Image source: The Motley Fool.
American Well Corporation (AMWL -2.13%)
Q4 2020 Earnings Call
Mar 24, 2021, 5:00 p.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Good afternoon, and welcome to Amwell's fourth-quarter and full-year 2020 conference call. [Operator instructions] Please be advised that today's conference is being recorded. Leading today's call are Dr. Ido Schoenberg, chairman and co-chief executive officer; and Keith Anderson, chief financial officer.
Ido and Keith will offer their prepared remarks, and then they will take your questions. The Amwell press release and webcast link are available on the Investor Relations section of Amwell's website. Please note that we will be discussing certain non-GAAP financial measures that we believe are important in evaluating Amwell's performance. Details on the relationship between these non-GAAP measures to the most comparable GAAP measures and reconciliations thereof can be found in the press release that is posted on our website.
Also, please note that certain statements made during this call will be forward-looking statements as defined by the Private Securities Litigation Reform Act of 1995. Such forward-looking statements are subject to risks, uncertainties and other factors that could cause the results for Amwell to differ materially from those expressed or implied in this call. And now I'll turn the call over to Dr. Ido Schoenberg, CEO of Amwell.
Ido?
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Good evening, and welcome to our 2020 fourth-quarter earnings call. 2020 was a significant year in many ways, especially in the world of healthcare. The pandemic stressed and challenged the entire healthcare ecosystem. Throughout the pandemic, Amwell empowered the providers of healthcare to continue to deliver care to their patients and also care for greater numbers of patients through virtual and remote care.
The pandemic, while terrible, only accelerated our transformation impact timetable by about three to five years. Patients and members have now embraced receiving care virtually. Providers of care are comfortable, in some cases, encouraging delivering care virtually to their patients across the care continuum, well beyond rudimentary urgent care or pre-pandemic telehealth-focused. The pandemic did not stop doctors and nurses [Inaudible] many of the new practice delivering care to their patients.
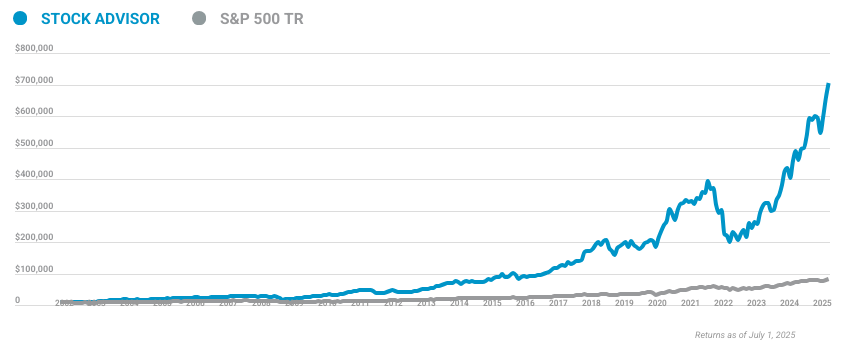
10 stocks we like better than AmWell
When investing geniuses David and Tom Gardner have a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
David and Tom just revealed what they believe are the ten best stocks for investors to buy right now... and AmWell wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of February 24, 2021
For example, we powered cardiologists, whose offices were abruptly closed, to enable them to continue seeing their patients and monitoring them remotely. We help obese, sick pregnant mothers as they progress through their pregnancy and enabled endocrinologists to follow up on their diabetic patients. In other words, the pandemic highlighted the power and differentiation of the Amwell platform. We're able to demonstrate how the Amwell platform could enable overall care delivery in the new hybrid world.
In 2020, we delivered over $245 million in revenues and are forecasting between $260 million and $270 million for 2021, representing a growth of over 35% over the last two years. In 2020, our platform supported 6 million visits, which is about five times the volume we saw in 2019. Most importantly, we added over 65,000 active providers to our platform, bringing the total number of active providers to over 72,000 at the end of the year. It was incredible to see that 68,000 of them who are not our AMG providers, but rather our clients' own providers.
During this transformative year, we worked with admiration the selfless work of our clients and partners, especially the healthcare providers in their heroic and courageous fight against COVID. Prior to the pandemic, and even in January of 2020, many view telehealth as complementary optional replacement service to simple urgent care. We now proved that this utility is only a small part of telehealth. COVID helped solidify Amwell's role of enabling digital care delivery infrastructure across the entire healthcare continuum.
It rapidly became apparent that telehealth does not replace in-person care. Instead, and especially for Amwell, it complements it and can be instrumental in strengthening existing patient-provider relationship. For example, the Chartis Group estimated that over 50% of visits were done virtually at the height of the pandemic, up from less than 1% before COVID. And today, the analysis is showing that the proportion of visits conducted virtually has stabilized around 15% to 20%.
Also, according to McKinsey, health systems, independent practices and other providers saw virtual visits increased by 50 to 175 times compared to pre-COVID, and more providers, 57% view telehealth more favorably than before COVID, and 64% are more comfortable using it. Our conversations with payers and providers also changed substantially in 2020 through focusing on affordable complementary services to empowering mission-critical technology. Digital connectivity enablement became a high priority for most of our clients and partners. Simplicity, reliability, modularity, extensibility and efficiency took priority over other features and functions.
The ability to integrate with existing digital assets through easily supportable solutions also became very important. We are very attentive to the new market needs and took significant measures to quickly address them. We saw visits in April 2020 as high as over 40,000 per day versus approximately 5,500 in January. Reacting to the tidal wave of demand, we grew capacity by about 10 times in 2020.
We launched a series of platform modules and care points aimed to dramatically simplify connectivity and make it more accessible and affordable. We also streamlined integration with many other assets of our clients and partners. These innovations also included the super simple and popular Amwell Now that help and is helping further accelerate provider adoption across delivery networks. They also include a deeply integrated Amwell Connect EHR module, the new affordable Amwell Touchpoint Tablet, the Amwell C500 Carepoint that is both home and hospital enabled and the revolutionary Amwell Hospital TV Carepoint that we discussed on our Q3 call.
We experienced significant growth across all segments of our business last year. Compared to 2019, in 2020, active client providers grew over 13 times from 5,000 to 68,000. We grew total visits five times from over 1 million to 6 million. Client provider visits accounted for over 70% of our total annual visits, up from 35% in 2019.
And AMG provider visit volume more than doubled from 750,000 to 1.6 million. Maybe even more important within our visits results is the continued shift to specialty visits. Behavioral health visits grew by 1,000%, surgical care grew over 2,000% and dentistry doubled. These trends created clear separation between Amwell and legacy telehealth players, aiming to offer affordable and convenient alternatives to physical services.
We have always focused on enabling and empowering trusted payers and providers and not on creating alternatives to their offerings. The transformation in the market's view of telehealth from a service to a platform is fast and profound. As the pandemic stabilized late in 2020, most of our clients began preparing to significantly expand the frequency and scope of use of our platform. In reaction to this tectonic market shift, we decided to accelerate our investment in innovative technology that powers our platform, as well as its models and programs.
Looking ahead, we see a rapidly evolving landscape in which trusted healthcare players develop hybrid model of care. They increasingly rely on Amwell to deliver an easy to use yet comprehensive platform to enable the full spectrum of their telehealth needs. Importantly, this care will be longitudinal, enabling the relationship between providers and patients over time, as well as supporting interdisciplinary team-based care delivery models. We recognize that many of our clients and partners have their own preferences and investments as it relates to telehealth-adjacent technologies, like navigation or remote patient monitoring.
We are, therefore, making sure that our platform does not overlap or compete with these assets, but rather makes it seamless for our clients and partners to integrate and embed their own choices. In 2021, we will continue our investment in our post-COVID technology platform buildout that we briefly discussed on our third-quarter call. We named the next release of the rapidly evolving annual platform Converge. At our upcoming client forum on April 28, we will present it and feature new functions and dynamics.
In advance of the forum and to help you frame our future and outlook for 2021, I will share that the key focus of Converge is the continued evolution of enabling care from episodic to longitudinal with the current relationship at its core. It also provides new possibilities for our clients, partners and third parties to further expand and diversify use cases enabled through our platform. The combination of our technology and its ubiquitous adoption across the ecosystem are likely to generate significant long-term competitive advantage for Amwell. Converge capabilities will also expand our TAM by both increasing our value to existing clients and opening new markets and opportunities for us.
The release of Converge is an important multiyear milestone for Amwell. An early example of our new longitudinal capabilities is demonstrated in the virtual primary care module, which we recently deployed. We believe that our VPC module is demonstrative of how healthcare will be experienced in the future. It provides patients a simple and convenient choice of online and in-person options, including referrals, imaging and lab services.
It preserves the long-term and recurring relationships with the primary care providers and others, while allowing payer sponsors to control utilization patterns without compromising our member experience, trust, quality and value. We are excited about the technology innovations we will present to the market this year. I encourage our investor partners to attend our client forum in April. We believe that our innovative solutions uniquely address a strong and urgent need in the market.
And now I would like to turn the call over to Keith to review our financials.
Keith Anderson -- Chief Financial Officer
Thank you, Ido, and good afternoon, everyone, and thank you for joining us for our fourth-quarter call. Before diving into our detailed results, I want to reiterate Ido's comments about how pleased we are with how we ended the year, and I'm happy to report that we have exceeded every forecast metric and are seeing continued momentum across all of our business lines. The conversations we are having with our current and prospective customers highlights their acknowledgment of the unique capabilities of our platform to deliver true longitudinal care, coordinated by your health plan or your doctor. This team has been the core of our strategic partnership conversations as we believe the new healthcare will require coordination of a full spectrum of care.
Now a couple of points on our full-year 2020 performance before we dig into the quarter. We ended the year generating over $245 million in revenue, which equates to 65% growth over the prior year. A large part of this growth was due to subscription average contract values expanding from $282,000 to $334,000 in 2019 to 2020 for our health system customers and from $546,000 to $612,000 for our health plan customers. The number of health system customers also grew from 140 to 158 in 2019 to 2020 and from 56 to 58 for our health plan customers.
In terms of active providers, at the end of the year, there were over 72,000 active providers on the Amwell platform delivering care to their patients. While this is a 10 times increase over the prior year and highlights the hard work of our team, in many cases bringing full hospital system doctor groups on the platform in rapid fashion, the explosion of our customers' own providers plugging into the Amwell platform is the most important long-term metric as these non-Amwell doctors grew 13 times from 5,100 providers in 2019 to over 68,000 at the end of 2020. As referenced, during the same period, the number of our own AMG providers grew from over 1,800 in 2019 to 4,500 at the end of 2020. As we first highlighted during the IPO and then on our Q3 call, this intended shift in care delivered by our customers' own providers is a critical dynamic that has been accelerated by the pandemic.
To illustrate, 66% of all visits in 2019 were performed by Amwell providers. In 2020, this dramatically shifted to where almost 70% of all 5.9 million visits, or 4.3 million, were performed not by Amwell providers, but by our customers' own providers. Reminding you that one of the primary tenets of Amwell is not to compete against the providers of healthcare, but to enable and facilitate their ability to deliver care to their patients. It is a fundamental difference in our business model that will allow Amwell to capture the network effect of care delivered virtually and all its surrounding coordinates for longitudinal care.
Now turning to our fourth-quarter financial results. I'm happy to report total revenue of $60.4 million, which is a 34% increase this quarter last year. Our subscription revenue came in at $26.3 million. The 15% increase over the previous year can be attributed to new customers, expanded programs within the health plan populations and an increase in the volume of platform visits performed by our health system and health plan customers' own providers.
In terms of visits, our visit volume remains elevated in comparison to pre-COVID-19 levels, driving a steep increase in our visit revenue, which totaled 26.2 million this quarter, up 75% over the previous year. In this quarter alone, 1.6 million visits were performed on our platform, bringing our total visits in 2020 to over 5.9 million. This is up 11% sequentially versus the 1.4 million visits performed on the platform in Q3. As we forecasted, we saw AMG visits decline 5% sequentially from Q3.
But within AMG visits, it's notable that we continue to experience significant growth in AMG specialty visits, which is on top of the dramatic increase in Q3 over and above Q2, which was the peak of the pandemic. This shift to more specialized visits versus simple urgent care has driven our average price per visit up to $73 per visit in 2020 versus $54 per visit in 2019. As I stated earlier, we continue to experience outsized usage of our platform by our customers' own providers. And 77% of all visits performed on the platform were conducted by our health plan and health system customers' own providers.
Recall, this percentage was 73% last quarter. So the dynamic in Q4 was similar to the peak of the pandemic in Q2, an overall trend that we see continuing throughout 2021 as healthcare delivery systems move to more hybrid care models, combining physical and virtual care. Our services and care points revenue of $7.9 million was an increase of 10% year over year, but a decrease of 5% compared to last quarter where, if you recall from our third-quarter call, we discussed some pull forward buying into Q3 due to the expiration of the CARES Act and the spending of these remaining funds in Q3. Gross margin for the quarter was 37.4%, compared to 32.7% last quarter versus 44.7% last year.
Versus last quarter, we continued to realize additional high-margin subscription revenue due to those contracts that contain volume components. The year-over-year margin decrease was a direct result of revenue mix shift to more visits versus 2019. G&A expense experienced a 36% decline versus last quarter as our IPO occurred in Q3 and there were related one-time noncash stock-based comp awards to our executives that were triggered by our successful IPO. With the IPO now behind us, Q4 G&A resembles a more normalized spend level in the mid-$20 million range.
We are reporting an adjusted EBITDA loss of $35.4 million, compared to $16.9 million loss last year. On a macro level, this was due to revenue mix shift to lower margin visits, continued investment in the platform and expenses incurred typically of a public company versus last year when we were private. From a balance sheet perspective, we ended the year with cash and investments of approximately $1 billion, and Amwell continues to have no debt. Now turning to forward guidance.
For the full-year 2021, we expect revenue to be in the range of $260 million to $270 million, representing a 35% compound growth over 2019. Similar to 2020, we are expecting visit revenue to account for approximately 50% of overall revenue, driven by forecasted visit volumes between 1.5 million and 1.7 million AMG visits. We are forecasting an adjusted EBITDA loss between $157 million and $147 million. As we did during our IPO in an effort to be transparent and give it all the moving parts and uncertainty amid the COVID-19 crisis, I want to provide a few high-level thoughts on framing 2021.
Most notably, we are projecting in 2021 AMG visit volumes at levels similar to during the pandemic with the midpoint of our range at 1.6 million visits, the same volume as we delivered in total in all of 2020. Now that is an important data point, as said differently, we see visit volumes coming out of the pandemic as foundational and not episodic. The underlying data supports that both our provider and health plan member customers have embraced delivering and receiving care virtually and are doing so on the Amwell platform. While we're projecting more normalized flu season later in 2021, we continue to observe a mix shift toward specialty visits, whereas urgent care and thus, are forecasting revenue per visit to continue to increase to around the $80 per visit range versus $73 in 2020 and $54 in 2019.
Subscription revenue from our innovator customers and revenues from sales of our care points and services are projected to return to more normalized levels as discussed during our IPO. Regarding R&D spend, as Ido discussed earlier, and we highlighted on the third-quarter call, we expect R&D expense as a percentage of revenue to continue throughout 2021 at the same levels as the fourth quarter of 2020. This temporary increase is driven by foundational changes in customer sentiment to use digital connectivity as part of mainstream healthcare. And thus, we have decided to accelerate the Converge platform project in advance of these longitudinal care-type products.
We'll talk more about this at our upcoming client forum in April. For the first-quarter 2021, we are expecting revenue will be lower than in the fourth quarter of 2020, in part, simply because of a fewer number of days, but more so the churn of two large contracts due to M&A that we identified and discussed during our IPO. Also, the run-up care points in Q3 and Q4 of last year pulling revenue forward into those quarters and out of the first quarter of this year; and finally, specific educational marketing campaigns by the health plans that occurred in the fourth quarter of last year. Looking beyond 2021, the Converge platform will expand our TAM through expanded partnerships and functionality and is the basis of some of our inorganic strategic discussions related to longitudinal care.
I want to highlight, though, that while we have accelerated this platform investment into 2021, our time line to achieve EBITDA profitability remains unchanged. In closing, I'd like to reiterate how pleased we are to report yet another strong quarter as this is only our second quarter since becoming a public company. I look forward to reporting progress toward our goals and forecast this year in 2021. We are well capitalized for growth and positioned to maintain a leadership position in the telehealth market, and I look forward to supplementing this foundational growth with our inorganic strategy.
With that, I'll turn the call back to Ido for his closing remarks.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Thank you, Keith. I want to thank all our incredible team members for their hard work over the year, supporting our customers and partners during their challenging times. It is clear to me that our platform enhances providers' abilities to deliver high-quality care to their patients today. The investments we are making will help us continue that well into the future.
With that, operator, we'll open the call to questions.
Questions & Answers:
Operator
Thank you. [Operator instructions] Your first question comes from the line of Ricky Goldwasser with Morgan Stanley. Your line is open.
Ricky Goldwasser -- Morgan Stanley -- Analyst
Yeah. Hey. Good evening. And congrats on the quarter and guidance.
Clearly, there's a lot of demand for your services. You are putting forward the investments in new product development. When we think about your long-term guidance of 20% to 30% top-line growth that you provided at IPO, is that the right way for us to think about jumping into '22? What do you think about 2022 and beyond? Or are you now seeing sort of a step-up in demand that is shaping how you think about that long-term revenue opportunity? And then somewhat related, Keith, you talked about the revenue per visit assumption of $80. What are the underlying assumptions that you're making regarding reimbursement for telehealth visit in any potential changes in the parity versus in-person or rebasing it to a different level?
Keith Anderson -- Chief Financial Officer
So Ricky, I think there was about five questions embedded in that. I'll take the first couple, and then I'll hand it over to Ido to talk about reimbursement and then some of the more conceptual answers to your last question. Yes, we are seeing -- so I mean, to answer your first two questions, we are seeing a step-up in demand. We are going to stick with what our IPO revenue growth targets were right now, but we look forward to updating you throughout the year, especially coming out of the client forum in April that I'm hoping you'll attend.
We are seeing the TAM expand through the platform expansion. And we are already achieving, as I mentioned, if you normalize for the two contracts, we actually are in the mid-20s percent growth this year for subscription. So yes, we are sticking to what we said during the IPO in terms of long-term growth, but we will update that as we go through the year. In terms of the price per visit.
We're staying around the $80 range, but it's -- the shift that happened in Q4 is continuing in Q1 to more specialty. And going back to what the overall mission statement of the business is and what our strategy is, it's to provide backup supplemental care and really empower the providers of care, your doctor, your health plan and the health plans' own providers to deliver that care. So we're seeing urgent care become more secondary, specialty care become more primary as we support those providers of care. So we're seeing, as Ido quoted, some explosive growth on our specialty side.
It's now making up about half of our overall visit volume, which is exciting. And that's what's driving the $80 range revenue per visit. In this last quarter, we saw significant growth on our platform providers. Those are non-Amwell doctors delivering care on the platform.
Sequentially, that was north of 15% quarter over quarter. So the shift we saw in Q4, and we're seeing continued into Q1 of this year. Ido?
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Thank you, Keith. And Ricky, it's good to hear your voice. One cannot overstate the enormity of what happened in 2020, and I think it will take years to fully understand it. The trend is very palpable, although the velocity of the change is hard to predict.
Therefore, we are very comfortable with our -- reiterating our growth assumptions going forward not ignoring the enormous upside that still exists. If you need to summarize the trend, telehealth moved from an alternative acute care service into an enabling platform, which is part of everyday healthcare. We've talked about it only a year ago as a vision, and it really has become a reality. We believe, especially with the release of Converge, that our technology gap as an enabler is significant.
And we think that the number of providers adopting it is a great indication of what's going to happen going forward. So we are very comfortable stating that we believe that there'll be a preference toward technology revenue that is obviously infinitely more efficient and much more scalable going forward. And we're going to learn a lot this year about the velocity of this change. And when we have more data, we could come back and reanalyze our future guidance.
Operator
Our next question comes from the line of Robert Jones with Goldman Sachs. Your line is open.
Robert Jones -- Goldman Sachs -- Analyst
Great. Good evening. Thanks for taking the question. Keith, I appreciate all the data points you shared, particularly as it relates to 2021, but I was wanting to get maybe even a better sense of what you're expecting as it relates to the health systems and health plan expectations for new adds and revenue.
If I heard you correctly, it sounds like you're expecting AMG will make up about 50% of revs. It sounds like the innovator revs will be a little bit better than what you saw. And so looking at that -- what that means on just projections for subscription, it seems like a little bit of a deceleration, if I'm thinking about that right. Anything more you're willing to share just around what underpins the assumptions on the health system and health plan subscription assumptions for the guidance?
Keith Anderson -- Chief Financial Officer
I mean it's -- for the health systems, it's adding new health systems, as well as the expansion of the average contract value. So when you saw our average contract value expand nicely, as I said on the call, we see both of those dynamics continuing to happen into 2021. So the name of the game there is land and expand. So landing new hospital system logos, expanding the current customers that we have through both the rollout of additional modules, as well as getting back to the cellphone plan we, want their providers to deliver more care virtually.
So those visit counts adding into the subscriptions, that was part of the increase in Q4. So we're seeing that happen. On the health plan side, just to be complete, there is more expansion through the population, expansion of new programs like virtual primary care and other programs out to the membership base. So it's land and expand on the system side, and expansion through the population on the health plan side.
Robert Jones -- Goldman Sachs -- Analyst
OK. So if I'm hearing you correctly, not a big deviation from what you had talked about before as far as new additions for health systems or health plans in '21?
Keith Anderson -- Chief Financial Officer
We would say that our conversations are really exciting in terms of pipeline, in terms of the -- and I guess, Converge, if you look at the announcement of Converge, that's a reflection of the level of conversations we're having with our partners. These are the biggest players in the space, and it shows the demand there to deliver the care on the platform. So they were bringing forward their designs for longitudinal care and what they wanted to do virtually on the platform so we had to accelerate our expansion on the platform. So we're really encouraged and excited about the level and depth of the conversations we're having.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Just to add detail. When you analyze what is subscription revenue, subscription is recognized revenue for an enterprise implementation of the hospital or a delivery network. It's safe to assume that in 2020, everybody was focused on their day job and the idea of implementing new infrastructure is really far and foreign for everybody. It's also safe to assume that everybody is up right now.
Everybody realizes that you have to have digital connectivity infrastructure really in order to survive and in order to grow. And that's the conversation that Keith was alluding to. The discussion there is not about the price of AMG doctors or the capacity of doctors that we have. The whole discussion is about simplicity integration, modularity, scalability and other -- many other features or functions where we believe we have a significant advantage around.
So overall, when you think about subscription revenue, we're actually fairly bullish when we look into the future.
Robert Jones -- Goldman Sachs -- Analyst
Got it. It's helpful. Thank you, both.
Operator
Your next question comes from the line of Sean Wieland with Piper Sandler. Your line is open.
Sean Wieland -- Piper Sandler -- Analyst
Thank you. So what can you tell us about the virtual primary care launch with United that you announced? Can you size that for us with respect to the '21 guidance and give us a little bit more detail on that launch?
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
So Sean, terrific to hear your voice, and thank you for joining the call. You know that we cannot discuss any specific client's details and numbers. That is something that we really care deeply about. However, I'm glad that you brought the topic of virtual primary care modules and programs, which we believe are very important.
And as I said on the call earlier, really a way that most people, in our opinion, would experience healthcare going forward. So for those on the call that are less familiar, this is the technology and service infrastructure that allow people to start their interaction with the healthcare system, not only telehealth, but the entire healthcare system online. So you go online, and then you have a highly personalized experience using artificial intelligence and very empathetic people that offer you a choice of the entire spectrum of services, from online programs and people to labs, imaging and physical referrals. This infrastructure is really designed from the get-go to encourage and support recurring longitudinal relationship.
So for the consumer, it really is a wonderful way to experience healthcare. It's trusted, it's immediate, it's personal. It has an element of choice. For the payer sponsor, for the risk bearer, it's an opportunity to really renegotiate the network and the options that you see and to make it also very efficient financially.
We are very glad that very large client chose it as its backbone. And we will let this client and others tell the market when they're ready about their experience. But when you talk about the superiority of our technology, whether it's Converge and future primary telehealth definitely part of that family, part of our platform, and when I said I was bullish about the future, this is definitely part of what I meant.
Keith Anderson -- Chief Financial Officer
So Sean, if I could -- yeah. I mean to go a level deeper for your model. So there's two parts that I see of revenue coming out of -- on virtual primary care. There's direct and indirect.
On the direct side, there is an access fee that is either paid in per member per month or a blanket access fee, depending on the plan that we are working with. There's a transaction fee. And this is the interaction with the member by the plan provider. And this is really where it's all going and what got those plans that we -- have been announced, as well as plans we're talking to get them really excited.
And then there's the clinical fee because this is a new way. I mean this is full longitudinal, full spectrum, fully coordinated care that is being delivered on our platform. And so that takes time to bring their doctors up to speed on how the coordination of care is going to impact them, where they need to plug in, where they need to have a primary node coordinator. So as backup, we have our AMG doctors at the ready that if someone has a bad experience using virtual primary care for the first time, they're not going to use it again.
So our doctors -- and I'll get to the visit impact in a second. Our doctors, we are assuming, are going to be helping out, in the beginning, a lot, and tapering off as more and more of their doctors become part of the care coordination plan. Then there's the indirect part. This is fully coordinated longitudinal care, at least that's the thesis of our partnership with the one customer that you referred to.
So there's a lot more programs. This is a goal for us and a goal for them, bringing more programs, bringing more coordination, bringing more holistic care to the front to deal with these members. There's also maybe RPM. I mean to be able to, regardless of the age, add some of the RPM functions that I'll let Ido comment about in a second.
But as it relates to the visits, this is an important point. We are projecting or forecasting the same number of visits in 2021 as 2020, but the components are really different. There was a significant number of visits that were performed in March, April, May that were just simple one-off urgent care demand, OK, I think I have COVID, dealing with different components. That has completely shifted in our 2021 forecast, where those components are being replaced by our specialists, being replaced by their provider doctors, your doctor plugging in and delivering care to you.
So a big part -- not a big part, but a component of the visit forecast, the same number ZIP code as 2020, includes those virtual primary care, back-up care, our AMG doctors. So Ido, do you want to talk about some of the other components that we see coming in as the indirect revenue that we've been talking about?
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Yes, absolutely. Thank you, Keith. I mean, Sean, just -- I wish we could talk more freely. But as I said earlier, we're limited about what we can say about some specific clients.
But to help you understand the dynamics, implementing virtual primary care is a no-brainer for a payer for obvious reasons. It's so efficient, it's so member-friendly and things of that nature. The way we monetize that infrastructure is: a, by technology subscriptions; b, by the volume, how often this technology is being used; and then by the scope of services, more modules, more programs; then there are clinical fees. So all these are direct fees that relate to the scope of deployment.
No one is deploying this overnight nationally. We deploy it over time, state by state. It's staged. You add more modules, you add more programs, but the direction is very steady.
And we know this is going because it adds so much value for everyone. The indirect effect is even more profound because, as you remember, unlike others, we have one platform and it's all connected. So imagine that the option that you see on the virtual primary care platform are excellent centers that are also Amwell clients. And because we allow them to change the business model, in participating very large payer programs, they become more sticky and we become more valuable to them as well.
On the flip side, the ability to tie this service with additional services, scheduled visits, the urgent care visits, a million other things that we're doing with people on one platform, is extremely valuable for others because it's not stand-alone. The fact that our platform is modular, the fact that we don't compete with our clients and partners is very important. We don't try to push our AMG providers and replace them with other providers. On the contrary, we use them as a support mechanism to really foster existing patient provider relationship.
And therefore, the acceptance and the likelihood to offer a greater choice and greater capabilities on our platform is much greater versus other people that are trying to do with this.
Sean Wieland -- Piper Sandler -- Analyst
Thank you for that. Very quick follow-up. Is all of the above material or immaterial to the '21 revenue guidance?
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Well, it's included in the guidance. And we have certain assumptions that have. We are very comfortable with our guidance. As I said, there is always a possibility to sometime do more, but we are not ready to go there yet.
A lot of the progress of deployments like that depend on factors that we simply don't control. They are driven by the clients, by the market, by other factors. And we really want to make sure that our guidance is extremely robust, and that's what we did.
Keith Anderson -- Chief Financial Officer
I mean they're rolling it out state by state. We're very comfortable with our guidance. I guess that's our response to the question, Sean.
Sean Wieland -- Piper Sandler -- Analyst
OK. Thank you very much.
Operator
Your next question comes from the line of Kevin Caliendo with UBS. Your line is open.
Kevin Caliendo -- UBS -- Analyst
Great. Thanks. Thanks for taking my call. I'd love to get your guys' take on the market consolidation we've seen in the last couple of months in the telehealth space.
There's been a couple of higher profile deals. In any way, shape or form, does that impact the landscape for your competitive positioning? Or how you think about the opportunity set? And also, M&A was always going to be a big part of the story, we thought, going forward, and we still expect it to be. We'd love to hear your take on your M&A pipeline, the valuations in the marketplace currently to that end. Thank you.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Hi, Kevin. And again, it doesn't really count like a question, but I'll take it as one. We are very clear about who we are and what our strategy. For example, in order to be an efficient connector, you cannot be owned by one of the targets.
That doesn't really work. It creates bias, and it does create a problem. So when a telehealth operator is -- gets acquired by a health plan, that's a helpful dynamic for a competitive situation because, obviously, many of the target clients are less comfortable interacting with that vendor. Now that the ownership of the plan necessarily is proper for healthcare play, unless you believe that it's a utility or service plan.
So that's good. On the other hand, we see some M&A activity with people that are trying to construct a longitudinal solution in the sense of doing more than one thing, doing telehealth and doing navigation and transparency, for example. We think that while it may look impressive in world numbers then and in scale, that's a mistake. When we talk to many of our customers, they have strong opinions about the different components they're going to build.
Digital connectivity platform is definitely a clear option. And hopefully, they choose us as often as possible. But then they have a strong opinion about other elements that they want to pile on top of it. The ability of platform to interact with those solutions is much more important than bringing the entire solution yourself.
And there are many examples where you see that a one telehealth company began to sell longitudinal program to chronic illness and things of this nature. And several clients really had hard time swallowing the entire thing. We believe that the whole point of integration is diversity and inclusion in the sense that you let others excel at what they do, and you remain incredibly true to yourself going forward. As far as the M&A, we will -- we are and will continue to look at options to further improve the value and competitive advantage of our platform and our technology.
That's the most important thing for us. We help our clients improve patient outcomes, clinical and financial. I'm sure that it's not lost on anyone on the call that a few months from now, valuations were much higher than they are today, and that's a good dynamic. Some of the spec activity is a little different than it was before, and that's a good dynamic.
We are going to be incredibly careful as we look for great opportunities to grow organically, inorganically from a strategic plan, but also from a valuation and monetary lens. And we are very encouraged by the fact that the market is going back to reality in some cases and the opportunities become much more attractive.
Keith Anderson -- Chief Financial Officer
I mean we're having -- as head of M&A, we're having a lot of conversations. That's the beauty of the platform as you can plug them in, you can integrate them quickly. Some of the different areas that Ido said on his prepared remarks, of the TAM expansion, we are focused internationally. We are focused on different functionality aspects of the platform so that it can be used in even more settings.
The partnership with Google is opening up opportunities that are beyond what we had when we went public last year. So we look forward to continuing to execute on the inorganic strategy and making announcements at the appropriate time.
Kevin Caliendo -- UBS -- Analyst
That's really helpful. If I can ask a quick follow-up. Pulling forward the R&D spend for Converge, is it fair to assume R&D should maybe decline in 2022? Maybe without guidance -- you have to provide guidance in 2022. But maybe just thinking about the color of cadence on spend is in the road map?
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Temporary increase. It really was being driven by our customers. I mean -- and it's a reflection of our conversations with them. So we were looking to methodically roll out these different functionalities over a longer period, over the next two to three years.
But virtual primary care is one example. The functionalities that -- beyond the one health plan we're working with, the other ones that we're in conversations with, we're asking for these things to be enabled on the platform. So based on all of those, we've accelerated the different aspects of the platform into 2021. It is temporary, and it will go back to more normalized levels in 2022.
Kevin Caliendo -- UBS -- Analyst
Great. Thanks so much, guys.
Operator
Your next question comes from the line of Jailendra Singh with Credit Suisse. Your line is open.
Jailendra Singh -- Credit Suisse -- Analyst
Good. Thank you. I know, Keith, you just touched upon this Google partnership. I was just trying to ask that more broadly.
You have these several interesting partnerships going on in terms of Google, Cleveland Clinic on expert opinion services. I was wondering if you could provide some color around how much, if any, revenue contribution or margin benefit is captured in your 2021 outlook? Or even just more broadly, maybe elaborate more on your Google partnership in terms of some more tangible benefits we should expect the company to start realizing in the coming quarters or years?
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Jailendra, it's good to hear your voice. We are -- we did not include any assumptions that relate to the Google or Cleveland Clinic relationship in our model. It was too early and too less specific in order to do that. However, that is not to say that we don't accept some pretty wonderful things coming down the pipe from those relationships.
And as I mentioned earlier, you can -- you're welcome to join our client forum in April to begin to see it with your own eyes. The -- long term, Converge is related to some of the strategic relationships that you've mentioned. Converge, like any one of our platform, is one code base. That's fairly unique.
There is nothing like it in the market, where the same platform is serving payers, providers, integrating with devices, with consumer-facing structures and other things. It's designed to do transactional and longitudinal and support hybrid care, people that you see in person and online. It's deeply integrated, which is very hard for large companies to do, with a long list of assets, including many, many electronic health records and other platforms. And very importantly, and related to your question, it is open.
So most platforms, especially telehealth platform, are close based. Whatever you see is what the vendor has built. We are a platform also in the sense that you can see the Converge is opening up to third parties. It allows our clients and partners to also offer their innovations on our platform.
And that's enormously helpful because it offers a much bigger array of use cases, much more diversity and much more flexibility for our clients and partners. The Converge is modular. So it really allows you to build and pay for what you need today, getting very comfortable that it will be there for you in the future. And the future is going to be fairly sizable in the sense of speed and enormity of change that we believe we are going to experience.
So it's a platform that is designed to truly offer a comprehensive array of capabilities. But at the same time, it's incredibly simple. It's simple in the way that it's run in a contact-sensitive way. You only see what you need at the time that you see it and the user experience is truly unique.
It's global-ready, it's scalable, and it's incredibly efficient in way of hosting costs and other ways, and that's also very, very important when we look into the future and the numbers that can -- we can see going forward.
Keith Anderson -- Chief Financial Officer
I guess to go more specifically into the model, Jailendra, we're cautious. That's only our second quarter as a public company. So until those relationships put points on the board beyond what they're currently doing, we're not going to put them in the model, the guidance or the forecast. So our relationship with Cleveland Clinic is fantastic.
We are generating revenue both from Cleveland Clinic, as well as from the JV. What they were doing in Q4, yes, we have that in the model. So we're waiting for points to be put on the board before we're comfortable putting them in the forward guidance, as well as some of the efficiencies that we're realizing from the partnership with Google. There was some of that dynamic and aspect in Q4 that is in the model.
It is happening. I can touch it, and so then it made it into our guidance. We're just conservative in terms of, OK, there's a lot of opportunities. The Google partnership gets me, as the CFO, very excited in terms of the operational efficiencies and then the whole executive team in terms of the opportunities globally.
But we don't have those in the model yet because I need to see some points put on the board before they make it into our forecast.
Jailendra Singh -- Credit Suisse -- Analyst
All right. Great. Thanks, guys.
Operator
Your next question comes from the line of Charles Rhyee with Cowen. Your line is open.
Charles Rhyee -- Cowen and Company -- Analyst
Yes. Thanks for taking the question. Maybe I can ask this question about -- you're talking, Keith, the visits this year is kind of a new base level, and this is where you expect to grow off of. And you guys were talking about the shift to specialist care being greater than 50% of visits in the past year.
Does this change or affect how you recruit providers for the AMG network? And maybe following up to someone else's question regarding M&A. Is this an area where you could deploy capital to help expand this quicker? Or is that not necessarily where you would be looking to use the balance sheet? Thanks.
Keith Anderson -- Chief Financial Officer
There's a lot of interest -- it's a great question. On the M&A side, there's a lot of interesting models out there using providers more efficiently. And so that is far and away our biggest area of cost. That is one that through different technologies, different processes, yes, we can become more efficient.
That is one that gets me excited. A lot gets me excited, I guess, but that one, especially. In terms of the mix shift. It was around half in 2020 were specialists.
We see that continuing into 2021 as more of the straight up urgent care has shifted to the health plan's own providers delivering care in the health systems, your own doctor delivering care to you. We see that continuing. We saw it in Q4. That is driving up the revenue or the price per visit to the $80 range from $54 and $74 in 2020.
In terms of recruiting, it's -- the pandemic has really -- and Ido said this in his prepared remarks. OBs, cardiologists, those specialists have now embraced delivering care to their specific patients. So if they're doing it, those specialists delivering care to their patients, it's natural for them to want to supplement their practice with plugging into our platform and delivering care. So from a -- part of the reason why we bought Aligned in 2019 is there's a psychiatric shortage out there, and the need is going the other direction.
So for our health system customers, we wanted to make sure that we had the right team on the field to be able to support their unmet need. But for the overall AMG providers on the platform, yes, we are seeing more of a shift to the specialists. Ido, if you want to take the overall aspects of AMG, but within the model, that is what we're seeing in Q4 and what we are forecasting that continuation throughout 2021.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Charles, thank you for the great questions. So as you know, we see AMG as a buffer, as a service to our client and not as a replacement to their own services. We also try to enable not only acute care but the full spectrum. So if you think about it, the incredible growth of client active provider that we experienced in 2020 and we expect to continue and grow rapidly into the future, is mostly in 2,000-plus medical centers, most of them are academic, most of them are specialists.
Of course, in order to envelope a specialist, it is infinitely more complicated than to have an acute care visit with a video online and provide it for [Inaudible]. We have different level of integration. The rules are much more complicated with multidisciplinary care that is required and so on and so forth. So our role is to increase -- improve financial and clinical outcomes.
When you think about financial clinical outcomes, you're mostly talking about the impact of chronic care and specialists that is enabled by our platform. As we try to get better supporting those specialists, sometimes, like in the case of the line, we grow AMG as a giant sandbox that also serves as a buffer for our clients. And as we figure out and streamline the workflow for AMG, we immediately make this information available in those technologies and services available to our ecosystem with the overarching goal to allow them to be as successful as they can with their own resources and not necessarily with AMG.
Charles Rhyee -- Cowen and Company -- Analyst
Great. Thank you.
Operator
Your next question comes from the line of Ravi Misra with Berenberg Capital Markets. Your line is open.
Ravi Misra -- Berenberg Capital Markets -- Analyst
Hi. Thank you for taking the question. So just maybe a little bit of an extension of that visit mix shift to -- in AMG and specialty. I'm just curious, how sustainable do you think that is? I mean if your kind of institutional partners are kind of shifting more of their visits to urgent care.
Or do you think, over time, they're also going to be moving the specialty care, given that revenue shift. And does that put your AMG profile and mix there -- at risk there? And maybe my second question is just around the investments, Keith, next year, it looks like you're guiding above consensus on a sales level, but you're also kind of investing a little bit more. Is that entirely R&D with Converge that's just pulled forward out of future years? Or should we think of this as the new normal in terms of the incremental spend going through the model in the out years? Thanks.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Keith, I think you're on mute. I know you're talking.
Keith Anderson -- Chief Financial Officer
Thanks, Ido. The second question is the easiest. The answer is yes. It is R&D confined to 2021.
That line goes back to a more normalized level in 2022. G&A goes down to what typically you're seeing with us and our competitors in terms of percentage of revenue and same with sales and marketing. So that question -- let's answer that one first. In terms of the second one, in terms of visit volumes, we -- where the specialist visits are actually more attractive in terms of what our providers want, our health system and health plan customers want, I mean the goal is, again, going back to the mission statement of the business, to have your doctor deliver care to you or your health plan coordinate the care and have, in most cases, that plan doctor deliver care to you.
So where the specialists are really supplementing care, the urgent care, yes, we're going to have those doctors ready to go in and provide the backup care when needed. But if all the doctors of the doctor group, cardiologists, OBs, endocrinologists, all of them are there providing the care. And then if they can't, we need to have those specialists in the warehouse ready to provide the care so that there's not any gaps or any delays. So we're seeing this shift continue into 2021.
You're seeing the price per visit or the revenue per visit continue nicely from $54.19 to $74 in 2020 to $80 range in 2021. That dynamic is already happening in Q4. So we don't report on a quarterly basis, price per visit, it's already happening. So this shift is intentional.
The shift is strategic, and it's the ultimate realization of Ido and Roy's vision in terms of providing backup care, not competing against the providers of care. We are a technology company. So we see that business, that revenue shifting up into the subscription line, and it's already happening. So Ido, I don't know if you have anything you want to follow up.
But that is the dynamics within the model that I think you were getting at.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
So Ravi, I would state it maybe in another way. We are a technology company, but we complement the offering with services to provide a complete offering to our clients. So back in the days when we build the infrastructure, it became very apparent that without having a national network of providers, starting with acute care and then to other disciplines, no one can operate our technology. You have to have that.
And it took enormous effort to create it, and it's still very valuable in way of this buffer. The next frontier after acute care and primary care is specialty care. It's very hard to organize psychiatrists, psychologists and different type of other specialists. On the one hand, we are really enabling our customers to do that, and they're doing it a lot on our platform.
But on the other hand, sometimes in order to pave the way, we also organized those services as a complete solution and use that as an add-on. And the line -- the example is a good one where we found that if you can be in a psychiatry, it will really be the emergency room, it can really help these patients earlier and provide some value. So this complementary buffer has moved from primary care into specialty care. Our intent is not to build the largest hospital in the cloud or specialists.
That will not make sense. Our role is to connect more specialists to the ecosystem through our platform, but we will create more and more examples potentially with some house programs that we're going to offer to our customers because they need it, and not everybody is able to do it themselves and because this is the best way to truly streamline our technology.
Ravi Misra -- Berenberg Capital Markets -- Analyst
Great. Thank you. And then maybe just one more on Converge. Looking forward to kind of seeing more detail on that at the upcoming event.
But just how do you think about that from your kind of land and expand or this kind of ACV upsell strategy? Is it something that kind of enables you to just easily implement more modules per customer? Or is there something else? Can you just provide a little bit more color on the business model around that? Thank you.
Keith Anderson -- Chief Financial Officer
Yeah, Ravi. Let's speak about that on April 28. That's -- we've got a whole day planned on it. We're going to have customers.
Let's kick that on the 28th.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
But the short answer is yes.
Operator
Your next question comes from the line of David Larsen with BTIG. Your line is open.
David Larsen -- BTIG -- Analyst
Hi. Congratulations on a good quarter. Can you talk a little bit about Amazon's announcement to push more services across the U.S. in their healthcare area, especially with telehealth? And one of the plans we talked to said that what's intriguing about this is that Amazon, in some cases or in some cities, may have a nurse that can show up at the patient's home the next morning at 9 a.m.
if they had a telehealth visit at 2 a.m. that same night and that nurse could bring medications with them. And then at the home, like there are different devices that could potentially be used like a stethoscope, things for respiratory, measuring, respiratory breathing habits and also like lab services that can be delivered at the home. Any thoughts around that? And do you have any potential plans to get into more of like this home health arena in a digitized way? Thanks.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
So again, this is in some ways, David, two questions. We're not going to opine about what Amazon is doing. I would just say welcome to the swamp. It's much more complicated than you think.
And we encourage the additional availability of convenient primary care. You cannot have enough of this. Amazon brings enormous amount of assets in way of drug delivery, in a way of consumer experience and things of that nature, and it relates to primary care in certain models, that could be a fantastic thing, which is very, very different from the role of Amwell. We always talked about the fact that care is moving into the home, and you need a very deep degree of integration with devices, better analytics, new care plans, better integration with multidisciplinary team, deep understanding of the clinical flows and the financial flows and so on and so forth.
It's very hard. We spent a decade and a half building it. It's not the DNA of big tech. And big tech did not have a track record of doing that in world technology.
In addition to that, the relationships in the ecosystem are not as easy as they are for us. We really did that for many years. We are trusted by the parties. Amazon may be less so in some ways.
So we think that what they bring to certain employers could be very helpful, and yet does not compete directly with most of the value proposition that we offer at this time. When you come to see Converge, you'll realize the enormity of complexity that you need to truly serve complicated patients with multiple existing relationships and financial arrangements and regulations in their most convenient location, which is their home. We certainly totally agree with that notion. We just think it's really, really hard to create a solution.
And very importantly, no one company can do that. That is, in our opinion, impossible. You need a very big coalition that is tightly integrated to reach that outcome.
Operator
Your next question comes from the line of Eric Percher with Nephron Research. Your line is open.
Eric Percher -- Nephron Research -- Analyst
Thank you. A non-Converge health system question. You noted the delayed pandemic impact on subscription. And we're at a point where health systems must now move from temporary to industrialized solutions.
So what is your view on the time line? Has the health system sales cycle contracted? And maybe what is the competitive environment?
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
So it was really interesting to see the dynamics in 2020. People were caught completely by surprise by the pandemic in the sense that telehealth was 1% of the visits at the beginning of '20. We tend to forget that. 1% of the visits were done virtually in January of 2020.
And then it went up to 50%, and now it's 15% to 20%. So these are amazing numbers. And what happened at the beginning is that people used whatever they know. They used Facetime, they used Zoom.
There's lots of product, and that was very, very helpful because it was very familiar, both to the patient and the doctor, but there are enormous list of shortcomings that became very apparent to people very, very quickly. So well into the year, the dialogue changed and people realized that the level of specification that is required for digital connectivity is much, much bigger than any of the tools that they had, and that was very opportunistic and very helpful to us. I don't know any leader of any delivery network that is not thinking now about digital health connectivity infrastructure. Some are ready to do it sooner than others, but it's not an optional thing.
It's just as important as your EMR in many ways, maybe even more important, in order to survive into the future. So the urgency is there. The clarity of what they want to buy is there as well. The ability to implement the speed do vary.
But we believe that in the next few years, I don't see any practice or any provider that is unable to effectively, in a fully integrated way, interact with their patients, both online and in person through a hybrid model. That probably spells bad news to anyone that has the model of docking the box in the cloud that is competing with that preferred option.
Keith Anderson -- Chief Financial Officer
Eric, I mean, from my perspective, when I look at the individual business lines, product lines, they're being a lot more thoughtful. Coming out of the pandemic, their doctors are asking for this. And as we discussed on the Q3 call, we're seeing happen even more. They're using it as a patient recruiting tool.
So if you go to the products that Ido mentioned on his prepared remarks, the C500 Carepoints can be used both in the hospital and in the home. The Amwell Hospital TV, same thing. So I mean what they're trying to do or what their part of their plan is, a, patient recruiting. They want to bring more of their doctors on the peripheral into the mainstream, delivering care through the hospital system.
That's the Amwell Now product. But they're also trying to expand their footprint into the community with the C500 cart, with the hospital TV. So the conversations we're having with them, they're asking for this functionality. They're asking, do you have this capability? And it's very, very differentiating.
So I would say versus COVID, when it was more emergency-based, OK, how quickly can we get your COVID module and how many C500 carts or any carts can we get to man our satellite emergency rooms, now they're being very, very thoughtful. Do you have this functionality? How quickly can we bring these doctors on the peripheral into the mainstream? So we're really excited about how differentiated our value proposition is for the hospital system customers and part of the Converge build-out.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
I would just very quickly add one more thing. What's really interesting is that finally, after a decade and a half, people realize the power of connectivity. For the first time in a really long time, many of our customers tell us, so how can we, providers, connect with payers? And payers say to us and say, how can we enable our provider network to be included in our best in care in our vision? And that's very refreshing. And that's a zone where we are extremely comfortable in and have very strong advantage.
Operator
Your next question comes from the line of David Grossman with Stifel. Your line is open.
David Grossman -- Stifel Financial Corp. -- Analyst
Thank you. So you guys have done a great job of covering all the big points here. So I'm just going to limit it to two quick financial questions. Keith, perhaps you could share with us what the fully diluted share count is if -- once you start making money, at least based on the options and shares that are out there.
And then the second quick one would be, sorry if I missed this, but can you tell us or help us understand how much of the average revenue per health system increase was number of modules versus utilization or any other factors that may impacted that?
Keith Anderson -- Chief Financial Officer
So I'll come back to you on the fully diluted because I normally quote that on a treasury stock method. And so I'll call you up and give you that one. But in terms of where the mix is coming from on the systems, like I said, the name of the game there is land and expand. So I mean you can see how the average contract value expanded nicely.
That is being driven both by the logos and by the expansion of the contract value. So what's keeping the contract value down is the number -- the denominator that is being added at a very good pace. So we're seeing our typical customer. I know we gave some quotes of what the typical contract looks like.
We have some of the larger health systems really getting up there in many, many millions in terms of total contract value.
David Grossman -- Stifel Financial Corp. -- Analyst
Right. So is there any stat you can share in terms of number of modules and how that's increasing on average or anything like that per client, independent of the kind of growth in the denominator, if you will?
Keith Anderson -- Chief Financial Officer
Yeah. We haven't disclosed that. We -- during the IPO, we listed all of the modules that we have. I would just say what we disclosed during the IPO and in the S-1.
Operator
There are no further questions at this time. I will turn the call back over to Dr. Ido Schoenberg.
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Thank you so much. I want to thank everyone for joining. Many of you are dear friends and follow us for many, many years. I really appreciate the time and effort that you are making.
Together, we are helping bring care to millions of people, and that's very important. So we look forward to continue the dialogue in person very soon.
Operator
[Operator signoff]
Duration: 79 minutes
Call participants:
Ido Schoenberg -- Chairman and Co-Chief Executive Officer
Keith Anderson -- Chief Financial Officer
Ricky Goldwasser -- Morgan Stanley -- Analyst
Robert Jones -- Goldman Sachs -- Analyst
Sean Wieland -- Piper Sandler -- Analyst
Kevin Caliendo -- UBS -- Analyst
Jailendra Singh -- Credit Suisse -- Analyst
Charles Rhyee -- Cowen and Company -- Analyst
Ravi Misra -- Berenberg Capital Markets -- Analyst
David Larsen -- BTIG -- Analyst
Eric Percher -- Nephron Research -- Analyst
David Grossman -- Stifel Financial Corp. -- Analyst