Image source: The Motley Fool.
Oscar Health, Inc. (OSCR 4.22%)
Q4 2021 Earnings Call
Feb 10, 2022, 5:00 p.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Good afternoon. My name is Rachel, and I will be your conference operator today. At this time, I would like to welcome everyone to Oscar Health's 2021 fourth quarter and full year earnings conference call. [Operator instructions] I would now like to turn it over to Cornelia Miller, vice president of corporate development and investor relations, to begin the conference.
Ma'am, please go ahead.
Cornelia Miller -- Vice President of Corporate Development and Investor Relations
Thank you, Rachel, and good afternoon, everyone. Thank you for joining us for our fourth quarter and year-end earnings call, where we'll discuss our financial results, the benefits of our increasing scale and reaffirm our 2022 outlook. Mario Schlosser, Oscar's co-founder and chief executive officer; and Scott Blackley, Oscar's chief financial officer, will host this afternoon's call, which can also be accessed through our investor relations website at ir.hioscar.com. Full details of our results and additional management commentary are available in our earnings release, which can be found on our investor relations website at ir.hioscar.com.
Any remarks that Oscar makes about the future constitute forward-looking statements within the meaning of the safe harbor provision under the Private Securities Litigation Reform Act of 1995. Actual results may differ materially from those indicated by those forward-looking statements as a result of various important factors, including those discussed in our quarterly report on Form 10-Q for the quarterly period ended September 30, 2021, filed with the SEC and our other filings with the SEC. Such forward-looking statements are based on current expectations as of today. Oscar anticipates that subsequent events and developments may cause estimates to change.
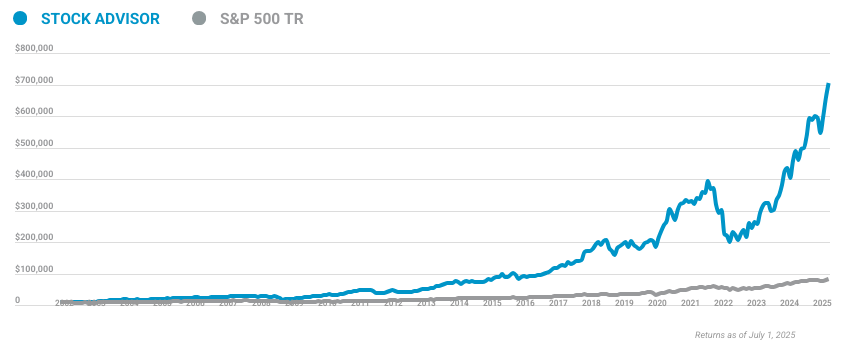
10 stocks we like better than Oscar Health, Inc.
When our award-winning analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Oscar Health, Inc. wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of January 20, 2022
While the company may elect to update these forward-looking statements at some point in the future, we specifically disclaim any obligation to do so. The call will also refer to certain non-GAAP measures. A reconciliation of these measures to the most directly comparable GAAP measures can be found in our fourth quarter 2021 press release, which is available on the company's Investor Relations website at ir.hioscar.com. With that, I would like to turn the call over to our CEO, Mario Schlosser.
Mario Schlosser -- Co-Founder and Chief Executive Officer
Good evening, everyone, and thank you for joining us. We have created something unique here at Oscar. We entered 2022 with strong tailwinds in our business and a clear strategy set for the years ahead. Building on our record-breaking growth, we remain focused on scaling operations and driving toward profitability.
We are leveraging the technology we have built to reduce medical costs to provide better clinical outcomes for our members and to reduce our operating expenses. The healthcare system is changing toward consumerization toward risk-sharing and toward increased disruption by technology, and we believe we are delivering on a unique set of business proof points to capitalize on the shifts. And we are well-positioned to deliver on our vision of making healthcare more accessible and more affordable for all. We are doing this through both our risk-based business and our +Oscar client relationships.
As you would recall, we shared some preliminary Q4 2021 results, as well as 2022 guidance on January 27. We will dig deeper into those metrics now. To start, Scott is going to take you through our Q4 and full year 2021 financials, and then I will come back and highlight the key themes for Oscar in 2022. With that, I would like to turn the call over to Scott.
Scott Blackley -- Chief Financial Officer
Thank you, Mario, and good afternoon, everyone. Today, I'm going to walk through in more detail the 2021 results, and I'll reaffirm our 2022 guidance. Before I jump into the numbers, I'll call out three key themes that are emerging in our results. We are seeing strong traction, gaining new members and retaining the majority of our existing ones.
We have made great progress on efficiency with our higher scale, and there is room for more progress. And lastly, we see opportunities for MLR improvement. Turning to the results. We had a number of onetime items in 2020 that impacted our year-over-year results, the largest of which was a $52 million net risk corridor settlement, which was recognized in the fourth quarter of 2020.
We excluded this nonrecurring item from all of our 2020 key results, including adjusted EBITDA. Moving to membership. We ended the year with approximately 598,000 members, an increase of 49% year over year, driven by growth in our individual C + O and Medicare Advantage books of business. Membership growth continued to exceed our expectations throughout the year as consumers continue to select Oscar's plans throughout the special enrollment window.
Powering our growth, we retained more than 80% of our year-end individual members in 2022. Fourth quarter direct and assumed policy premiums increased 59% year over year to $873 million, driven by higher membership, as well as business mix shifts toward higher premium Silver plans and modest rate increases. For the full year, direct and assumed policy premiums increased 50% year over year to $3.4 billion, largely driven by the same factors. This represents more than 70% annual top line growth over the past four years.
Our enhanced scale drove a fit -- drove greater efficiencies across our businesses in 2021. Specifically, our Q4 2021 insurance company administrative ratio was 24.5%, an improvement of 12 points year over year, and our full year InsureCo administrative ratio improved 430 basis points year over year to 21.8%. Fixed cost leverage, variable cost efficiencies and the elimination of the health insurance fee -- health insurer fee in 2021 drove the ratio lower year over year. Scale benefits also positively impacted our newest metric, our adjusted administrative expense ratio, which was 34.4% in the quarter and 28.9% for the full year.
The full year metric improved by 560 basis points. Turning to medical costs. Our medical loss ratio was 97.9% in the quarter, down 10 points from the fourth quarter of 2020. We recognized $35 million of favorable development in the fourth quarter of '21, driven by lower-than-expected utilization in the third quarter of '21 and some positive prior year development.
The full year MLR of 88.9% was at the low end of our guidance as utilization came in as expected, and we benefited from the favorable development. Compared to 2020, MLR increased 420 basis points year over year, largely due to higher net COVID costs and higher SEP growth in 2021, which was partially offset by favorable development. Let me spend a moment on COVID. Overall, net COVID costs were in line with our expectations in the fourth quarter of '21.
We continue to see direct COVID costs being partly offset by lower non-COVID utilization. Our overall combined ratio, which is the sum of our medical loss ratio and the insurance company administrative expense ratio was 122.4% in the quarter and 110.7% for the full year. The full year '21 combined ratio was essentially flat on a year-over-year basis as improvements in administrative efficiencies were offset by higher net COVID costs in the MLR. Our fourth quarter '21 adjusted EBITDA loss of $164 million, was $52 million better year over year.
And for 2021, it was $430 million, an increase of $27 million year over year. In addition to the drivers impacting the MLR and the administrative ratios year over year, we had a release of premium deficiency reserves in 2021 versus an increase in 2020. Turning to the balance sheet. We ended the quarter with over $2.5 billion in total company cash and investments, including roughly $740 million of cash and investments at the parent and another $1.8 billion of cash and investments at our insurance subsidiaries.
The new funding of $305 million that we announced two weeks ago provides us with strong balance sheet resilience as we start the year. We are also reiterating our 2022 guidance, which reflects the increased scale of the business and builds on the momentum we saw last year. This includes an expectation for more than 80% growth at the midpoint in our direct and assumed policy premiums to $6.1 billion to $6.4 billion, as well as 400 basis points of improvement at the midpoint in our MLR to 84% to 86%. I'd note that our MLR guidance assumes non-COVID utilization returns to baseline levels this year.
We have had a strong track record of delivering high growth while still driving MLR improvement. Our direct policy premiums increased 70% on average annually over the past four years. And during that period, we decreased our MLR roughly 8 points. Excluding COVID, our MLR decreased 13 points since 2017 as we effectively absorbed higher membership while reducing medical costs.
We're also seeing a step change in our +Oscar business results as we are expecting $65 million to $70 million of fee-based revenue in 2022. Our positive top line momentum and increased scale continues to drive meaningful progress on our administrative expense ratios. Our adjusted administrative expense ratio has declined roughly 500 basis points over the past two years, and we're expecting another 300 basis points of improvement in 2022. Importantly, the majority of these costs are in our control.
All told, for 2022, we are expecting an adjusted EBITDA loss between $380 million and $480 million, which at the midpoint is roughly consistent with 2021 on an absolute basis. On a relative basis, this is roughly half of that of 2021, measured as a percentage of premiums before ceded reinsurance. Our larger scale is a tailwind for reaching our 2023 profitability target for the insurance company. We look forward to discussing this in more detail at our March 25 Investor Day.
And with that, let me turn the call over to Mario.
Mario Schlosser -- Co-Founder and Chief Executive Officer
Thank you, Scott. I want to close with a summary of why Oscar is position for success in 2022 and beyond. I firmly believe that Oscar is the vanguard for the new way healthcare will be delivered in the U.S. We feel that we have found a model that works in consumer-driven markets that are best served with deep provider partnerships and with a frictionless experience.
And we see clear signs that more of the U.S. healthcare system will move further in this direction in the future. The ACA markets has been a proving ground for the value of this frictionless experience in healthcare. And our innovative approach, which couples our full-stack technology with industry-leading member engagements resulted in a powerful open roaming season where we saw monumental growth and record high retention rates.
To the point we are today, approximately one in 15 ACA members are now served by Oscar. And the value of the experience we deliver is also evident in our retention with just above 80% of our IFP members, 85% of the groups in C + O with 90% in our latest co-branded +Oscar Medicare Advantage plan staying with us year over year. Our fourth quarter 2021 Net Promoter Score reached 42, and remains meaningfully higher than the industry average of three. So as we see it, our results in growth to more than 1 million members is driven by our strong brands by our member experience and by our innovation in plant design and product offerings.
I'll just give you a couple of examples for these product offerings. We now have 40% of our members on a plan, offering our virtual primary care, which has made the Oscar Medical Group the No. 1 or No. 2 primary care group in every market where it is available.
We also recently updated our costs made too well, which can price claims in real time and empowers the member with control and choice when it comes to their care decisions. It's these kind of offerings that enable us to price to achieve growth and improve margins for 2022, where we, in fact, increased our premium rates at the overall book level. In this past of enrollment period, so for 2022, only 16% of all of our new initiations came from markets where we had the lowest price plan offering. And if you look at where membership is now, only 13% of our total individual membership is in markets where Oscar is the lowest price offering.
Now we're also successfully bringing our unique model to +Oscar clients. And the platform we have is delivering clear business results for them. Take C + O, for example, we pointed the platform in a different market segments, small group segments. And in one year, we have had nine times growth to now more than 30,000 members, actually doubling from the year-end number of 16,500 members.
Hence, our broker NPS score in the small business segment is 66, which highlights the value our other stakeholders find in our frictionless technology. We continue to build out this kind of +Oscar business. And we expect, as Scott said, +Oscar generates $65 million to $70 million of revenue in 2022. Our platform has key applications across the healthcare system.
For example, one of our clients realized administrative savings of 20% by leveraging +Oscar. We are encouraged by our negotiations with prospective clients and look forward to sharing more details on this during the upcoming Investor Day. Now to me, the best illustration of our path forward is the following. When we look across all of our markets, we generally see that the lower the medical loss ratio, the higher the Net Promoter Score.
In my view, there couldn't be a better illustration of where a more consumerized healthcare system is going and of how Oscar is going to deliver on our mission of making healthcare accessible and affordable. Because that mission motivates us to deliver our business model of consumerizing healthcare profitably. Our growth today provides scale and operating leverage that we will harness to drive improved efficiency in our administrative cost and medical loss ratio. A good early sign, by the way, is that despite our nearly two times membership growth, we have swiftly met the demands of our new members and have seen higher member satisfaction scores year over year.
That said, we still have plenty of ways to operate more efficiently and to leverage our provider and member engagement initiatives to reduce healthcare costs, and that's what we are focused on. In many ways, we are still a young company with meaningful improvement opportunities ahead. To that end, over the last several years, we have added experienced healthcare executives to our bench, including most recently, former chief legal officer at Everside Health and career law and health executive Ranmali Bopitiya as EVP and chief legal officer; and former Aetna CEO, Mark Bertolini as strategic advisor. Before I close, I want to reiterate our strategic priorities for 2022 and 2023.
First, we will continue to drive meaningful growth across our business, both for the insurance company and for +Oscar. Second, we continue to target profitability for insurance company in 2023, and we are committed to becoming profitable at the overall company level over time as our businesses are reaching scale and we gain more efficiencies from our technology. Now finally, I want to thank the Oscar team for working so tirelessly during our first year as a public company to serve our members and work toward our mission of making a healthier life affordable and accessible for all. As we say here at Oscar, we're powered by our people, and I continue to be inspired by the creativity, the tenacity and the dedication, Oscar team member show every day.
I'm very, very proud of what we can accomplish when we come together as a team. With that, I'll turn the call over to the operator for questions.
Questions & Answers:
Operator
Thank you. [Operator instructions] Your first question comes from the line of Ricky Goldwasser with Morgan Stanley. Sir, your line is open.
Ricky Goldwasser -- Morgan Stanley -- Analyst
Yeah. Hi. Good afternoon, Mario and Scott. So my question is on the exchange enrollment that you've seen.
I mean, clearly, phenomenal results significantly surpassed your expectations on [Inaudible]. Can you just give us some color on sort of any contribution that you had from marketing or sales channels and how that helped you sort of achieve this milestone growth? And then also, as we look ahead to 2023, do you expect to see continued scaling? Or do you believe that now you have the scale that you need? And from now on, you're going to focus on that kind of like margin expansion and MLR improvement opportunity?
Mario Schlosser -- Co-Founder and Chief Executive Officer
Yeah. Ricky, great questions. Let me hit on both, and then have Scott comment on the second question here as well. So in terms of channels that members come through, I think we see a couple of different things.
Generally, we grow in markets where we've got kind of the perfect mix of product design, being right, networks being built well and deep provider partnerships, and ideally word of mouth and brand as well. So that's where it works best. Now the other piece to this is the distribution as well. We have worked quite a bit with the broker channel in particular.
And I mentioned earlier the NPS the brokers have when they work with us in our small group business, for example, because we're able to deliver fast turnaround times there. We're able to help them deliver frictionless to their members when they enroll. And that also helps us grow in these markets, it will be all of the market segments. So that's really been -- that's been where the focus has been.
But you really can't take any of these elements out of the equation, I would say. It's going to be the mix of products, network, brands and distribution and that then works best. Now in terms of where we are as a company and what our focus will be, I really want to reaffirm these two [Inaudible] we have for 2022. One is continue the growth in insurance company and +Oscar.
And we think we have a lot of runway ahead of us there. We're only in half the markets in the -- for the cap markets right now. And we're only in eight states for the C + O products. And we have a ton of more runway ahead of us in delivering MA growth to +Oscar partnerships as well.
And so we're going to keep doing that. However, we have a great focus on making sure we target profitability insurance company next year. And as I said, profitability in the overall company over time, truly as well. And then that is where, right now, a lot of our internal focus really is going with both MLR improvements, administrative efficiency improvements as well.
Scott, do you want to add more?
Scott Blackley -- Chief Financial Officer
No, Ricky. I think that on that point, we'll be sharing more information about future plans at our Investor Day in March, so I won't jump out of that.
Ricky Goldwasser -- Morgan Stanley -- Analyst
OK. And as a follow-up, if you think about +Oscar, Mario, you talk to the pipeline and the negotiations that you're having. Can you maybe a little bit talk about what's sort of the profile of the companies in the +Oscar pipeline?
Mario Schlosser -- Co-Founder and Chief Executive Officer
Yeah. And it really is the kind of three major segments we've talked about before, which is health systems who want to add more risk and go deep into the risk markets where we've seen quite a bit more people pick up their heads even just in the last 12 months. The second segment is -- and we have several of those examples in the pipeline right now. The second segment is health systems already have a plan, already in the risk business in this example.
So that's in the pipeline as well. And the third segment is sort of midsized insurance companies who are realizing that, as I said in my prepared remarks here, the healthcare system is inevitably going to -- it demands more frictionless provider experience and where we can really help both take the cost out and enable them to put more innovative plan designs out there. And so all three of these are in the pipeline right now, and we're excited about both where that will go in the next couple of years. And how we concern this increasing from a business process as a service model toward a Software-as-a-Service model as well and also where we are for this year.
Operator
Thank you. The next question comes from the line of Kevin Fischbeck with Bank of America. Your line is open.
Adam Ron -- Bank of America Merrill Lynch -- Analyst
Hey, thanks for the question. This is Adam Ron on for Kevin. We were a little surprise by the fact that you were getting more SG&A leverage. I know we talked about this last time with the 2022 guidance, given that you grew revenue and membership at such a rapid pace.
And so from here, would you expect most of the cost leverage that you're underwriting going forward to come from higher revenue on the same SG&A base? Or is there actually a chance that, on a dollar basis, it could actually decline?
Scott Blackley -- Chief Financial Officer
Yeah. Adam, thanks for the question. So I'll start off by saying that I think that our greater scale that we're seeing in 2022 is going to help us to achieve better cost leverage on our fixed cost and our variable cost going forward. We can negotiate better costs with vendors.
We have an opportunity to continue to optimize our operations and the opportunity for even further fixed cost leverage as we head into next year. So we certainly see opportunities on the cost side beyond just what's available from increasing revenues into the future.
Adam Ron -- Bank of America Merrill Lynch -- Analyst
All right. Great. And then on 2023, if exchange subsidies were to end up expiring, do you think the overall marketplace would shrink? And would you be able to grow in that environment? And if not, would that hurt your ability to drive that SG&A leverage and ultimately achieve InsureCo profitability? And also in that scenario? Or are there any offsets like potentially lower membership, meaning better MLR?
Mario Schlosser -- Co-Founder and Chief Executive Officer
Yeah, Adam, I'd say a couple of thoughts on this one. One is, we now have several different business lines that are growing, C + O, +Oscar deals and so on. So I do think we are diversifying ourselves in a sense there, that helps. The second point, though, is that if you're looking for a company that has -- maybe has the highest volatility of regulatory environment, it might just be us over the last two years.
I mean we have lifted in so many cycles of ACA on, ACA off. I can't even count them anymore. What we have generally believed, and I think it's proven to be true is that benefits like now ensuring 50 million-plus people is very, very unlikely to get the clock turned back on. And so in some shape or form, I would very strongly believe that these subsidies will remain in place or will be replaced by similar subsidies under different name, perhaps, and that's sort of like generally what we are assuming there.
However, we have also lived through cycles, plenty of them where Silver loading happens and some CSR subsidies were repeated and things like that. And we have fought through them and its always improved throughout these cycles, which makes me very confident that if somehow we have to deal with some upheaval there, we certainly could. And actually, the final point there is that we've been building our platform internally partly because we want to be able to react quickly. If there is a regulatory change, like, for example, more testing reimbursements that we can flip a couple of switches and very quickly react to it and thrive through it really.
And I think that's the same applies here. If there's new regulation, we'll adapt to it quickly. The kind of inevitable march of the healthcare system toward more consumerization, I don't think will be stopped by any of what might come our way there.
Scott Blackley -- Chief Financial Officer
Just to pile on to your questions about efficiency and scale. I would just say this. So one, we continue to think that the company is built to be able to grow. But regardless of what we see on the growth side, we still think that there are opportunities to create additional leverage in our model so that means that we see opportunities of improving both fixed cost, as well as variable costs.
And at the scale that we're seeing at '22, I'm anticipating that we will be able to, as I mentioned in another question, I am expecting that we're going to be able to drive down vendor costs that we are going to be able to continue to optimize our operations against that larger base. And that is going to -- even with -- in '22, we're starting to see significant fixed cost leverage, and I would anticipate that we're going to be able to continue to deliver that.
Adam Ron -- Bank of America Merrill Lynch -- Analyst
Great. Thanks.
Operator
Your next question comes from the line of Stephen Baxter with Wells Fargo. Your line is open.
Stephen Baxter -- Wells Fargo Securities -- Analyst
Yeah. Hi, thank you. Can you talk a little bit about how your breakout of metal tiers for the exchanges is kind of shaping up? I'd love to hear if you have a reminder on where you ended up for 2021 in terms of your Bronze and your Silver mix and then how that is shaping up for 2022? Any specifics there would be very helpful. And I would also like to hear a little bit more about how you're thinking about your risk adjustment position as you move from 2021 to 2022? And how that's impacted by any of your product mix changes or just how you guys are thinking about it? Thanks.
Mario Schlosser -- Co-Founder and Chief Executive Officer
Yeah. Steve, let me start with the metal tier mix. And then Scott, you can talk a bit about risk adjustments. We talked about this in the IPO and even before that, but we were off the market average for quite some time with a higher book of Bronze membership, lower PMPM, therefore, a higher reserve and payout, as well as the results.
And part of our march toward profitability has been to return the dial toward higher PMPM membership than actually more clinically ill members as well and older members and more of a membership. And I think we've done this really very successfully. If you trace just the last three OEs, we went through 37% Silver in OE '20 to 50% Silver in OE '21 to now 65% Silver in OE '22. So you had a very nice shift every to what these higher PMPM Silver plans.
That's, again, a mix of the same kind of factors I gave with you earlier, which is work with the distribution at different plan designs and branding will be put into these plans and so on. So that's been a really important shift there for us. You see this also continuously in the numbers that the PMPM revenue always goes up. So revenue grows faster than the membership count there.
And we're going to continue to pursue that in that same way. Now we also constantly change our plan designs in other tiers, and are very confident there that those planned designs can also deliver value, and -- so we'll focus there as well. So Scott, you can maybe talk about [Inaudible] --
Scott Blackley -- Chief Financial Officer
Yeah. And in terms of the risk adjustment, we've seen strong performance in that line item. We've had primarily positive adjustments on an ongoing basis. And I would just say in terms of RA as a percentage of direct and assumed premiums I would expect that with the changing mix toward more Silver, we'll see slightly improved RA as a percentage of that.
And I would expect to see -- we saw some of that in '21, we'd expect to see further improvement in '22.
Stephen Baxter -- Wells Fargo Securities -- Analyst
Got it, thanks. And then just as a quick follow-up or a second question. Just the fee-based revenue you're expecting in 2022, just any insight into how that's expected to ramp up through the year. Is it expected to be a more even contribution as we think about the contribution margin against an incremental revenue, I guess how should we be thinking about the incremental margin or sort of the cost profile of that revenue as you bring it online? Thanks.
Scott Blackley -- Chief Financial Officer
Yup. On the fee-based revenue, I would just say on fee-based revenue, we started the Health First contract on January 1. That's going to be relatively stable throughout the year. And then in our C + O book of business, that scenario where we're hopeful and expect that we'll be able to continue to ramp that up, and that will drive fee-based revenue to increase throughout the year.
So I would say that, in general, it's going to be stable but growing throughout the year. On margin, look, I think that I would just say that we're expecting that that fee-based revenue is contributing positive margin to the bottom line starting in the first quarter. And so we're seeing that business generating positive returns and positive contribution to adjusted EBITDA.
Stephen Baxter -- Wells Fargo Securities -- Analyst
Thank you very much.
Operator
Thank you. The next question comes from the line of Jonathan Yong with Credit Suisse. Sir, your line is open.
Jonathan Yong -- Credit Suisse -- Analyst
Thanks for the question. So thanks for the details on the percentile on Silver tier. I guess is there something structurally difficult within the Bronze mix where it's just more difficult money there? Obviously, one of your peers today called out that they effectively exited the Bronze side of the tiers and moved all to Silver. So I'm curious from your perspective, given you have shifted more to Silver is what's the structural issue there? And could you eventually reexpand into Bronze? Or is it really just all a Silver game right now?
Mario Schlosser -- Co-Founder and Chief Executive Officer
Yeah. So we have -- so let me answer this with facts first. It is -- Bronze is a bit more structurally difficult to make money, and that part is true as compared to Silver for a couple of reasons. One is it is a lower PMPM number, generally, right? You're a tier below.
The second piece is that it often attracts more members, relatively speaking, who don't really utilize a whole lot -- and that has two effects. One is, it actually is worse for risk adjustments, again, relatively speaking, than having numbers to utilize sort of like average amounts, in a sense. But the other part actually is that those tend to also be members who have higher churn rates. And so there is sort of like a chunk of the ACA marketplace that is more easily changing plans from year to year and it's going to chase the lowest price plans.
In the past, it was maybe 15%, 20% of the marketplace. So it's hard to put a finger on really. And so you have that membership a bit more concentrated in the Bronze as well. Now those effects are not new.
They've been in place for the past many years, and we've found a number of antidotes, I would say, in these effects. For example, we think that some of what we're doing in virtual primary care is actually meaningful to build more attractive plan designs in Bronze and some of what we're doing around certain deductibles and other plan design elements we have in our Bronze plans has helped us shift -- have helped us shift up to PMPM in the Bronze a year. And so obviously, I think I mentioned last time that generally, even when you have a member who is not utilizing healthcare a whole lots. If we get that member into our digital interactions, we get higher retention rates out of them.
So about 6 percentage points, higher retention, the members engage with us digitally than the kind of the average book of business base in the year, that is not any different in the Bronze either. And so with all of these things together, we're comfortable in that here and have creative ideas, what else to do then the years going forward.
Jonathan Yong -- Credit Suisse -- Analyst
Great. That's helpful. And then you mentioned that you have an expectation of being at non-COVID utilization, it will be at baseline levels. I'm assuming this is a bit more gradual over the year.
I just want to confirm that. And is there any view of deferred care stepping up as COVID subsides? Thanks.
Scott Blackley -- Chief Financial Officer
Yeah. With respect to the MLR, I would say a few things, kind of looking at 2022. So one, this year, as we've talked about, we price for better margins. So we're assuming that price to cover cost trends and we price for an endemic level of COVID spend.
So that's going to be a positive factor for us. Secondly, I would just say that when we think about COVID as we've seen kind of Omicron starting to fade and some of the effects of that dropping off, we are based on having an endemic level of COVID in our assumptions, we are expecting that we'll see utilization from non-COVID sources normalizing throughout the rest of the year. So at this point, again, I'm anticipating that we're going to have about on a year-over-year basis between '21 and '22, we'll have about 400 basis points of improvement in the MLR, primarily driven by COVID to a lesser degree, some of the SEP things that we saw. And then we also have opportunities in the MLR from some structural advantages of scale.
And having a larger membership book, we think there's some other opportunities for us to continue to drive improvements as well. So those are kind of the key points that you're going to drive the year-over-year change.
Mario Schlosser -- Co-Founder and Chief Executive Officer
Yeah, maybe I'll add two more points that I find interesting. One is that we have not seen a lot of catch-up here, as I think we talked about in the past as well. And if we look at that number and refresh stats and then the metastatic cancer rate, for example, in past diagnosis have been very much on the same level in 2019, '20 and '21. So there's not a lot of evidence there that somehow disease burden is getting worse because care has to get caught up to work.
The other point we pointed out last year is that SEP members when they came in last year, it will have a bit higher organization early on with hypertensive care utilization early on. And so you can wonder there. So a different segment of the market now suddenly coming in there and what will that do. And one new data point we have there is that the retention rate on those SEP folks was actually the same as the retention rates into this year of the non-SEP folks last year around 80% as we talked about.
And I would say that that is at least a data point that the population is not that different. We sort of like behaving similarly and therefore, not a lot of evidence here that that will be a catch up either. We're obviously going to watch that very, very closely. I think we can do a fair amount of that also with our engagement on the members with the provider enablement and so on.
Jonathan Yong -- Credit Suisse -- Analyst
Great. Thanks.
Operator
Thank you. The next question comes from the line of Josh Raskin with Nephron Research. Please go ahead.
Josh Raskin -- Nephron Research -- Analyst
Thanks, and good evening. My question is around consumer engagement. Mario, you're talking about this, and I'm specifically interested in the digital engagement on the consumer side. Can you give us a sense -- and I think you gave us some data when you guys were going public, but could you give us a sense on differences by demographic and if that's changing at all or any expectations in 2022? And then are you finding a correlation -- I heard the NPS correlation with digital engagement, but is there an MLR correlation that you guys are seeing in terms of those that are digitally engaged versus not?
Mario Schlosser -- Co-Founder and Chief Executive Officer
Yeah. So in terms of statistics, we've talked in the past about how members who created digital profile, for example, are 80% in the fourth quarter of last year, and that's still been around 75%. And obviously, that's probably influenced by SEP where we need always some time to kind of create that digital engagement and for people to come in. We still have -- if you look at mobile app downloads of membership base, we still have a much higher mobile app download rate [Inaudible] impression a few weeks ago than pretty much anybody else out there in the health insurance industry from what we can tell.
So look at kind of app store numbers and number of things like that there. So those -- that's how we drive engagements, where we -- so in terms of how that looks across the age ranges, there is an impact. So you have in the 56- to 64-year-old segments, probably about 25% or so lower digital engagement, as compared to the younger segments there. But if we then look at the overall engagement with Oscar, that tends to be pretty similar because they then end up having more conversations with their consumer teams, for example.
The other nice statistics that I mentioned in the last earnings call that I want to reiterate as well is if you look at all of the conversations we've had with members since the beginning of this year, right? And this is, again, obviously, double membership. And we got a year older on average membership base, shifting more toward Silver, chronically ill and so on. You look at all those conversations beginning of the year, 40% of those conversations were digital, meaning in secure messages between the care guides and the member through the mobile app effective on the website. I think also very powerful proof point there that even in a new segment in a sense.
So a new membership base, we can right away, get some engagement there. High number that I think is very interesting is that we just do a lot to outbound engagement as well. And the latest number I have there for you is that on a weekly basis, there's about 25% of members who engage with one of our outbound messages, it can be email campaigns, text messages and [Inaudible] messages in the mobile app and things like that. So the answers are very consistent.
Now the impact on the MLR, we like to really look at in more sort of like nuance detail there and sort of trace through directly. And one piece of data that we have there now is that when you look at the members in virtual primary care, plan designs, the number I gave, I think, last time was that about 44% or so of those members say that they didn't have a PCP before they came on board with our essentially virtual -- or the Oscar is going to go virtual PCP, and we are seeing impact there on the total cost of care on a monthly basis. And that is coming through, for example, by having refer to better more efficient downstream specialists and by kind of some other moves in shifting more toward drugs that were effective and efficient from a cost point of view as well. And that, to us, suggests also that we have more opportunity there of getting that MLR down.
So that's kind of a couple of data points for you there. We're going to keep very closely working on that this year. And as I mentioned, we're happy with how we've really grown membership base from the last couple of years, but at the same time, really got good news on the MLR as well. And they're really, in our view, is quite a bit more of opportunity of [Inaudible] to do that in the next couple of years.
Josh Raskin -- Nephron Research -- Analyst
Great. I think that MLR data would be helpful to understand the engagement. And just a quick follow-up. Can you just remind me, and I know I should know this on the accounting side, the PDR was up in 4Q this year versus down last quarter.
And it felt like -- is that -- was that indicative of any change in expectation for 2020 to over the last three months? Or why -- what was the difference there?
Scott Blackley -- Chief Financial Officer
Yeah. So you're right. We built PDR in 2020. Obviously, that build was related to our expectations for '21.
And then in 2021, we had a smaller PDR, so we had a release of reserves. And I would just say, in general, two things: the PDR that we had in 2020 had -- was kind of split between individual and MA. And as I look at the 2021 PDR that's really related more toward our non-individual businesses. And I think it just really represents the fact that as we are seeing better performance across our book.
We're certainly getting more scale, as we've talked about that results in fewer plans that have a deficiency reserve related to them. So that's really the driver of why you see a lower PDR at the end of 2021.
Josh Raskin -- Nephron Research -- Analyst
Gotcha. So there's still a PDR accrual. It's just the change in the amount of accrual that got better. Is that the way to think?
Scott Blackley -- Chief Financial Officer
You've got it. Absolutely. Again, the balance sheet, we had $85 million at the end of 2020. We've got about $29 million at the end of 2021.
Operator
Thank you. And this will be our last question, and it will be from Nathan Rich with Goldman Sachs. Please go ahead.
Nathan Rich -- Goldman Sachs -- Analyst
Hi. Good afternoon, thanks for the question. On MLR, Mario or Scott, could you update us on what you've seen in the cohort data, and how MLR tends to trend in the second and third years of members are with you. And relatedly, is there a kind of target level of MLR that you feel like the business needs to achieve to reach profitability for the InsureCo?
Scott Blackley -- Chief Financial Officer
Yeah. So with respect to the MLR, we certainly have data about how membership is -- how that performance accrues over time. I would say that there's actually not a huge amount of difference in the near term as you see members. In the first year, there's a little bit of a lull as those members are onboarding and getting into their routines with their physicians and pharmaceuticals, etc.
And then that starts to stabilize over time. So nothing in the near term there that I would call out. And then on a broader perspective, if we think about MLR in general with that new population, I think that we feel like this is a population that we have pretty consistently been able to grow and see these kinds of new members come into the book. And we've got good experience there.
So our track record gives us confidence that we're going to be able to continue to bring on these new numbers and manage that MLR.
Nathan Rich -- Goldman Sachs -- Analyst
OK, great. Thank you.
Operator
[Operator signoff]
Duration: 45 minutes
Call participants:
Cornelia Miller -- Vice President of Corporate Development and Investor Relations
Mario Schlosser -- Co-Founder and Chief Executive Officer
Scott Blackley -- Chief Financial Officer
Ricky Goldwasser -- Morgan Stanley -- Analyst
Adam Ron -- Bank of America Merrill Lynch -- Analyst
Stephen Baxter -- Wells Fargo Securities -- Analyst
Jonathan Yong -- Credit Suisse -- Analyst
Josh Raskin -- Nephron Research -- Analyst
Nathan Rich -- Goldman Sachs -- Analyst