Image source: The Motley Fool.
Reata Pharmaceuticals, Inc. (RETA)
Q4 2020 Earnings Call
Mar 1, 2021, 8:30 a.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Ladies and gentlemen, thank you for standing by and welcome to the Reata Pharmaceuticals Fourth Quarter Financial and Full Year 2020 Financial Results and Update on Development Programs Conference Call. An audio recording of today's webcast will be available shortly after the call today on Reata's website at reatapharma.com in the Investors section.
Before the company proceeds with its remarks, please note that forward-looking statements disclosed in the company's press release. The company will be making forward-looking statements on today's call and there are many factors that could cause results to differ from expectations including those noted in the company's SEC filings. Today's statements are no guarantees of future outcomes. Please also note that any comments made on today's call apply only as of today March 1, 2021 and may no longer be accurate at the time of any webcast replay or transcript reading. Following the prepared remarks, we will open the call up for questions. At that time we will ask that you please limit yourself to one question and one follow-up, so that we can accommodate as many questions as possible.
We are joined today by the company's Chief Executive Officer, Warren Huff; Chief Research and Development Officer Colin Meyer; Chief Operating Officer and Chief Financial Officer, Manmeet Soni. At this time I would like to turn the conference call over to Warren Huff, Chief Executive Officer of Reata.
10 stocks we like better than Reata Pharmaceuticals, Inc.
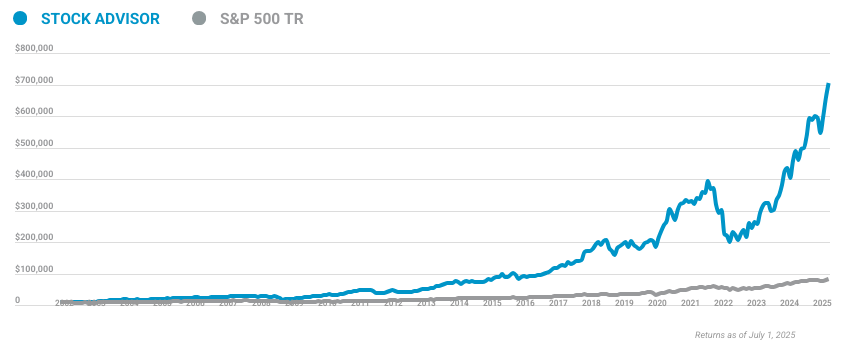
When investing geniuses David and Tom Gardner have a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
David and Tom just revealed what they believe are the ten best stocks for investors to buy right now... and Reata Pharmaceuticals, Inc. wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of February 24, 2021
Warren Huff -- Founding Chief Executive Officer and President
Thank you. Good morning everyone and thank you for joining us today. We have a full agenda of information to share and I will begin with our most recent updates starting on Slide 4. I am pleased to report that Reata has submitted its new drug application for bardoxolone and Alport syndrome. The completion of our NDA follows from the positive Phase 3 year two data we reported just three and half months ago. This marks a major milestone for our company. It's the first NDA Reata has submitted in its history, more importantly this NDA marks a major milestone for Alport syndrome patients who have a devastating disease for which there is no approved therapy. On behalf of everyone at Reata, I extend my deepest thanks to the patients who participated in our clinical trials and also their families. As a serious genetic condition, Alport syndrome can have far reaching effects on the families who face it. For them most of all, we're committed to seeing the regulatory process through to completion.
As you'll see from our Reata at a Glance slide, we have a number of updates to share today beyond the submitted NDA. Among other topics we will highlight the progress of the FALCON study of bardoxolone in Autosomal Dominant Polycystic Kidney Disease. I'm very pleased with the momentum we see in FALCON enrollment across sites worldwide. Colin will walk through those details, who will also discuss the MERLIN trial of bardoxolone in rapidly progressing forms of CKD. Continuing with recent updates, I want to acknowledge the patient petition that we received from the Friedrich's Ataxia community a few weeks ago. More than 74,000 Friedrich's Ataxia patients, their families, physicians, researchers, and others came together to express their desire for a regulatory path forward for Omav.
As you know, we issued a response to the petition in which we emphasized our hope to be able to advance Omav further through the regulatory process pending direction from the FDA. We've requested a Type C meeting to carry the discussion forward. At that meeting, we plan to present additional 72-week data that we believe supports Omav's potential as a disease modifying therapy in Friedreich's Ataxia. Colin will offer a top line overview of these data as part of his comments on this call. He'll also offer insights into work under way to develop additional assets in our expanding neurology portfolio.
I want to emphasize the strength of our company's position as we move further into 2021. The onset of the COVID-19 pandemic in 2020 imposed significant challenges for Reata at a crucial interval. Our company's mission to develop therapies that can change patient's lives for the better will continue to fuel us on the road ahead. Colin will now discuss updates to our development pipelines.
Colin Meyer -- Chief Research & Development Officer and Executive Vice President
Thanks, Warren. I'll provide a top line review of progress in our development programs last year, followed by a review of updates for a FALCON trial in ADPKD or MERLIN trial in CKD patients at risk of rapid progression, the regulatory status of Omav and FA and an update on RTA 901. As we've discussed previously, Alport syndrome is the second most common hereditary form of CKD, which is caused by mutations in collagen that promote inflammation, fibrosis, and loss of kidney function. The misdiagnosis rate has been reported to be as high as 62% and due to the rapid loss of kidney function, patients have a high likelihood of kidney failure. In the most severe forms of the disease, patients have a 100% lifetime risk of kidney failure with a median age of kidney failure of 25 years.
As shown in the next slide, our NDA contains data from three separate Alport's syndrome trials that contain just under 200 unique patients, including the Phase 2 and Phase 3 CARDINAL studies, as well as the ongoing EAGLE open label extension study that is continuing to accumulate data. The EAGLE Extension study allows patients to complete CARDINAL to receive open label bardoxolone until the drug is commercially available. At this time, we have enrolled 100 patients in the EAGLE Extension study.
Next slide. Unlike most rare disease development programs that contain a relatively small datasets based on the extensive development history, our NDA contains data from multiple clinical trials and disease states that have enrolled over 3,000 patients which support our Alport syndrome NDA. We have shown improvements in kidney function as measured by estimated GFR or eGFR, measured GFR, and creatinine clearance, demonstrating that the changes in eGFR represent is assessed by some. creatinine represents a true change in kidney function. We have shown reductions in inflammatory biomarkers supporting bardoxolone's anti-inflammatory mechanism of action, we have observed sustained improvements in eGFR for up to three years in Alport syndrome patients. Prior to our Alport's syndrome trials, we have shown sustained improvements in eGFR for a year and significant improvements in off-treating eGFR in two prior trials. In the CARDINAL Phase 3 and a prior diabetic CKD trial, we observed a reduction in the risk of kidney failure outcomes.
Next slide. Chronic inflammation is integral to progressive decline of kidney function associated with numerous forms of chronic kidney disease or CKD, including Alport syndrome. Co-inflammatory stimuli such as Angiotensin 2 increase the production of ROS, resulting in glomerular endothelial function, pathogenic mesangial cell contraction, and impaired [Indecipherable] function. These effects reduce the glomerular surface area for filtration or Kf [Phonetic], which in turn reduces single nephron GFR. In addition, chronic inflammation drives kidney remodeling by activating NF-kB and TGF-Beta and other pro-fibrotic mediators. Over time, these chronic processes result in the complete loss of function of individual nephrons. Nrf2 is a transcription factor with anti-inflammatory and tissue per test effects that is suppressed in many forms of CKD. Genome wide analysis from kidney biopsies across nine different forms of CKD validate the association between impaired intellectual activity and reduced kidney function across multiple forms of CKD, including Alport syndrome.
Next slide. We have conducted a large number of non-clinical studies to elucidate the mechanism of action of bardoxolone, which is novel. Our academic collaborators and we have conducted sophisticated imaging experiments in living animals to demonstrate that bardoxolone acutely increases single nephron GFR by restoring the filtration surface area in the kidney, reversing inflammation within constriction. We have shown that this effect is not associated with any changes in the afferent for efferent tone, demonstrating that this effect is not associated with increases in inter-glomerular pressure or hyperfiltration. Lastly, we have demonstrated that bardoxolone methyl has anti fibrotic effects and improves kidney structure and function in response to pressure overload and multiple classical animal models of CKD caused by hyperfiltration, hypertension, high protein, diabetes, and dyslipidemia.
Next slide. Turning to supporters, Alport syndrome's specific clinical data, they're contained in the NDA recall that the CARDINAL Phase 3 study was a randomized, double blind, placebo controlled two-year trial. The trial enrolled a broad range of patients with eGFR from 30 to 90 ml per minute in age from 12 to 70 years. The primary endpoints were the on-treatment changes in eGFR at least 48 and 100 [Phonetic] and the key secondary endpoints where the off treatment eGFR changes that leaves 52 and 104. We believe the on treatment changes in eGFR represent the full clinical benefit of bardoxolone and the off treatment changes were included to determine if bardoxolone's eGFR profile is consistent with disease modification and to rule out harm.
As shown on the next slide and previously discussed CARDINAL met its primary endpoints demonstrating large, clinically meaningful improvements in on treatment eGFR with significant P values. It is important to recognize the distinction between the ITT and the mITT populations. The ITT analysis includes all available eGFR values from all patients, even if they discontinued drugs. This is a very conservative analysis since it is diluted by patients who discontinue drugs and are no longer benefiting from the drug. To understand the treatment effect of bardoxolone while patients are actually receiving drug, we prospectively defined the mITT population, which excludes eGFR values once patients discontinue bardoxolone. In clinical practice, when patients are receiving bardoxolone, the mITT eGFR improvement is likely most representative of the actual clinical benefit. As we discussed during our last call, the mITT eGFR changeover time in the second year separated for the bardoxolone patients compared to the placebo patients.
As you can see on the next slide, all pre-specified subgroups favored bardoxolone. We observed a treatment effect in pediatric patients, adults, males, females, patients with high and low proteinuria across the eGFR range studied in all major genetic subtypes and on top of standard of care ACE inhibitors and ARBs. As shown on the following slide and previously discussed, CARDINAL also met its key secondary off-treatment endpoints. The persisting significant increase in eGFR following wash-out observed twice in CARDINAL provided evidence that the on-treatment eGFR improvement is consistent with a beneficial and not harmful profile. While we believe the on treatment effect represents the clinical benefits, the off treatment improvements demonstrate disease modification. This off treatment endpoint was previously used to support the approval of tolvaptan for ADPKD.
Next slide. Due to the relatively small size of the CARDINAL trial, which was conducted in a rare disease population, it was not powered to show a difference in the off treatment eGFR from year one to year two. Additionally, the patients included in each analysis are slightly different due to drop outs. So these independent endpoints aren't directly comparable. To understand the relationship between the off treatment change after year one and two, we performed a longitudinal off treatment eGFR slope analysis. This effectively uses paired values from patients to generate individual slopes. These are then used to estimate the population for each treatment group. As you can see in the figure, the dotted lines represent the off-treatment slopes and shows a 50% slower slope for bardoxolone. This suggests that bardoxolone is slowing disease progression by 50%.
As I mentioned earlier, bardoxolone has a novel mechanism of action and sustained increases in eGFR have not been observed in CKD studies with any other intervention. The one intervention that has been shown to increase eGFR and amlodipine does so by increasing pressure causing hyperfiltration. In the African-American study of kidney disease, also known as ASK, the initial eGFR increase was small and transient. The increase in eGFR was only 4 ml per minute and peaked at six months of treatment. After this time, eGFR declined quickly and more rapidly than was observed in the other treatment groups. We performed a quartile analysis why eGFR changed at week 12 in CARDINAL to determine what happens to the patients who have the largest acute changes in eGFR after two years of treatment. As you can see in the table, the quartile with the largest eGFR change had a very large increase in eGFR of 27 ml per minutes at week 12. And after two years of treatment, these patients had the largest on and off treatment changes at least 100 and 104 relative to all other bardoxolone placebo quartiles. Conversely, the bardoxolone patients who had the smallest acute changes at week 12 had the smallest improvements at the end of two years. These data are very important since they demonstrate that acute increases in eGFR are not associated with accelerated progression of kidney disease long-term and are opposite the pattern of hyper filtration.
Turning to Slide 19. As we've discussed previously, the largest improvements in eGFR across all pre-specified subgroups were observed in the pediatric patients. These patients have the most severe mutations and progress at the fastest rate. The improvements in eGFR at least 100 and 104 for large clinically meaningful and even statistically significant within the subgroup. Notably, the most forms of CKD, two years of treatment may represent only 10% or less of patients remaining dialysis through time, since it often takes decades for patients to progress to kidney failure. However, in these patients with very rapid progression, the two-year duration of treatment represents approximately 30% in these patients remaining dialysis three times.
Next Slide. We've previously shown the proteinuria data measured as a urine albumin to creatinine ratio or UACR across all patients. Initial increases were observed in the bardoxolone group that were mathematically accounted for by the change in eGFR, which would be expected to increase UACR. Importantly, UACR did not worsen over time and the value has returned to placebo levels during the two-hour treatment periods. In the overall population, which was primarily adults, there was only a slight worsening in UACR in the placebo patients despite the large losses of eGFR. The pediatric UACR data are shown on this slide and demonstrate a meaningful worsening of UACR in the placebo patients over the two-year duration of the trial. These patients had a doubling of UACR, whereas the bardoxolone treated pediatric patients had no change from baseline. By week 104, UACR levels in the bardoxolone treated pediatric patients were reduced when compared to the placebo pediatric patients. We believe the pediatric data highlight the overall data set and provide evidence that bardoxolone has a clinically meaningful and disease modifying profile.
Moving on to other topics, on Slide 21, those unfamiliar with bardoxolone's profile sometimes ask if it is consistent with hyperfiltration. As shown on this slide in our extensively studied in nonclinical and clinical studies the profile is opposite of hyperfiltration. Hyperfiltration is caused by increases in pressure within the kidney that cause damage, including increased permeability to albumin and worsening of fibrosis. We have shown that bardoxolone acutely increases GFR like increasing glomerular surface area without affecting the intraglomerular pressure or permeability to albumin. In the gold standard model of hyperfiltration, the 5-6 nephrectomy, we observed preservation of kidney function and reduced fibrosis. As mentioned a few minutes ago, the clinical eGFR profile of hyperfiltration clinically is associated with transient, small increases in eGFR, followed by accelerated decline of eGFR after six months of treatment. Off-treatment eGFR changes are worse than placebo and hyperfiltration increases kidney failure composite events. Bardoxolone's eGFR profile is associated with large sustained increases in eGFR for at least three years, persistent improvements in off treatment eGFR and a reduction of kidney failure composite events. The UACR profile hyperfiltration is associated with initial increases in UACR that are out of proportion to changes in eGFR and continue over time. Off treatment values are higher than placebo due to loss of glomerular integrity. Bardoxolone's profile demonstrates initial increase that is accounted for by increases in eGFR, plateaus after the initial increase, and returns to baseline within four weeks of stopping drugs. Therefore, the profile of bardoxolone is novel and differentiated from hyperfiltration. We believe we have fully addressed this issue and there is no evidence that supports that bardoxolone's mechanism of action is due to hyperfiltration.
Next slide. Clinically, we have observed increases in ALT and AST, which is associated with reductions in total bilirubin or improvement in liver function. While ALT and AST are used clinically as biomarkers of liver toxicity as seen on the left part of the slide, they are expressed in numerous tissues other than the liver, including fat tissue, the kidney, muscle, the brain, lungs, and others. They have an important role in energy metabolism, including biosynthesis, which are fundamental processes associated with Nrf2 activation. Genetic suppression of Nrf2 is associated with lower tissue expression and serum activated ALT, whereas genetic activation of Nrf2 generally increases ALT production and activity. We have shown in cells from multiple tissues, including the liver, muscle, colon, macrophages and kidney that bardoxolone increases production of ALT and AST, demonstrating that these increases are due to pharmacological increases in production and not injury.
Next slide. The clinical profile of ALT, AST, and bilirubin is consistent with data we have published from our prior trials in diabetic CKD. ALT and ASD levels peaked approximately two weeks after patients reached their goal dose. Levels then trend down to a new steady state, likely as a new equilibrium is reached. And during the off treatment periods, the levels return to baseline and placebo levels. Across our entire development program, in clinical trials conducted to date, we have not observed any cases of highest law, which is associated with large increases in total bilirubin and impaired liver function. Instead, we have observed reductions in total bilirubin or improvements in liver function. In CARDINAL we conservatively implemented stopping criteria in accordance with FDA guidance. A total of six patients met these criteria. Notably, none of these patients had any evidence of liver injury. We have relaxed these criteria in our ongoing FALCON trial to further reduce these discontinuations. The draft proposed Alport Syndrome label provides guidance for monitoring and management that we believe will minimize discontinuations due to these increases.
Next slide. Regarding changes in body weight, we had previously shown a non-clinical model that this effect is due to metabolic reprogramming, resulting in utilization of sward fuels in the form of fat, increased energy production, and reduced weight due to fat loss. We have shown in four prior trials, that changes in eGFR are not due to changes in creatinine production or excretion, demonstrating that weight loss is not due to muscle loss. We have also shown that weight loss is dependent on baseline BMI. In the CARDINAL trial, there was no correlation between weight and eGFR change. Further in the pre-specified subgroups of BMI lower than or higher than 30, the eGFR change was almost identical, despite the large difference in weight loss of 1.9 kg versus 7.1 kg. In summary, eGFR increases with bardoxolone are not due to weight or muscle loss and reflect true increases in GFR.
Next slide. In conclusion, our Alport Syndrome program has been conducted in a rare, severe form of CKD with no approved therapies. Our Phase 3 CARDINAL trial hit its primary and key secondary endpoints, demonstrated disease modifying activity, and an acceptable safety profile is supported by a large safety database of over 3,000 patients. We are pleased to have submitted our first NDA and we believe that if approved, bardoxolone may be the first therapy to preserve kidney function with disease modifying effects in patients with Alport's Syndrome.
Next Slide. Turning to our ADPKD development program, ADPKD is a second -- I am sorry, it is the most common hereditary form of CKD with approximately 140,000 diagnosed patients in the US. Despite standard of care, including blood pressure control and one approved drug, patients still lose kidney function at a fast rate. Because of this, a high percentage of patients ultimately progress to kidney failure. Our Phase 3 FALCON trial is currently enrolling patients. Enrollment was passed last year due to COVID and we've been able to resume enrollment at most sites. Currently over 220 patients have been enrolled and we are planning to increase the sample size of FALCON to 550 patients from 300, primarily to account for the increased variability in the second year of the CARDINAL trial so that we can maintain the same statistical powering assumptions. We are not changing the estimated treatment effect to drop out estimates or any other parameters, and this change will make the trial similar in size to other ADPKD trials. Similar to the CARDINAL trial, the trial was two years in total duration and the key endpoints are at the end of the first and second year of treatment. Even with the sample size increase, we expect enrollment to be complete by the end of 2021.
Turning to Slide 30. We recently initiated MERLIN, a double blind, placebo controlled Phase 2 trial evaluating the safety and efficacy of bardoxolone in patients at risk of rapidly progressing CKD due to multiple etiologies, including common and rare forms of CKD such as diabetic CKD, hypertensive CKD, IJ nephropathy, FSGS and others. We plan to enroll approximately 70 patients aged 18 to 70, with eGFR between 20 to 60 ml per minutes and one of several risk factors for progression. The primary endpoint of MERLIN is a change in eGFR from baseline to week 12. Enrollment began in February, last month and they are expected in the second half of this year. If results of this study are positive our plan would be to potentially proceed to a larger Phase 3 trial in this population of patients at high risk for progression to kidney failure.
Now, let's move to our program in Friedreich's Ataxia. FA is a rare disease characterized by progressive loss of motor function with a median survival of 35 years. There are an estimated 5,000 patients in the US out of 4,000 diagnosed and these patients have no approved therapies. On our last call, I stated that we submitted a baseline controlled study to FDA in response to their request for additional analysis to increase the persuasiveness of MOXIe Part 2 data. After their internal review, they stated that these analyses did not strengthen the results and they recommended an initial analysis. We have named these analyses the delayed start analysis that compares patients initially randomized to placebo and Omav to each other in the extension. We believe this analysis is intended to determine if Omav's profile is consistent with disease modification. FDA stated that the potential for these analyses to sufficiently strengthen the study results was questionable due to the small number of patients available for analysis.
Next Slide. The results of the delayed start analysis are shown on the next slide. We compared the rate of change in mFARS and the extension for the patients initially randomized to Omav versus those originally randomized to placebo. We conduct the analysis using two populations. First, we used all available data in the extension to compute annualized rates of mFARS change and 73 out of 82 or 89% of patients who enrolled in MOXIe Part 2 contribute to this analysis. Notably, this is higher than the 14 Part 2 patients who contribute to the baseline control study. Second, we analyzed patients who completed one and a half years of the extension, which includes a total of 20 patients. 11 of these patients have received Omav for a total of two and a half years. As can be seen in this figure on the left, which includes data from all extension patients, once patients enter the extension those initially randomized to Omav progressed at a very slow rate of approximately 0.5 mFARS points per year.
After another 1.5 years of follow up, patients initially randomized to placebo, progressed about 1.5 points from their initial baseline MOXIe Part 2 to baseline extension also progressed at a rate of approximately 0.5 inverse points per year in extension which is slower than the prior rate of progression. In the extension the slopes are generally parallel and there's no significant difference between them. Most important, patients initially randomized to placebo did not catch up with the patients who initially randomized to Omav. If Omav only provided symptomatic treatment, they would be able to achieve the same treatment response relative to the initial baseline. However, patients who initially received Omav have been able to maintain better absolute impulse scores, demonstrating that the first year of treatment in MOXIe Part 2 provided a treatment benefit. This is the hallmark of disease modifying activity.
The analysis on the right, which includes all patients who have completed one and a half years in extension, shows similar findings. The data at each time point contains the same patients, with the exception of week 100, which has some missing values due to site closures related to COVID-19. In this completer subset, the 11 patients who have received two and a half years of treatment have on average not progressed. The patients, initially randomized to placebo to progress while receiving placebo, have also on average not progressed during the one and a half years on Omav during the extension, consistent with the analysis that includes all patients. The patients originally randomized to placebo did not catch up with those initially randomized to Omav, which demonstrates the disease modifying profile.
Next slide. From a regulatory perspective, we have requested a Type C meeting with FDA to discuss the delayed start analysis and the development program. Pending discussions with FDA and EMA we plan to initiate a second pivotal trial of Omav in the second half of 2021 to support approval. Turning to Slide 37, we believe the MOXIe results provide proof of concept for the use of Omav in other neurological diseases that have a common pathophysiology of mitochondrial dysfunction and neural inflammation. Omav and analogues have shown activity in numerous nonclinical models as well as patient biopsy samples and we believe the pharmacology is applicable to a broad set of neurological diseases, including other movement disorders such as PSP, Parkinson's disease, and Huntington's disease, as well as other diseases that affect neuromuscular function and memory.
Now on Slide 39, our earlier stage pipeline includes RTA 901, which is wholly owned by Reata. RTA 901 is a highly potent and selective oral, small molecule C-terminal modulator of Hsp90. Hsp90 is a molecular chaperone that facilitates the folding instability of many proteins critical for cellular viability. Hsp90 also regulates the expression of Hsp70, another molecular chaperone that promotes cell survival in response to stress and affects mitochondrial function. N-terminal Hsp90 inhibitors previously developed as anticancer agents increase Hsp70 expression, but also inhibit client protein folding, which results in cytotoxicity. In contrast, RTA 901 increases transcription of Hsp70 without inhibiting client protein folding, resulting in robust cytoprotection in the absence of cellular toxicity. This biology is distinct from our [Indecipherable] activator program but has many parallels.
Next Slide, RTA 901 has demonstrated activity in multiple models of diabetic neuropathy. It has been shown to reduce pain acutely in models of painful diabetic neuropathy. Most notably, RTA 901 treatment results in recovery of lost sensation in models of insensate diabetic neuropathy, which is a novel and differentiated profile from other agents that have targeted diabetic neuropathy.
Next slide. Of the approximately 4 million US patients with moderate or severe diabetic peripheral neuropathic pain, approximately half of those treated do not achieve an adequate pain reduction with available therapies. We have completed Phase 1 SAD and MAD studies in healthy volunteers that demonstrated an acceptable safety profile with no safety signals, drug discontinuations or SAE while achieving appropriate safety margins. In the second quarter of this year, we're planning to initiate two additional clinical pharmacology studies to support the launch of the phase two study in the fourth quarter of this year. This study will be a randomized placebo controlled dose ranging study using a standardized pain scale. I'll now turn the call over to Manmeet to provide a summary of our financials for the fourth quarter and full year 2020.
Manmeet S. Soni -- Chief Operating Officer & Chief Financial Officer and Executive Vice President
Thanks, Colin. And good morning, everyone. Please refer to our press release issued earlier today for a summary of our financial results for the fourth quarter and full year of 2020. I will start on Slide 43. With our cash balance, we maintained a solid balance sheet ending 2020 with approximately $818.2 million in cash and cash equivalents. This includes cash proceeds coming from our financing completed in December 2020 amounting to approximately $277.5 million in net proceeds. Our GAAP net loss for the fourth quarter of 2020 was $65.8 million, or $1.90 per share on both basic and diluted basis, as compared to a net loss of $186.9 million or $5.91 per share on both basic and diluted basis for the same period of the prior year.
Our GAAP net loss for the year ended December 31, 2020 was $247.8 million or $7.35 per share on both basic and diluted basis as compared to a net loss of $290.2 million or $9.54 per share on both basic and diluted basis for the prior year. The decrease in net loss was primarily due to reacquired license rights expense incurred in 2019 and is offset by an increase in operating expenses in 2020. In addition, our R&D expenses increased due to R&D activities and higher personnel and equity compensation expenses due to increase in headcount. Increases in our G&A expenses were driven by higher personnel and equity compensation expense due to increase in headcount to prepare for commercial launch and to support growth in our development activities. We have made all necessary investments to ensure the strong and successful commercial launch of bardoxolone later this year, pending FDA review and approval.
Moving to revenues, our collaboration revenues were $3.2 million during the fourth quarter of 2020 as compared to $2.7 million in the fourth quarter of 2019. The increase was related to reimbursement from KKC related to manufacturing and non-clinical study. Moving to non-GAAP measures on Slide 44, our non-GAAP R&D expenses were $32.7 million for the fourth quarter of 2020 as compared to $36.7 million for the same period of the year prior. Our non-GAAP G&A expenses were $12.3 million for the fourth quarter of 2020 as compared to $13.4 million for the same period of the year prior. To summarize, our non-GAAP operating expenses were $45.2 million during the fourth quarter of 2020 with multiple pivotal programs and substantial preclinical activities, reflective of the strength and potential of Reata's pipeline. In keeping with our current guidance, our year-end cash balance of $880 million is expected to fund our operations through mid-2024.
In terms of our commercial readiness with our submission of NDA, an anticipated PDUFA later this year, we have taken concerted steps to ensure launch readiness by Q4 of this year. We continue to ramp up our broad based disease education efforts, including our newly launched disease education website alportsyndrome.com designed for prescribers and patients. Our field directors of market access are on track for hiring in the second quarter. We continue to advance our peer engagement strategy with the goal of achieving broad and timely payer coverage of bardoxolone. Finally, we are in the final stages of building our logistics infrastructure with a patient hub, specialized pharmacy, and distributed network and third party logistics, all in that full launch readiness for bard in the US by fourth quarter of 2021 with a longer term aim of supporting multiple launches over the next several years.
With that, I will turn the call over to Warren who will take us through Slide 47.
Warren Huff -- Founding Chief Executive Officer and President
Thanks Manmeet. As our presentation today indicates, we're making significant progress across our broadening set of programs, including our late stage and earlier pipeline programs. We've now fulfilled a major regulatory milestone for bardoxolone and Alport Syndrome. We remain dedicated to advancing Omav in Friedrich's Ataxia. We look forward to the year ahead and maximizing the opportunities that it presents to our company. That concludes our prepared remarks and I'd like to thank everyone who dialed in. I'll now turn the call over to the operator for questions.
Questions and Answers:
Operator
[Operator Instructions]
Our first question today comes from Yigal Nochomovitz from Citigroup. Please go ahead with your question.
Yigal Nochomovitz -- Citigroup -- Analyst
Hi, great, thanks for taking my questions. I have one with respect to the second Friedrich's Ataxia Phase 3 trial. Could you comment on how that study may potentially differ from MOXIe Part 2 and will the data and learnings from the delayed start analysis that you did for MOXIe Part 2 impact the design of the second FA Phase 3?
Warren Huff -- Founding Chief Executive Officer and President
Thanks Yigal. So you're asking about the potential design of a second pivotal study in Friedrich's Ataxia. Colin could you take that?
Colin Meyer -- Chief Research & Development Officer and Executive Vice President
Sure. And so I think, yes, the prior MOXIe Part 2 data plus the delayed start analysis, as well as our baseline controlled study will inform the next design. And so we need to have discussions with FDA to determine specifically what we would need to do to fulfill the obligations in order to get the approval. And so I think we'll provide more guidance after our Type C meeting.
Yigal Nochomovitz -- Citigroup -- Analyst
Okay, got it. Thanks. And then just one follow-up. With respect to the increased enrollment in FALCON, can you just comment on whether that was an internal decision or was that the result of any FDA feedback or possibly seeing any of the pools and blinded data that would suggest that the variability is greater than you previously anticipated?
Warren Huff -- Founding Chief Executive Officer and President
Yes, so you're asking about the whether the increase in the sample size was based on any FDA feedback or overall analysis of the variability. I'll actually I'll respond directly to that. It wasn't in response to FDA feedback, it was directly in response to what we observed in variability in the year two of the CARDINAL study, and which, may be related to the pandemic environment that we're in. And so we felt it was simply prudent to increase the sample size to preserve the statistical power if we observe a similar rate of variability.
Yigal Nochomovitz -- Citigroup -- Analyst
Got it, thanks Warren.
Operator
Our next question comes from Maury Raycroft from Jefferies. Please go ahead with your question.
Maury Raycroft -- Jefferies -- Analyst
Hi, good morning everyone, and congrats on the progress. Thanks for taking my questions. First one is going to be Friedrich's Ataxia too. Just wondering if we can get a better sense of if you could still file for approval after the Type C meeting and prior to running -- and prior to running the second study. I guess, can you run through possible scenarios for outcomes from the Type C meeting?
Warren Huff -- Founding Chief Executive Officer and President
Sure, I'll take that. Obviously, the position of an agency has been to date that we need to increase the persuasiveness statistically of the result or we need to provide additional data from the long-term extension or perform a second pivotal study. The purpose of the Type C meeting that we just requested, is to put that question directly to them and there are multiple outcomes. They could potentially see the additional analysis as supporting the conclusion that it's disease modifying. If they reach that conclusion, then there would be an ethical problem with conducting a second pivotal study, and then they might permit us to submit an NDA based on the existing clinical package. However, they may find that that data doesn't support a conclusion, that it's disease modifying, and require us to conduct a second pivotal study. And so it's just the -- it's up to the FDA.
Maury Raycroft -- Jefferies -- Analyst
Got it, OK. And just to clarify for the ongoing FALCON study, are you seeing anything with dose reductions, discontinuations, or anything else from the study that would also provide some reason to upsize that study?
Warren Huff -- Founding Chief Executive Officer and President
Colin, would you like to take that?
Colin Meyer -- Chief Research & Development Officer and Executive Vice President
Yes, Maury. So as I mentioned, during my prepared remarks, there's no data that would suggest that we need to change our assumptions, or dropouts, treatment factor or anything else. It's solely based upon the variability from the CARDINAL trial, and Alport Syndrome. As Warren said, we noted a higher variability or standard deviation of change in an estimated GFR in year two of CARDINAL and so we're not sure if that's going to happen in the FALCON trial. But we thought it'd be prudent to increase the sample size. There was no other data that suggested that our assumptions may be wrong. But since standard deviation is a critical input into the power calculations, we wanted to make sure that we accounted for a potential increase, if we were to observe it. And then from an enrollment perspective, we today disclosed for the first time the number of patients we've enrolled, and despite having to pause enrollment due to COVID, we have made substantial progress. We've enrolled over 220 patients and since most of our sites are able to screen and enroll patients, the incremental time to increase enrollment, enroll those additional patients is not that long. And so this makes the trial overall, we believe robust and similar in size to other PKD trials, and accounts for any potential increase in variability that we could assume.
Maury Raycroft -- Jefferies -- Analyst
Got it, pretty good. Thanks for taking my questions. I will hop back in the queue.
Operator
Our next question comes from Annabel Samimy from Stifel. Please go ahead with your question.
Annabel Samimy -- Stifel -- Analyst
Hi, thanks for taking my question. I have a couple So can you talk about what specifically you're doing to address the discontinuation from the ASP and ALT in the ADPKD trial, it seems to be a big question among physicians to control the discontinuation? And then follow on Omav, what is it specifically, do you know that the FDA would be looking at to determine whether it is disease modifying, did that change -- that difference between the slopes need to be statistically significant or is it enough that they're parallel? Thank you.
Warren Huff -- Founding Chief Executive Officer and President
I'll take the second question first Colin and then would you comment on FALCON. We believe that the analysis that they suggested is based on guidance that they've given for these type of analyses in the Alzheimer's setting. And basically, what you're looking for is to see that the patients that crossed over to the long term extension study from active basically maintained a benefit over time, versus the patients that crossed over to the long-term extension from placebo. So you actually want those slopes to be parallel, and there to not be statistical significance between them. And that's -- we believe that that's what the data shows. A key question will just be is the patient -- are the patient numbers high enough and is the competence around that data strong enough to convince them that that is evidence of a disease modifying effect. We think it is but again, the decision is the decision of the FDA.
Annabel Samimy -- Stifel -- Analyst
Great, and then on the ALT, ASP changes?
Colin Meyer -- Chief Research & Development Officer and Executive Vice President
Yes, so as I disclosed a few minutes ago, we had six patients who met criteria in standard FDA guidance that I believe, probably almost all companies follow during clinical trials. And if patients have an elevation of a certain magnitude and meet certain criteria, we had been requiring patients to permanently discontinue study bard. So they could not restart, but based upon our extensive safety database and in consultation with a herpetologist and as we've now published, we believe that these changes are pharmacological changes consistent with activation of Nrf2 and things are very distinct from a profile of liver injury. And so in the FALCON protocol, we did not require permanent discontinuations. And so with patients, you'll hit a certain threshold that would have required permanent discontinuation, we simply give the patients a drug holiday and they come back to the clinic and start at a lower dose. So it's a very straightforward way to manage these elevations.
Annabel Samimy -- Stifel -- Analyst
Okay, great, thank you.
Operator
Our next question comes from Brian Skorney from Baird. Please go ahead with your question.
Brian Skorney -- Baird -- Analyst
Hey, good morning everyone. Thanks for taking the question. And thanks for all the granularity in the presentation. My question is really on sort of the differences across the different populations and how we could kind of think about the results from FALCON with the increase in enrollment size. We've seen in BEACON and we've seen in CARDINAL at least some sort of numerical benefits in terms of progression to end stage renal disease, your partner Kirin is powered at about a little more than twice the size of FALCON in diabetic kidney disease. So I'm just wondering if we kind of think about the ADPKD patient population, what the rate of progression to ESRD is in this patient population relative to diabetic kidney disease and Alport and at this scale, if we sort of saw a reduction in progression to ESRD on par with the numerical reduction we saw in CARDINAL, would this be a statistically valuable secondary endpoint?
Warren Huff -- Founding Chief Executive Officer and President
Colin, do you want to take that?
Colin Meyer -- Chief Research & Development Officer and Executive Vice President
Yes, so I think we predefined it in CARDINAL because we thought it'd be helpful to characterize the composite is now used in trials like our Japanese partners on the trial. And so we don't -- we're not changing the size so that can be power for that endpoint. But it would potentially increase our chances of showing statistical separation in CARDINAL with 157 patients, the p value was 0.086, I believe and the hazard ratio was about 0.5. And so in ADPKD patients progressed at a slower rate and there's not as many of the patients who have extremely large losses, for instance, the patient in CARDINAL had the largest losses, the placebo patient had lost about 50 ml per minute, over two years. And so we don't expect patients to have that extreme blood losses. But, potentially, if things go the right way, that could be a very valuable input for us.
Brian Skorney -- Baird -- Analyst
Okay.
Operator
Our next question comes from Charles Duncan from Cantor Fitzgerald. Please go ahead with your question.
Charles Duncan -- Cantor Fitzgerald -- Analyst
Hey, thanks for taking my questions. Congrats, Warren and team on the bardoxolone filing and Alport. I had a question on Omav and I apologize if I missed this. I'm juggling multiple calls this morning. But in terms of the Type C meeting, can you give us a little bit more color on that timing and would you wait for the meeting minutes to be able to disclose what you plan to do and I saw in your press release that you plan to start a second study in the second half, when do you think you could operationalize that, just a little bit more color on the playing forward with Omav?
Warren Huff -- Founding Chief Executive Officer and President
Sure. We can't comment on the timing in fact we don't normally comment on the exact timing of the meetings but we have submitted the meeting request. And then what we say publicly after the meeting really depends on and how could we do that depends on what we hear. If something is obviously very material, then we generally release it even before we get the minutes. But normally we were prudent dictates that you wait to get their minutes before you comment.
Charles Duncan -- Cantor Fitzgerald -- Analyst
That makes sense to me. And then in terms of the study timing, when can you operationalize that?
Warren Huff -- Founding Chief Executive Officer and President
We believe that we could have it operationalize by Q4. But it could potentially be earlier, depending upon what happens in the interactions with the FDA.
Charles Duncan -- Cantor Fitzgerald -- Analyst
Yes. And then regarding the agency, I mean, I appreciate what you mentioned in terms of the Alzheimer's space and the kind of the setup for disease modification. It seems like, in some ways, talking or seeing what's going on in the Alzheimer's space, that paradigm is somewhat being thrown out in Alzheimer's disease modification versus symptomatic. And so we seem to be that symptomatic therapy in FA would be quite valuable as well, do you have an argument for that to go to the agency with?
Warren Huff -- Founding Chief Executive Officer and President
Yes, and the point about the analysis is not whether or not a purely symptomatic treatment would be approvable, it clearly would be approvable, and they haven't indicated that there would be any problem with the approval of Omav for FA if the treatment was only symptomatic. In fact, they made clear that's not the case. The question really goes to the ethicalness of conducting a second study. Once you've demonstrated in a randomized controlled trial a disease modifying activity then it's much more difficult to ethically justify a second randomized controlled trial.
Charles Duncan -- Cantor Fitzgerald -- Analyst
Especially in an orphan indication. Appreciate taking the question.
Warren Huff -- Founding Chief Executive Officer and President
Yes exactly, especially in a deadly disease with no approved therapy. Yes, exactly.
Operator
Our next question comes from Joseph Schwartz from SVB Leerink. Please go ahead with your question.
Joseph Schwartz -- SVB Leerink -- Analyst
Great, hi. Thanks so much for the detailed update. I was wondering if you could talk about the patient inclusion methodology and criteria that you propose to the FDA for your proposed Alport indication in the NDA for bardoxolone? And how many patients with these characteristics would you estimate are addressable at the sites that you're targeting or focusing on for commercialization?
Warren Huff -- Founding Chief Executive Officer and President
Right, just so you're asking about like what patients would be included essentially in the label?
Joseph Schwartz -- SVB Leerink -- Analyst
Yes, essentially and just in order to exclude patients that are too far advanced or otherwise not well suited for treatment, you've found early on in development in the Type 2 diabetic CKD studies?
Warren Huff -- Founding Chief Executive Officer and President
Yep, sure. Colin, would you like to comment on that.
Colin Meyer -- Chief Research & Development Officer and Executive Vice President
Sure, we think that the label would likely, in general, reflect the patients that we enrolled in CARDINAL. And so there's a broad age and GFR range, the call that the eligibility criteria where age as low as 12 highest 70, eGFR 30 to 90, above 90 is basically normal. And we enroll patients with all genetic subtypes. And then as you alluded to, we excluded patients who had a significant cardiovascular history and BMP over 200 pica grams per mil, indicating that those patients were already retaining fluid. And, as I think I've mentioned probably a couple years ago, once we completed enrollment, very few patients discontinued. I'm sorry, we're not eligible to enroll because of your significant cardiovascular history or elevated D&P. So we think that those patients would represent a very small proportion of patients with Alport Syndrome. And in general, we'll have to obviously negotiate the label with FDA to figure out specifically what it states and so they may draw a hard line with some of the criteria or it could be left open for interpretation by the treating physician. But overall, we believe that it's likely to represent, a large percentage of patients who have impaired kidney function, who have not reached the need for dialysis or transplant.
Manmeet S. Soni -- Chief Operating Officer & Chief Financial Officer and Executive Vice President
Hey Joe, this is Manmeet. And I can give you some numbers for the here, right. In terms of the total overall prevalence opportunity, I think we believe Bard could address the high unmet need in the estimated population of 30,000 to 60,000 patients with Alport Syndrome in the United States and approximately 30,000 to 60,000 patients in the EU five. But if you look at the claims data, which came in recently to the IQ claims data, there are approximately 14,000 projected patients diagnosed with Alport Syndrome in all the stages of CKD in the United States. And as you know, like many other rare diseases, and this is a -- there is no approved therapy, right, there is no incentive for physicians to diagnose and identify patients, and we believe many patients go unrecognized, or undiagnosed, or even misdiagnosed until treatment will be available. And so we are deeply committed in identifying those patients. And as you remember, last year, we initiated a genetic testing program, kidney code, which was initiated to improve the accuracy and timeliness of diagnosis in the United States. And we were pretty impressed right with the initial data which we received. And you would have seen our papers in the ASN where many new patients were diagnosed with kidney code, and those patients were earlier misdiagnosed. So I think it's too early to give you a specific number today, but we believe the opportunity is pretty big. And it will continue to expand as we continue with our commercialization efforts and with our medical affairs teams, which we have already initiated to make sure that education and awareness and genetic testing is made available to physicians and that will keep expanding the market by itself calling. Colin or Warren do you want to add anything?
Warren Huff -- Founding Chief Executive Officer and President
No, I think you covered it.
Joseph Schwartz -- SVB Leerink -- Analyst
Thank you very much.
Operator
[Operator Instructions]
And our next question comes from Matt Kaplan from Ladenburg Thalmann. Please go ahead with your question.
Matt Kaplan -- Ladenburg Thalmann -- Analyst
Hi, good morning guys. And congrats on the progress. Wondered if you could give us more information in terms of your strategy with the launch of the MERLIN study and rapidly progressing patients with CKD. And in the context of your plans to initiate additional studies in other CKD indications which you studied before, in terms of IG nephropathy, Type 1 diabetes, and FSGS. What are your thoughts in terms of how MERLIN fits in and that indication fits into your kind of regulatory strategy for bardoxolone?
Warren Huff -- Founding Chief Executive Officer and President
Yes, so Matt you're asking about how MERLIN fits into our overall development strategy in CKD. And Colin would you like?
Colin Meyer -- Chief Research & Development Officer and Executive Vice President
Yes. Would you like to comment on that column? Sure. And so as we've demonstrated, you know, in Phoenix, and Cardinal elites observed activity in multiple forms of CKD, it's six or seven now. And we decided to pursue Phase 3 studies with two of those indications, obviously -- first and ADPKD second. When I actually think about how we progress further with development, there's really no two main paths. One is to do single indication studies, so another FALCON and another CARDINAL, which in general would probably require 300 to 400, maybe 500 patients each depending upon the application and powering assumptions. The other opportunity is to do a single study that allows us to enroll patients with multiple different etiologies who have this common theme of likely some intrinsic defect in the kidney that puts them at a very high lifetime risk of progression to kidney failure, where we can also exclude patients who perhaps have significant cardiovascular comorbidities that may be targeted by other agents such as ACE inhibitors, A or B, specialty inhibitors, etc. So the data from CARDINAL really struck as some of these patients have substantial loss of kidney function despite receiving ACE inhibitors and ARBs. Once again, the pediatric data really, really highlights that with losses of 15 -- in two years. And so we've thought about a way where we can, once again enroll patients with a common phenotype, who meets one of the few eligibility criteria for rapid risk of progression. And where we can really increase the value to patients as well as to prescribers for use of bardoxolone, and differentiate the drugs versus you know, for use of bardoxolone. And differentiate the drugs versus other agents that effect blood pressure or have cardiovascular benefits. And so the MERLIN trial is a way for us to tune up the eligibility criteria, look at enrollment across sites, and try to figure out how best we could operationalize a future Phase 3 trial. That if we did proceed, would likely allow sufficient patients to be able to power up for an actual outcomes composite, which would obviously be a very strong label, if we're able to demonstrate a difference in outcomes.
Matt Kaplan -- Ladenburg Thalmann -- Analyst
Great, that's very helpful. Thanks for the added color.
Operator
[Operator Closing Remarks]
Duration: 64 minutes
Call participants:
Warren Huff -- Founding Chief Executive Officer and President
Colin Meyer -- Chief Research & Development Officer and Executive Vice President
Manmeet S. Soni -- Chief Operating Officer & Chief Financial Officer and Executive Vice President
Yigal Nochomovitz -- Citigroup -- Analyst
Maury Raycroft -- Jefferies -- Analyst
Annabel Samimy -- Stifel -- Analyst
Brian Skorney -- Baird -- Analyst
Charles Duncan -- Cantor Fitzgerald -- Analyst
Joseph Schwartz -- SVB Leerink -- Analyst
Matt Kaplan -- Ladenburg Thalmann -- Analyst