margins from pandemic era lows, which we expect will more than offset the impact of membership attrition and margin normalization in our Medicaid business when eligibility redeterminations resume.
By 2023, we anticipate growth in medical membership despite commercial repricing and Medicaid redeterminations. Commercial risk-based membership is expected in 2023, up over 200,000 at the midpoint, ending the year in the range of 4.9 million to 5.1 million members. Growth will be driven by individual and small group risk-based membership, partially offset by attrition, and our large group risk business, driven by the repricing discussed earlier. Note that we expect commercial risk-based membership to decline by approximately 60,000 in the first quarter, with individual up approximately 100,000 and group risk-based membership down approximately 160,000.
We anticipate growth in individual and group risk-based membership over the balance of the year, concentrated in the second half, as consumers transition from Medicaid to commercial coverage. Fee-based membership is expected to grow by approximately 600,000 members at the midpoint to 27.1 million to 27.4 million at year end 2023. The wider-than-normal range contemplates a variety of scenarios related to coverage shifts out of Medicaid and into employer-sponsored plans, and the relatively uncertain macroeconomic backdrop. We expect approximately one third of this growth to occur in the first quarter, with the balance more heavily concentrated in the back half of the year as consumers transition from Medicaid to commercial coverage.
Total commercial membership will end the year in the range of 32 million to 32.5 million members, up over 800,000 members at the midpoint. Medicare Advantage membership is expected to grow by approximately 75,000 to 125,000 members, with growth in both individual and group, pushing our membership over the 2 million member mark. Medicaid membership is expected to end the year in the range of 10.8 million to 11.3 million, driven by the attrition associated with eligibility redeterminations beginning on April 1st of this year. This wider-than-normal range contemplates a range of scenarios on the pace of redeterminations and the prospect of macroeconomic headwinds developing over the course of 2023.
And finally, we expect our Medicare supplement and federal employees health benefits memberships will be relatively stable year over year. In total, medical membership is expected to end 2023 in the range of 47.4 million to 48.5 million, reflecting growth of over 400,000 members at the midpoint. The consolidated medical loss ratio is expected to be 87.2% in 2023, plus or minus 50 basis points, an improvement of approximately 20 basis points compared with 2022, primarily driven by the repricing of commercial risk-based business and margin expansion and Medicare Advantage related to the improved reimbursement levels across rates, risk adjustment, and star-quality performance. The SG&A expense ratio is expected to be 11.2%, plus or minus 50 basis points, a reduction of 20 basis points at the midpoint, driven by expense leverage associated with growth in operating revenue, partially offset by continued growth in our Carelon businesses, which carry higher SG&A ratio in our health benefits business.
We expect operating gain for the year to be greater than $9.35 billion, reflecting growth of at least 10% over 2022, again, being the primary driver of growth in adjusted earnings per share. Below the line, we expect investment income to be approximately $1.6 billion and interest expense to be approximate $1 billion, both reflecting the impact of higher interest rates. And our effective tax rate is expected to be in the range of 22% to 24%. Our full year operating cash flow is expected to be greater than $7.6 billion, including the unfavorable impact of a timing delay on the payment of approximately 500 million to certain Medicaid state partners that we previously believed we would pay in the fourth quarter of 2022.
Adjusting for timing, our 2023 cash flow outlook would be greater than $8.1 billion or approximately 1.1 times are expected GAAP net income. We expect full year share repurchases of approximately $2 billion, and our weighted average fully diluted share count for the year is expected to be in the range of 239 million to 240 million shares outstanding. Our 2023 guidance does not include the pending acquisition of BioPlus or Blue Cross and Blue Shield of Louisiana, which we expect will close later in the year. Importantly, neither is expected to have a material impact on earnings in 2023.
At the segment level, we expect the health benefits segment operating revenue to grow in the mid to upper single-digit percentage range year over year in 2023 with segment operating margin of 25 to 50 basis points year over year. We expect CarelonRx revenue to grow in the upper single-digit percentage range with low single-digit growth in adjusted scripts and mid-single digit growth in revenue per adjusted script. And we expect Carelon services to grow revenue in the low double-digit range organically, excluding all pending or unannounced M&A, driven by growth in revenue per consumer served, as we expect consumer serve to grow in the low single-digit range from 105 million at year-end 2022. Carelon services operating margin is expected to expand by 25 to 50 basis points year over year in 2023.
With respect to earnings seasonality, we are projecting similar profitability patterns to historical ranges and expect to earn slightly more than 55% of our full year adjusted earnings per share in the first half of the year, with slightly more than half of that in the first quarter, consistent with current consensus modeling of seasonality. Finally, we remain committed to enhancing shareholder returns through capital deployment, including share repurchases and dividends, and are pleased to announce that our board of directors recently approved a 16% increase in our regular quarterly dividend to $1.48 per share, our 12th consecutive annual increase, which will be paid on March 24th to shareholders of record at the close of business on March 10th. In closing, 2022 was another year of strong growth for Elevance Health as we continue down the path of transforming from a traditional health insurance company to a lifetime trusted healthcare. And we are well positioned to deliver another year of strong growth in line with our long-term targets in 2023.
We look forward to discussing our enterprise strategy and long-term financial targets at our upcoming investor conference, which we will host in New York City on Thursday, March 23, 2023. And with that. Operator, please open the line for questions.
Questions & Answers:
Operator
[Operator instructions] Our first question will go to the line of Lance Wilkes from Bernstein. Your line is open.
Lance Wilkes -- AllianceBernstein -- Analyst
Yeah. Thanks. Can you talk a little bit about the growth in the services business, which is really interesting, both org changes that you're intending to put in place to kind of support the new segment reporting, if any? And then, in the care delivery aspect of that, can you just talked a little bit about what you've been doing today with some of your partnerships with Aledade and Privia, and how that's kind of being deployed in the market and what your expectations are for care delivery long term?
Gail Boudreaux -- President and Chief Executive Officer
Well, thanks for the question, Lance. Let me frame a little bit of what you asked, and then I'll ask Pete Haytaian, who leads Carelon, to give you a little bit more color on that. First, in terms of structure. We've actually been building our team over the last 18 months, and Pete's done a really strong job of both bringing individuals who are in the services industry to Carelon, but also taking individuals from our health benefits business who have a deep understanding of that business and having them leave.
So, we feel we've got a really good mix of talent and have been building our bench strength pretty effectively. So, we don't envision any structural changes. Obviously, as acquisitions come in, they fit into the verticals that we've shared as part of our strategy. Let me just have Pete comment a little bit more about Carelon and our growth there.
Peter Haytaian -- President, Diversified Business and IngenioRx
Yeah, no, thanks a lot, Gail. Thanks a lot, Lance, for the question. You know, overall, as Gail said, we're really pleased with the momentum and performance that we saw on 2022. And as Gail noted, you know, in the year, we did do a lot around restructuring.
We obviously went through rebranding, which there was a lot of excitement around. And as she said, we infused a lot of new talent across the organization. And then, in terms of the infrastructure we built internally, we're very focused. As you know, a core part of our strategy is focused on internal growth and serving Elevance-affiliated health plans.
And so, we built the infrastructure to engage and to a much better degree with our associates and partners internally. And we're seeing, you know, really good progress there. I hope you can see that through the numbers and the improvement in the year. We remain keenly focused on whole health and improving the patient experience.
That's something else that we're very focused on, looking from the outside in, in terms of the patient experience. And then, I'd say the other thing that we've been really focused on internally, and we're trying to change the culture and it's working, is driving more risk and capitation through the portfolio. And that has really helped in terms of the acceleration of our growth and the innovation that we're seeing, you know, going forward. As it relates to your question on some of the care delivery partnerships, we're seeing really good progress there.
Again, when you look at the assets within Carelon, it can add a lot of value to our partners. And so, we continue to look to wrap around those services and create incremental value. And as we look forward, you know, we have that in mind as well when we talk to our provider-based partners. Where are they feeling stress? Where can we support them? So, there's a lot of opportunity in that regard going forward.
Gail Boudreaux -- President and Chief Executive Officer
Yes. Thanks, Pete and Lance. Specifically, in terms of how we're deploying, we see those partnerships and some of the investments we've made as part of our overall value-based care strategy. Our penetration has been strong, around 63%, driven by purposeful collaboration.
Those are two really good examples. You know, we continue to learn and improve that approach. And part of that is how we work closely with Carelon to capitate services and actually, I think, impact more of the healthcare dollar and impact more of overall services. But we feel really confident about the strategy that we've deployed.
And as I've shared before on these calls, we know that sharing -- the downside risk is really the most important part of where we need to achieve better outcomes. And so, we're continuing to grow those arrangements early days still, but we feel good about the partnerships that we have. And we continue to expand them, and we feel on track to deliver on the goals that we've shared previously at our investor day, but also in these calls. So, thanks very much for the question.
And next question, please.
Operator
Next, we'll go to the line of A.J. Rice from Credit Suisse. Please go ahead.
A.J. Rice -- Credit Suisse -- Analyst
Thanks. Hi, everybody. Congratulations on the Blue Cross and Blue Shield of Louisiana deal. It's been quite a while since we've seen one of those.
My vague recollection is the approval process and navigating the regulatory side of things can be a little tricky. Can you give us a sense of any discussions you've had with the state to this point and your confidence level? I know you're saying by year-end close. And, John, you mentioned that it wouldn't be meaningful to this year's numbers. I'm assuming that's partly due to late closure.
But is it -- can we say that it would be accretive? Is there anything you can say financially about it? And then, the last aspect of this is, obviously, there's a lot of changing things related to the Blues generally with the antitrust settlement, etc. Are you seeing more discussions, Gail, as you're out there? Or is there more interest in collaboration, maybe we could see a broader upswing in activity?
Gail Boudreaux -- President and Chief Executive Officer
Well, thank you, A.J. That was a very comprehensive set of questions. And let me try to kind of go through them. First, you know, we really are excited about the acquisition of Blue Cross and Blue Shield of Louisiana.
As you said, it's been some time since one of these has occurred. But I think, you know, as you think about like the driver for this, this is very much a strategic acquisition. The board of Blue Cross and Blue Shield of Louisiana really wanted to have a greater impact and accelerate the strategy that they put in place. This is a solidly run plan, 4.5 star Medicare plan.
And I think those are really important things as you think about this acquisition. The other thing that I think is really important for us is Blue Cross and Blue Shield of Louisiana very much aligns with our strategy. They're deeply rooted in their local communities. You know, as we shared, they've served Louisianans for more than 90 years.
Our mission and purpose is well aligned. And we've had a Healthy Blue alliance partnership with them that serves our Medicaid and dual special needs plans for a number of years now. So, we've worked together culturally. I think there's a great alignment there.
And the other thing is, is, you know, we're excited because this brings the 15th Blue state. So, we can -- just as we have in our other 14, we've kept our deep local roots in the new market, but we also can bring our national scale and access to our portfolio of innovative solutions and capabilities, again, accelerating what the Blue Cross Blue Shield strategic focus has been, and that supports the community and, I think, accelerates their strategy in making an even greater difference and impact on the 1.9 million lives. In terms of closing, you know, this will be subject to the normal closing conditions. And as we shared, we believe that we expect the deal to close in the second half of 2023.
So, again, not much more there. We do feel, you know, the impact that we have on the community and the citizens of Louisiana with the foundation accelerate Louisiana really as a strong component of this and helps accelerate healthcare status, accessibility, affordability, as well as health equity in those are areas that we've been deeply investing and committed to as well. In terms of collaborations, you heard that we've done a number of collaborations and feel good about the Synergie Medical Collective, which is a great example of all of us coming together around medical specialty and, again, with an alignment and focus around fundamentally improving affordability. We have 150 million Americans that we serve across this country, and we feel that ability for us to work together to have an even greater impact, again, on access and affordability is really important.
And I would just point to that as an example. So, thank you very much for the question. I think we again are excited about this. We think it's a great collaboration for us and feel that there's an opportunity for us to work together and for us to obviously use Carelon to help support the advancement of all Blues.
So, thanks very much. Next question, please.
Operator
Next, we'll go to the line of Justin Lake from Wolfe Research. Please go ahead.
Justin Lake -- Wolfe Research -- Analyst
Thanks. Good morning. I just wanted to check in. In 2022, you did about 7% margin in that commercial business.
I know you're not reporting it specifically anymore. But you had 11% target out there for 2025. Want to check in on that target and just find out if that is still what you're expecting to do by 2025. Maybe you could share with us how much progress you're making toward that in 2023.
And then, give us -- you know, I'm sure there's offset there in terms of more conservatism on the Medicaid side from a margin perspective. Can you share where you expect your Medicaid margins to be versus the 2% to 4% target you have out there long term? Thanks.
John Gallina -- Executive Vice President and Chief Financial Officer
Thank you, Justin. Good morning, and we do appreciate the questions. You know, in terms of, you know, commercial, you know, we're actually doing very, very well. You know, we have a repricing effort going on, you know, that began on July 1st of 2022.
And, you know, what we had seen was the overall cost structure of the commercial market was higher than we had assumed. And so, this repricing was about 25% of the large group block in July. And then, we repriced about 50% of the block here on January 1, 2023. And it was really to ensure that the premiums more accurately reflected the underlying cost structure of the book.
The result of that would be margin recovery associated with that. You know, we feel very good about the progress that we're making, and we still stand by the commitments that were made in our prior investor day to get the commercial margins up to the level that we estimated by 2025. You know, you have to look at now the health services segment in total. And, you know, as you had asked, we have the commercial margin improvement ongoing.
We will have Medicare margin improvement as our risk adjusters are really recovering, risk-adjusted revenue really recovering from pandemic era lows. Also, we do have 74% of our MA membership in 4-star plans are above for the 2023 payment year. And we believe our Medicare Advantage business will be solidly within the target margin range of 3% to 5%. And then, on Medicaid, which was your final question, you know, we've been working very closely with our state partners on Medicaid and feel very good about the rating actions and that the rates are actuarially sound rates, and feel very good about that.
However, you know, we were making either at or above the high end of our range here the last couple of years, you know, which obviously resulted in more collars and various other rebates being paid back to the states. We expect that the Medicaid business will be solidly within the 2% to 4% range, closer to the high end, but still with actuarial equipment equivalent rates. So, hopefully that helps clarify all that. Thank you.
Gail Boudreaux -- President and Chief Executive Officer
Thank you. Next question, please.
Operator
Next, we'll go to the line of Nathan Rich from Goldman Sachs. Please go ahead.
Nathan Rich -- Goldman Sachs -- Analyst
Hi. Good morning. Thanks for the questions. On Carelon, you mentioned that you hit the target for 20% of the benefit expense through Carelon ahead of schedule.
Can you talk about how much higher this percentage can go from here with your current capabilities? And then, specifically, on the outlook for 2023, the revenue guidance for Carelon services came in a bit below your long-term target. How are you thinking about growth from here, just given the progress that you've made? And will more growth come from external customers going forward? Thank you.
Gail Boudreaux -- President and Chief Executive Officer
Yes. Actually, I'm going to have Pete Haytaian provide a little perspective. And, you know, as we shared earlier, we are going to be updating our long-term planning at our investor day in March. So, we probably won't go into like where we think our updated guidance is on that, but we can certainly give you some color on how each of the components are playing.
We feel very good about the progress that Carelon overall is making. So, Pete?
Peter Haytaian -- President, Diversified Business and IngenioRx
Yeah, no, thanks for the question, Nathan. You know, as it relates to '23, just to be clear, and John noted this in the prepared remarks, that the low double-digit range growth in '23 is really organic growth. It does not include M&A. I think if you look at our recent history, there's been a lot of M&A that's contributed meaningfully to us.
And we're being very intentional about that. We're very focused on it. It's something that we'll continue to do, and I think it's an important part, you know, of our growth strategy going forward. As Gail said, you know, in terms of the amount of medical spend that we penetrate, we'll talk more about that at investor day, but we're really encouraged with our trajectory right now.
We feel like we can continue to grow pretty significantly. There's a lot of whitespace internally, so a lot of opportunity there. But to your point about external growth, we did establish some new leadership. We've got a new infrastructure in terms of external growth.
We're very focused as Gail said. We've heard a lot about the Blues and Blue partnerships, and we're very encouraged at what we're seeing in terms of the Blue opportunity. We do think we can see nice growth externally as well. But again, our first focus is on the affiliate health plans creating value there first.
Gail Boudreaux -- President and Chief Executive Officer
Thank you. Next question, please.
Operator
Next, we'll go to the line of Scott Fidel from Stephens. Please go ahead.
Scott Fidel -- Stephens, Inc. -- Analyst
Hi. Thanks. Good morning. I just had two follow-ups on the Blues topic.
The first is if you can maybe give us some color on the incremental revenue you expect to drive from the BCBSLA Louisiana acquisition because, obviously, you already have some revenues that you're generating off of Healthy Blue. Then, also, maybe just an update on the Blue Cross and Blue Shield of Minnesota situation. I think that that relationship on the Medicaid side will term at the beginning of 2024. Just any update on membership or financial impact that you expect from that situation as well.
Thank you.
John Gallina -- Executive Vice President and Chief Financial Officer
Yeah, sure. Thank you, Scott, for the question. So, you know, associated with, you know, with Blue Cross and Blue Shield of Louisiana, as we had stated, we're not expecting that to close until later in 2023, will not be material, really down the line items. However, assuming it does close in '23, 2024, what we should see is an incremental 1.6 million members after you eliminate the various double counts, and you reference the significant partnership we have with them already.
So, it's an incremental 1.6 million members, and it's really an incremental 4.5 billion in revenue on top of what we have now. So, that's really the high-level economics that we would expect to incur in 2024.
Gail Boudreaux -- President and Chief Executive Officer
I'm going to ask Felicia Norwood to comment on Minnesota.
Felicia Norwood -- President, Government Business Division
Yes. Good morning, Scott, and thank you for the question on Minnesota. You know, we operate over 27 Medicaid plans across the country with over 11.5 million members. And when you think about what we do, we bring very deep expertise in this business and a relentless focus on our whole health strategy, health equity, and improving health outcomes.
The expertise we bring to the table has been recognized by our external partners, and we really look forward to continuing to bring that experience to other Blue partners and alliances, not only in Medicaid but in Medicare as well. When I think about our alliance relationships, each of them is very different. And Blue Cross and Blue Shield of Minnesota decided to end our administrative services relationship, which supported about 330,000 Medicaid members and provide back-office services in-house. You know, we're going to work with them to make sure that there is a seamless transition because at the core of what we do, we want to make sure our members are taken care of, and that's our highest priority.
So, we continue to value alliance relationships and really look forward to continue growth in this segment with partners who value the deep expertise that we bring to the table for serving vulnerable and complex populations. Thank you.
Gail Boudreaux -- President and Chief Executive Officer
Yeah, thanks, Felicia. And, Scott, that will be in January 24, just from a timing perspective. Next question, please.
Operator
Next, we'll go to the line of Lisa Gill from JPMorgan. Please go ahead.
Lisa Gill -- JPMorgan Chase and Company -- Analyst
Thanks very much. Good morning. I just wanted to follow up on utilization expectations for 2023. John, you made the comment that COVID is not going away.
I agree that that should be in the baseline. But as we think about this, do you feel like there's any level of pent-up demand or potentially higher acuity levels as we move into 2023? And would you call out any specific line of business?
John Gallina -- Executive Vice President and Chief Financial Officer
Thank you for the question, Lisa. You know, we're not discussing specific trend assumptions for 2023, but, you know, really, when you look at some of the cost drivers that we have relative the expectations, you know, emergency room has been favorable, inpatient has been favorable, pharmacy cost actually running a little bit higher than expected, and outpatient is running a little bit higher than expected. I don't know that we really see any pent-up demand as much as we see, you know, being as much of the new normal. But, you know, just to reiterate, you know, the overall cost structure of the business is higher than if COVID had never occurred.
COVID is here, and it continues to be a cost driver. What I think is probably most important in all of this is that our pricing now reflects the underlying cost structure. And our MLR guidance also reflects this higher cost structure. So, we are very well positioned going into 2023.
Thank you.
Gail Boudreaux -- President and Chief Executive Officer
Next question, please.
Operator
Next, we'll go to the line of Kevin Fischbeck from Bank of America. Please go ahead.
Kevin Fischbeck -- Bank of America Merrill Lynch -- Analyst
Great. Thanks. I guess my question is going to be really on 2024, so if you can make a direct comment on that, that would be great. But if not, at least comment on the 2023 trajectory to give us a little bit of a sense.
Because it seems like the story here for 2023 is balanced portfolio improvements in commercial and Medicare are offsetting Medicaid, but, obviously, the Medicaid pressure is one that builds throughout the year, both from a revenue and, I would think, from an MLR pressure perspective, which begs the question about whether it's a bigger headwind in 2024 than it is in 2023 and whether there are similar opportunities in 2024 to kind of -- to offset that. Thanks.
John Gallina -- Executive Vice President and Chief Financial Officer
Yeah, thank you for the question, Kevin. And as you indicated in your question, we're not going to provide any specific details or data on 2024. Obviously, at our investor day, coming up here in a few months, we'll provide a lot more long-term aspirations. But I think the way you've characterized 2023 is correct.
Really, it's a year of optimizing our health benefits business while we continue to grow and expand the capabilities within Carelon. I think you talked about, well, gee, could the headwind be greater? You know, as you look at the Medicaid redeterminations, there's certainly a lot of variables associated with the pace and timing on a state-by-state basis, where they go, which lines of business they ultimately reside in. I think one of the great things about the balance and resilience of our membership base is that, you know, we end up with the members somewhere. We have a product offering for every member, regardless of age, regardless of employment status, regardless of health condition.
And I feel very, very good. So, you know, we do expect approximately, you know, about half of the Medicaid members to be reverified here in this calendar year and the other half next year. So, there is, you know, some balance there. But at the end of the day, we are very well positioned to retain much of that membership.
Thank you.
Gail Boudreaux -- President and Chief Executive Officer
Yeah. Thanks, John. And, Kevin, I think it's an insightful question because as you've heard us talk about, I think there's three core pillars of how we see our business evolving. You know, optimizing our health benefits business, it's highly scaled.
We're very diversified in that business. And again, as you think about 2023, we have an opportunity for margin recovery, which is really we've been intensely focused on. But the other two pillars, I think, are really important about our future growth, which is investing in growth opportunities. And then, third, accelerating services and capabilities, particularly through Carelon.
And remember, as we think about Carelon, a lot of that is synergistic with our health plan business. We continue to grow that health plan business, and that allows the synergy to also occur with Carelon' services, as well as expanding capabilities that you've seen us get through organically and inorganically. So, overall, I think we've got more levers than we've ever had historically, and those position us well for the balance that John just shared. Next question, please.
Operator
Next, we'll go to the line of Stephen Baxter from Wells Fargo. Please go ahead.
Stephen Baxter -- Wells Fargo Securities -- Analyst
Hi. Good morning. It'd be great if you could expand a little bit on the dynamics you saw in Medicare Advantage open enrollment this year and how you think those trends might play out over the next couple. And then, specifically, hoping to clarify the enrollment expectations there.
I think you said 75,000 to 100,000 membership growth. Is that a sequential Q1 figure or year-end figure? Just trying to realign versus the previous expectations you've shared here. Thanks.
Gail Boudreaux -- President and Chief Executive Officer
Sure. I'll have Felicia Norwood, who leads that business, share her comments.
Felicia Norwood -- President, Government Business Division
So, good morning, and thank you for that question. You know, when we think about Medicare Advantage, you know, as Gail mentioned in her early remarks, we took a very strategic approach as we thought about our bids for '23. And we expect to deliver a good performance in terms of growth, not just in individual but also in group. As John referenced, we plan to grow between 75,000 and 125,000.
But we did end up encountering a very competitive AEP. On the other hand, we had very solid growth in our D-SNP business, which is where we've had a focus for some period of time. And I think that positions us well for the rest of OEP and the remainder of 2023. As we think about our competitiveness, we have a very strong benefit portfolio, and we believe that we're positioned well in order to continue to grow this business.
So, at the end of the day, you know, a competitive environment, which is always will be in Medicare Advantage, but still an opportunity to grow and a business that we feel very good about. And most importantly, the opportunity is we -- in 2023, to deliver a very strong margin recovery and operate squarely within our 3% to 5% pre-tax target margin range in this business. So, solid growth and solid margins in 2023.
Gail Boudreaux -- President and Chief Executive Officer
Thank you. Next question, please.
Operator
Next, we'll go to the line of Josh Raskin from Nephron Research. Please go ahead.
Josh Raskin -- Nephron Research -- Analyst
Hi. Thanks. Good morning. I was wondering if you could provide an update on some of the trends you're seeing in value-based care.
I heard some of the comments earlier. But as you go into 2023, are there any changes, you know, in the dynamics of the industry? Any changes specify in contracting terms that either the providers are looking for or that you're trying to push? And then, maybe any updated views on the employment or ownership of physicians or physician groups.
Gail Boudreaux -- President and Chief Executive Officer
Well, thanks for the question, Josh. In terms of -- a little bit consistent, I guess, with what I shared before on value-based care, I mean, we've been -- we continue, quite frankly, to refine and improve our strategy. We feel we're making really good progress on it. You know, what we're seeing is a lot more interest in sharing up and downside risk.
Historically, value-based care was more upside risk, and we've gotten about 63%. We've gone -- we've continued to refine that to now include much more downside risk. And also, I think one of the biggest differences is the sharing of data bilaterally and much more timely. So that action can be taken, I think, in a much more integrated way.
And we're doing a lot of work with that with our care providers. It's embedded. And also, what happens, like, post primary care. So how do we manage all the specialty services? That's a big part of the Carelon strategy in terms of what Pete is doing in his business.
So, as I think about that, you know, I would say, structurally, we're seeing a lot more interest and a lot more conversation as this takes several years for, I think, physician practices to get comfortable with value-based care. And so, we're building credibility with that. We're getting better at our reporting and our engagement. And we're not only doing it across Medicare Advantage, and I think that is one of the changes.
Some of our relationships are specific to commercial, for example, and that's a very different approach, including with some fee-based customers. So, that would be a trend. In terms of the ownership of physicians, I think, we've been very consistent about that. We do own physicians in terms of our integrated health plans.
And those have performed very well in MMM and Healthfund in Florida. I think CareMore is beginning to become even more integrated with the work we're doing. So, I think our strategy has stayed very consistent there. So, I don't really have any significant updates other than I think it's all embedded in our ability to drive more downside risk, integrate data in a much more real-time basis, and then, really, become true partners and train each other and how do we work in a value-based care environment.
As, I think, you know well, this doesn't happen overnight. And it takes quite a bit of work for us on both sides to be committed to the long-term partnership. But we feel good, and we're seeing more enrollment in those partnerships. And the results have been good.
We see differentiated quality and cost outcomes. So, thank you very much for the question. Next question, please.
Operator
Next, we'll go to the line of Rob Cottrell from Cleveland Research. Please go ahead.
Rob Cottrell -- Cleveland Research Company -- Analyst
Hi. Good morning. Thanks for taking my questions. Just on the CarelonRx or PBM, how should we square the high single-digit outlook for 2023 relative to your long-term 2025 low double-digit outlook? And then, also, can you provide a bit more color on what Carelon's role will be within the Synergie Collective? Thank you.
Gail Boudreaux -- President and Chief Executive Officer
I'm going to ask Pete Haytaian to address that, please.
Peter Haytaian -- President, Diversified Business and IngenioRx
Yeah. Thanks. In terms of the short term, if you're referencing the script growth, you know, overall, we're going to see nice script growth in Medicare and commercial. In terms of the headwind to that, really, that's due to the Medicaid dynamic around reverifications or redeterminations.
And then, overall, you know, we're going to see lower COVID vaccination. So, that doesn't impact operating gain, but that is really the reason for the difference in the numbers in terms of what you're seeing short term, you know, long term. In terms of overall growth, though, we feel really good about, you know, how we're doing in the pharmacy business. There continues to be a lot of interest in our integrated value proposition.
In 2022, we're coming off a good year. We saw a 300% improvement in net membership growth. So, that was good in terms of penetrating our self-funded business. And we're seeing that continue to play through into 2023.
Where -- obviously, through a lot of the selling for the beginning of the year, what we did see is we saw a lot more activity and penetration in the 10,000 or less business. We saw RFPs up by about 6% year over year. And again, I'll reiterate that this is a segment, an area that we perform really, really well in. I think you referenced Synergie at the end of your question.
And again, to Gail's point in our commentary, our focus -- you know, a big part of our strategy is overall affordability and choice. And this creates an opportunity for us in the context of medical specialty to create more affordability for our members. Again, by working in conjunction with the Blues across 100 million Americans, those that are utilizing specialty on the medical side, we have an opportunity to create much greater affordability. So, we look forward to that.
That work is in earnest right now in 2023 with value potentially playing through into 2024.
Gail Boudreaux -- President and Chief Executive Officer
Thank you. Next question, please.
Operator
Next, we'll go to the line of Whit Mayo from SVB Securities. Please go ahead.
Whit Mayo -- SVB Securities -- Analyst
Hey, just on the topic of health plan optimization and commercial repricing initiatives, can you comment maybe more specifically on stop-loss? You know, I think, you guys are beginning to anniversary some of the challenges in the creep and high-cost claims last year. Just how you feel about trends in the business margins, just maybe broadly any comments about the overall stop-loss market? Thanks.
Gail Boudreaux -- President and Chief Executive Officer
Sure, Whit. I'm going to have Morgan Kendrick, who leads our commercial business, give you some perspective there.
Morgan Kendrick -- President, Commercial Business
Hi, there, and, Whit, thank you for the question. You know, regarding the stop-loss business, that's certainly an area that was underperforming priorly. And we began that journey to recover the margins in that business back in January of last year. It started with some of our integrated -- our external business rather.
And then, year progressed further, we had our July cohort, which John mentioned earlier, which was about 25% of our integrated business, both stop-loss and risk-based business. Both of those went through a repricing exercise midyear, and then that concluded with January. So, regarding the stop-loss market, we feel very good about it. We've got continued strong penetration but opportunity to continue to grow that, both on our internal integrated business, as well as our external.
And we feel, at this point in time, we have right-priced our business based on risk, and we'll continue doing that so very fastidiously as we move through in 2023.
Gail Boudreaux -- President and Chief Executive Officer
Thank you. Next question, please.
Operator
Next, we'll go to the line of Dave Windley from Jefferies. Please go ahead.
Dave Windley -- Jefferies -- Analyst
Hi. Thanks for taking my question. Good morning. You called out a headwind to the MLR this year from the growth, the outsized growth in Medicaid, did not call out a benefit to the SG&A ratio in 2022 from that.
I'm wondering if there was one. And then, more importantly, as the direction of those books reverses and Medicaid shrinks in 2023 from redetermination, does that create a headwind? And what levers are you pulling to offset that headwind for SG&A ratio? Thanks.
John Gallina -- Executive Vice President and Chief Financial Officer
Thank you for the question, Dave. You know, as you can imagine, there's a lot of puts and takes associated with SG&A ratios and by the ability to invest and the fact that we have been investing quite heavily in various digital capabilities, things that are member facing and can actually improve the member experience. The other aspect is that, you know, we've really enjoyed a lot of fixed cost leveraging. You know, our premiums grew at 13.5% year over year, which obviously allowed the SG&A ratio to decline, you know, from that aspect as well.
So, you know, we do expect a reduction in our operating expense ratio in 2023, driven by the leverage of top-line growth, as well as improved operating efficiency, partially offset by the reinvestment and strategic initiatives in support of our growth. So, while certainly the mix of business does matter, and as we said in the guidance, Carelon services carries a higher SG&A ratio than the rest of the company in general, and we expect Carelon services to grow faster, a lot of puts and takes, but fixed cost leveraging and investment in capabilities are probably two of the most significant drivers year over year. Thank you.
Gail Boudreaux -- President and Chief Executive Officer
Next question, please.
Operator
Next, we'll go to the line of Steven Valiquette from Barclays. Please go ahead.
Steve Valiquette -- Barclays -- Analyst
Yeah. Great. Thanks. Good morning.
Appreciate the color on the '23 membership guidance, particularly in you commercial segment with the repricing strategy. You may have touched on this a little bit, but I guess, you previously talked about your goal of narrowing the profitability gap between the fee-based and risk-based commercial customers. So, I'm just curious if you can just provide a little more color on your expected progress on that profit gap in calendar 2023, in particular, just in light of all the pricing and growth trends you talked about for the risk- and fee-based books of business in commercial.
Gail Boudreaux -- President and Chief Executive Officer
Great. I'll have Morgan share his thoughts.
Morgan Kendrick -- President, Commercial Business
Steven, thank you for the question. And, you know, we had a very successful selling season with CarelonRx, as Pete indicated. And we grew our specialty lines of business rather materially. And, you know, we continue to make steady progress toward our goal of improving that revenue gap between risk- and fee-based business.
One thing of note, when you think about in 2022, retrospectively, looking back, which will take -- carry us forward as well, admin fee revenue grew nearly 8% compared with 4% in our fee-based membership growth. So, this alone is certainly clearly indicating that we've got an expansion in revenue and product per sold member. I would say, you know, this is driven by not only our Carelon assets, but it's also driven by strong growth in our clinical buy-ups, again, noted specialty products and our aligned incentives in Carelon services products. You know, and again -- so we feel good about that trajectory.
We feel good about that gap continuing to close. And as John had indicated earlier, this isn't about any one segment. This is around actually growing that fee-based business. Much of that business is moving to the fee-based schedules, but also the pull-through of the Carelon asset that we're working jointly with Pete and his team on.
Thank you for the question.
Gail Boudreaux -- President and Chief Executive Officer
Yeah. Thanks for the question. I think, as Morgan just shared, we're making really nice progress on really improving both the revenue per member and the profitability per member in our fee-based business. And, you know, the example he gave, I think, helps demonstrate that.
And so, overall, we feel it's been strong, and we have a lot of confidence in that. So, thanks again for the question. And it's, again, part of optimizing our health benefits business that we've talked about. Next question, please.
Operator
Next, we'll go to the line of George Hill from Deutsche Bank. Please go ahead.
George Hill -- Deutsche Bank -- Analyst
Hey, good morning. And thanks for taking the question. I have kind of a question on the future state of the CarelonRx business because you guys announced the BioPlus acquisition, you've got the Synergie Initiative, you've got the JV with SS&C on DomaniRx. So, I guess it's probably a question for '24 or beyond.
But I guess, can you talk about how much of the vertical integration of the PBM business that you think that you need to do, given the outsourced relationship with CVS and the other initiatives that you have going on? Thank you.
Peter Haytaian -- President, Diversified Business and IngenioRx
Yeah, George. Thanks a lot for that question. And I think it's helpful to sort of step back and think about our overall strategy and where we started in this regard. You know, when we started a few years ago, we always talked about being a different kind of PBM.
And our strategy has been keenly focused on whole health and integration of medical, pharmacy, behavioral, and social. And that's been core to what we've been doing. And we've also said, and we've been very deliberate about this, that we want to own the strategic levers that matter, those that, quite frankly, drive the greatest affordability choice, and, of course, superior patient experience. And that's the journey we're going on.
I think what you're seeing in BioPlus and what you're seeing in Synergie are really good examples of that and what we prioritize. If you look at specialty pharmacy, it's 40% to 50% of the overall growth spend right now. And it's a critical driver of value for patients. And so, that's where we started.
And we'll continue on this journey, again, through the lens of greater affordability and superior patient experience. So, over time, you will continue to see us take ownership of the strategic levers that really matter.
Gail Boudreaux -- President and Chief Executive Officer
Thank you. Next question.
Operator
Next, we'll go to the line of Gary Taylor from Cowen. Please go ahead.
Gary Taylor -- Cowen and Company -- Analyst
Hi. Good morning. Actually, I had a quick question about BioPlus as well. I was just wondering a couple of things.
If you could give us a sense of annual revenue there, geographic reach. And someone, I think Pete earlier, said, in the future would bring specialty fulfillment in-house. And I thought that's what BioPlus was. So, I just want to make sure I understand the business model there.
Peter Haytaian -- President, Diversified Business and IngenioRx
Yeah. Thanks for the question, Gary. We feel really good about adding BioPlus to the family. It hasn't obviously closed yet.
We think it will likely close in the first quarter. And in terms of their breadth, I won't get into all the specifics about it, but they are the largest independent specialty pharmacy out there that remains with a broad range of services. They cover over 100 of the limited distribution drugs, so we feel really good about that. And their footprint is covering all 50 states.
So, we believe it's a really great platform. The other thing I would say that we're really impressed by two things, quite frankly. One is really great talent over there with a lot of experience, long-standing experience. And then, the other real differentiating factor around BioPlus is their differentiated service model.
Time-to-therapy, the speed to which they're providing services, is really differentiating, and we'd like to build upon that. So, we're excited about this. And when it closes, we're obviously going to be very focused on building the scale to be able to take on all our specialty pharmacy.
Gail Boudreaux -- President and Chief Executive Officer
Thank you. We have one last question.
Operator
And for our final question, we'll go to the line of Michael Hall from Morgan Stanley. Please go ahead.
Michael Hall -- Morgan Stanley -- Analyst
Hey, thank you for the questions. Just wanted to dig a little deeper on commercial margins. I know you mentioned you're still targeting 10.5% to 11.5% by '25. I think John might have mentioned 125 bps better commercial margin in 2023.
Was that right? And if so, that would be slightly more than 8% for '23, which means there's still a considerable gap to your '25 target. And I was expecting a majority of that improvement might happen this year, just given your repricing experts. But, you know, if you're seeing 125 bps in '23, and the following two years would need at least 225 bps of improvement. So, I was wondering if you could just talk a little bit more about the path and progression of that improvement in '24 and '25.
If you could help us break down the drivers we can better envision that path, like, what percent of that improvement is coming from upselling your fee-based business or the shift to higher-margin small group, or just any other contributors, maybe potentially more of a pricing efforts beyond '23? Yeah, thank you.
John Gallina -- Executive Vice President and Chief Financial Officer
Yeah. Thank you for the question, Michael. I'm not sure where your 125 basis point comment came from, but that was not part of our prepared remarks. What I can share is that if you look at the press release and you can see on a reported basis, the third quarter of '22 versus the third quarter of '21, commercial margins increased by 120 basis points.
And then, in the fourth quarter of '22 versus fourth quarter of '21, on that reported basis, the commercial margins increased by 180 basis points. You know, in terms of the margin improvement, as we have said historically, it is not going to be pro rata. You know, we've got three more years, '23 to '25 to get to those target margins, that it will -- there will be far more of the improvement here in '23 for the reason that you noted. And then, there will be continued improvement in '24 and '25.
And obviously, we're going to continue to optimize our fully insured block together with the fee-based selling strategies that Morgan talked about. Overall, you know, we're still standing behind that margin target through 2025. Thank you.
Gail Boudreaux -- President and Chief Executive Officer
Thank you, John. And thank you for everyone for joining us. In closing, we're pleased to have delivered another strong year in 2022 and are confident that the ongoing execution of our strategy positions us well for 2023. We look forward to discussing our long-term strategy in greater detail at our 2023 investor conference, which we said we plan to host in New York City on March 23, 2023.
Thank you for your interest in Elevance Health, and have a great rest of week. Thank you.
Operator
[Operator signoff]
Duration: 0 minutes
Call participants:
Steve Tanal -- Vice President, Investor Relations
Gail Boudreaux -- President and Chief Executive Officer
John Gallina -- Executive Vice President and Chief Financial Officer
Lance Wilkes -- AllianceBernstein -- Analyst
Peter Haytaian -- President, Diversified Business and IngenioRx
A.J. Rice -- Credit Suisse -- Analyst
Justin Lake -- Wolfe Research -- Analyst
Nathan Rich -- Goldman Sachs -- Analyst
Scott Fidel -- Stephens, Inc. -- Analyst
Felicia Norwood -- President, Government Business Division
Lisa Gill -- JPMorgan Chase and Company -- Analyst
Kevin Fischbeck -- Bank of America Merrill Lynch -- Analyst
Stephen Baxter -- Wells Fargo Securities -- Analyst
Josh Raskin -- Nephron Research -- Analyst
Rob Cottrell -- Cleveland Research Company -- Analyst
Whit Mayo -- SVB Securities -- Analyst
Morgan Kendrick -- President, Commercial Business
Dave Windley -- Jefferies -- Analyst
Steve Valiquette -- Barclays -- Analyst
George Hill -- Deutsche Bank -- Analyst
Gary Taylor -- Cowen and Company -- Analyst
Michael Hall -- Morgan Stanley -- Analyst