Image source: The Motley Fool.
Evolent Health (EVH -3.21%)
Q4 2021 Earnings Call
Feb 23, 2022, 5:00 p.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Welcome to Evolent Health's earnings conference call for the fourth quarter and year ended December 31, 2021. As a reminder, this conference call is being recorded. Your host for the call today from Evolent Health are Seth Blackley, chief executive officer; and John Johnson, chief financial officer. This call will be archived and available later this evening and for the next week via the webcast on the company's website in the section entitled Investor Relations.
I will now hand the call to Seth Frank, Evolent's vice president of investor relations. Please go ahead.
Seth Frank -- Vice President of Investor Relations
Thank you, and good afternoon. This conference call will contain forward-looking statements within the U.S. federal laws. These statements are subject to risks and uncertainties that could cause actual Evolent Health results to differ materially from historical experience or present expectations.
A description of some of the risks and uncertainties can be found in the company's reports that are filed with the Securities and Exchange Commission, including cautionary statements, including our current and periodic filings. For additional information on the company's results and outlook, please refer to its fourth-quarter press release issued earlier today. Finally, as a reminder, reconciliations of non-GAAP measures discussed during today's call to the most direct comparable GAAP measures are available in the summary presentation available in the company's Investor Relations section of our website or in the company's press release issued today and posted on the Investor Relations section of the company's website, ir.evolenthealth.com, and the Form 8-K filed by the company with the SEC earlier today. During management's presentation and discussion, we will reference certain GAAP and non-GAAP figures and metrics that can be found in our earnings release, as well as a summary presentation available on the Events section of Evolent's IR website, ir.evolenthealth.com.
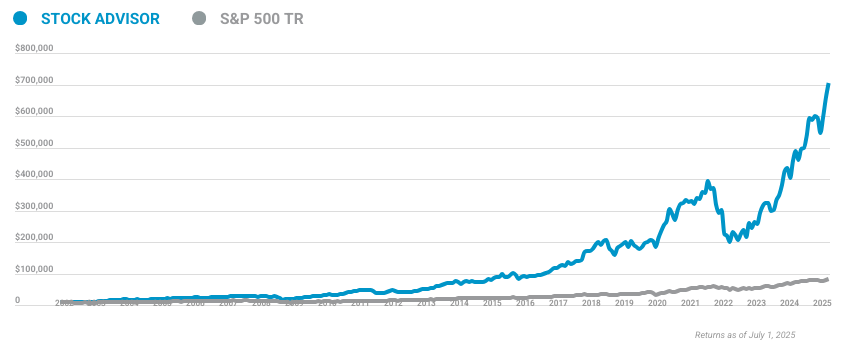
10 stocks we like better than Evolent Health
When our award-winning analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Evolent Health wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of January 20, 2022
And now I'll hand the call over to Evolent's CEO, Seth Blackley.
Seth Blackley -- Chief Executive Officer
Good afternoon, everyone, and thank you for joining the call. Today, I'll summarize the results for the fourth quarter and full year 2021, as well as the outlook for 2022, then I'll turn to an update of our three primary investment themes of strong organic growth, expanding margins, and optimal capital deployment. And I'll wrap up with the macro industry environment update. John will provide a detailed dive on the Q4 numbers, our 2022 outlook, and medium-term revenue and margin targets.
As always, we'll close by taking your questions. Turning to the key financial results for the fourth quarter of 2021 ending December 31, 2021, Evolent Health total revenue was $248.4 million. Revenue, excluding divested assets, was $245.9 million, reflecting a 39.7% year-over-year revenue growth rate. Adjusted EBITDA for Q4 was $24.3 million, compared to our Q4 outlook of a range of $14 million to $18 million.
During the fourth quarter, we closed the acquisition of Vital Decisions, which contributed approximately $5 million of Q4 revenue and approximately $1 million of Q4 adjusted EBITDA, consistent with expectations. Underlying our strong performance is the year-over-year growth in lives under management, the key volume component of Evolent's revenue. As of December 31, 2021, Evolent's services covered 20 million lives with 1.6 million managed within Evolent Health Services and 18.4 million lives in our Clinical Solutions segment. Lives in our Clinical Solutions segments are composed of 1.5 million lives managed under our risk-based performance suite through New Century Health and Evolent Care Partners.
And as of the end of December, we supported an additional 16.9 million lives through New Century Health's Technology and Services platform, inclusive of the Vital Decisions acquisition. For perspective, Evolent's contracted solutions currently cover approximately 6% of the U.S. population. For the full year 2021, we ended the year with total revenue of $908 million and $890.6 million of revenue, excluding divested assets.
This reflects growth of 36.7%. Adjusted EBITDA for 2021 totaled $66.3 million, representing growth of 36.5% year over year. These results are ahead of our medium-term revenue targets and tracking to our 2024 adjusted EBITDA margin target. The results also exceed the high end of our initial guidance for 2021 of $830 million to $880 million of revenue and adjusted EBITDA of between $40 million and $50 million.
The fourth quarter of 2021 marks the capstone of a highly successful year for Evolent across key performance metrics, and we're pleased with the continued momentum driving our business, as well as the impact Evolent is delivering for employees, partners, patients, and our mission. John will provide our complete 2022 outlook later in the call, but I'm also pleased that we expect 2022 total revenue growth between 23% and 30% and adjusted EBITDA of between $80 million and $90 million. Across the top and bottom lines, we continue to be on a path to deliver on or exceed our medium-term revenue growth and adjusted EBITDA targets. On behalf of Evolent's leadership team and Evolent's board of directors, I want to express my appreciation to all 3,500 Evolenteers worldwide.
Their passion and commitment to improving healthcare through innovation continues to contribute to the quality and efficiency of healthcare delivery in the United States. I continue to be highly impressed with our team, and I'm proud to report that, even through the pandemic and upheaval in the broader economy, our employee engagement score is at an all-time high, and Evolent remains a highly desired destination for a diverse and productive workforce. Now, let's discuss our ongoing progress against Evolent's three core operating objectives: number one, strong organic growth; two, expanding margins; and three, optimal capital allocation. Touching our first theme of strong organic growth, we're pleased to announce four new operating partners today.
As a reminder, we consider new operating partners to include both new partner logos, as well as any significant geographic expansions with existing partners using our clinical performance suite. We're pleased to have added 10 new partners during 2021 versus our annual target of six to eight partnerships, and we're off to a strong start in 2022 with today's announcements. Three of the four new partnerships announced are for New Century Health with Molina Healthcare, an important and growing partner. We have signed an agreement to bring our cardiology performance suite to Molina Nevada.
In addition, Molina Healthcare in Kentucky and Washington State have elected to migrate from our Technology and Services suite to our Cardiology Performance Suite. With these three expansions, in addition to the previously announced Performance Suite relationship with Molina Ohio, we anticipate Molina will contribute more than $75 million of revenue in 2022, with the opportunity to continue to grow in future years. Further, we feel that the conversion from New Century Technology and Services to our Performance Suite is further evidence of the value we provide to our partners and to the expansion opportunity we see within our existing partner base. In deploying the Performance Suite, payers and risk-bearing providers are seeking a partner who can guarantee cost reduction and quality improvements in high-cost specialties.
We believe we offer a compelling value proposition, whereby a health plan partner transfers responsibility for a scope of medical cost to Evolent. We, in turn, drive our margin by capturing the clinical savings we create from that capitation rate using our advanced technology platform, scaled services, and our proprietary clinical intellectual property. We are pleased that we have also extended this Performance Suite model to primary care through our Evolent Care Partners business. As such, our fourth new partnership announcement is the first primary care performance suite agreement for Evolent with Blue Cross Blue Shield of North Carolina.
Effective in January 2022, Evolent Care Partners and its network of independent primary care physicians began managing over 10,000 Blue Premera members. Evolent Care Partners will leverage our proprietary Identifi platform, proven care management, and patient engagement programs to improve quality and reduce unnecessary costs. Blue Cross and Blue Shield of North Carolina is a leading payer in the value-based care space, and we look forward to collaborating with them to improve the health of communities across North Carolina. Rounding out our growth news today, we are disclosing that our previously announced Evolent Health Services national payer is Bright HealthCare.
Beginning January 1, 2022, we went live with a multiyear operational partnership, whereby Bright will leverage Evolent's health plan administrative services to initially support an estimated 350,000 commercial and Medicare Advantage members. We're delighted to work with Bright as they integrate vendor relationships and seek to expand their unique patient-centered integrated payer/provider model to the health plan market. Moving to our second objective of margin expansion. We're pleased with our progress toward our medium-term margin targets.
Given our high revenue growth rates and larger portion of mix from Performance Suite products, which have lower Year 1 margins and higher margins in later years, we will continue to see some fluctuations in year-to-year EBITDA margin percentages. Our high revenue growth rates give us greater conviction with our medium-term outlook, including confidence of reaching our absolute adjusted EBITDA dollar goals, which we believe to be the best indicator of success on our margin expansion targets. Finally, I'd like to discuss our third theme of shareholder value creation for Evolent, which is optimal capital allocation. Even as we rapidly scale our business, our execution and our differentiated solutions increasingly generate higher levels of operating cash flow, enabling us to further accelerate our market leadership.
As we think about capital deployment, our priority is to drive innovation and market leadership around our core three solutions: first, through continued R&D in our core business; second, through strategic M&A in the core; and third, through innovative capital-light partnerships. Regarding R&D within the core, we plan to continue steady and disciplined investment around our primary solutions. For example, within Evolent Health Services, we're leveraging artificial intelligence and other technology investments to scale high-volume transaction processing activity more efficiently for our provider and health plan partners. Regarding M&A, our 2021 acquisition of Vital Decisions is a good example of how we use M&A to extend our market leadership.
By integrating Vital Decisions into New Century Health, we add important capabilities to better manage overall end-of-life quality and cost. According to CMS and published studies, direct medical costs during the last 12 months of a person's life are approximately 20% of total Medicare spending. Vital Decisions greatly enhances and deepens our ability to impact those costs, especially within oncology and cardiology, which represent the majority of end-of-life medical expenditures. Our Vital integration is going well and is on schedule.
During 2022, we'll continue to evaluate other strategic accretive acquisition opportunities. Given our market leadership position and high demand in the market, we continue to see particularly interesting opportunities to deepen and broaden the New Century platform through continued M&A. Third, we also seek to innovate through partnerships with no or minimal use of R&D or M&A capital. For example, within oncology, we are partnered in the evolving pharmacogenomic space.
This relationship seeks to further optimize treatments that maximize efficacy, effectiveness and minimize the risk of side effects. In addition, we're partnering with the Welsh, Carson Valtruis-backed organization that seeks to expand oncology care capacity with a new hybrid value-based delivery model. Finally, complementing our primary care-centric focus with Evolent Care Partners, we have partnered with an organization to support early identification and treatment in kidney care. These relationships and others like them accelerate and enhance our existing solutions, allowing us to innovate without deploying significant capital.
Collectively, across our R&D, M&A, and focused business partnerships, we remain optimistic regarding our ability to extend Evolent's market leadership and to continue to build long-term profitable growth. To conclude, I want to give you our perspective on where the current environment stands as it pertains to value-based care in both the public and private sectors. As many of you know, there are many value-based care models and experiments going on, all attempting to bend healthcare's unsustainable cost curve while improving quality. On the public side, as you're likely aware, CMS seeks to ensure 100% of Medicare, and most Medicaid beneficiaries are in value-based relationships by 2030.
The Medicare Shared Savings Program generated a sevenfold increase in total earned shared savings between 2013 and 2020, with dramatic savings acceleration between 2018 and 2020. Also importantly, CMS reports average quality scores for the programs for 2020 were 97%, the highest level since the initiation of the program. As previously discussed, we chose not to participate in the Center for Medicare and Medicaid Innovation's direct contracting model and instead focus on the more proven but similar Medicare Shared Savings Program called Pathways to Success. While the various model formats will surely evolve to reflect stakeholder feedback over time, we're highly confident in our near-term Evolent opportunities with the current Pathways to Success program.
We're also confident that there's broad bipartisan support for value programs in the years and decades ahead. More importantly, we also continue to see a strong push to value models in the private payer and risk-based provider markets. As evidenced by numerous national payers and risk-bearing providers highlighting their efforts to drive costs down and quality up through engaging their provider networks, we continue to see strong demand for our solutions. Taken together, the impact of policy and the private market direction, these trends give us confidence that we'll have strong macro tailwinds for years to come.
I'll now ask John to give some detail on the numbers this quarter and also provide our outlook.
John Johnson -- Chief Financial Officer
Thanks, Seth, and good evening, everyone. Overall, we're very pleased with our achievements relative to our 2021 financial goals, exceeding the high end of our initial and updated ranges for both our revenue and adjusted EBITDA targets and consistently delivering on all three of our strategic goals: strong organic growth, expanding margins and efficient capital allocation. We came into 2021 with a strong visibility to exceeding our mid-teens organic growth target. After adding 10 new partnerships, as well as driving strong same-store sales growth throughout the year, we further exceeded expectations, achieving 37% growth for $891 million of revenue, excluding divested assets, compared to $652 million in 2020.
On the bottom line, we ended 2021 with total adjusted EBITDA of $66.3 million or 7.3% of revenue, 210 basis points ahead of the midpoint of our initial 2021 guidance. Our strong margin expansion across 2021, the result of accelerated cost-reduction efforts, as well as the rapid maturation of some of our newer clinical partnerships, puts us ahead of schedule coming into 2022. This profitability expansion, combined with a continued disciplined approach to investment in capitalized software development, further allowed us to expand our operating cash flow during the year, delever our balance sheet, and continue to bolster our cash reserves for future strategic investments. We ended the year with $215.6 million of available cash and net leverage of 1.1 times our trailing 12-month adjusted EBITDA, down 2.1 turns from where we began the year.
Now, turning to our consolidated fourth-quarter results. Total revenue of $248.4 million in the quarter represents an increase of 0.7% year over year. More importantly, revenue less divested assets of $245.9 million increased 39.7% from $176 million in the prior year due to growth from new partner additions, as well as same-store sales growth. Adjusted EBITDA grew to $24.3 million, compared to $20.4 million in the same period of the prior year.
The revenue and adjusted EBITDA outperformance was driven in part by approximately $6 million in positive revenue impact from strong performance on contracts within our Clinical segment, which related to earlier months in 2021. If these revenue impacts were allocated into the periods to which they relate, Q4 adjusted EBITDA performance would have been in line with the high end of our Q4 guidance range, specifically $18 million, with a margin of 7.4%. Turning to our segment results. Within our Clinical Solutions segment, revenue in the fourth quarter increased 9.9% to $161.1 million, up from $146.6 million in the same period of the prior year.
Excluding revenue from divested assets, Clinical Solutions revenue grew 47.7%. Q4 adjusted EBITDA from Clinical Solutions was $29.5 million, compared to $8.6 million in the prior year. This EBITDA outperformance was largely driven by the aforementioned revenue true-ups. Membership in our Performance Suite for Clinical Solutions was 1.5 million, relative to 1.6 million in Q4 of the prior year, with a PMPM fee of $32.33 versus $28.55.
Membership in our Technology and Services Suite for Clinical Solutions was 16.9 million, relative to 6.2 million in Q4 of the prior year, with a PMPM fee of $0.39 versus $0.43 in Q4 of the prior year. The PMPM decrease was in line with expectations as we saw faster growth in Medicaid and commercial lines of business. Sequentially, our Technology and Services suite lives grew 5.2 million versus Q3, largely driven by both continued new market rollout progress across existing New Century customers, as well as the addition of 2.3 million lives from Vital Decisions. Within our Evolent Health Services segment, fourth-quarter revenue decreased 12.7% to $87.2 million.
Excluding revenue from divested assets, Evolent Health Services revenue grew 26.5%. Membership in our Performance Suite for Evolent Health Services was 1.6 million, compared to 1.9 million in Q4 of 2021, with a PMPM fee of $17.25 versus $17.63. Adjusted EBITDA from our Evolent Health Services segment for the quarter was $7.9 million, compared to $21.4 million in the prior year. Looking at the year-over-year comparison, Evolent Health Services EBITDA in the same quarter of 2020 was positively impacted by a performance payment related to certain of our divested health plan assets.
Finally, corporate costs increased to 37% to $13.1 million, up from $9.6 million in the same period of the prior year. This increase was primarily related to one-time and seasonal costs, and we expect corporate costs in '22 to return to levels consistent with the first three quarters of 2021. Turning to the balance sheet. We finished the quarter with $266.4 million in cash, cash equivalents, and investments, including $50.8 million in cash held in regulated accounts related to the wind-down of Passport.
Excluding cash held for Passport, we have $215.6 million of available cash, an increase of $24.7 million versus the end of the third quarter. This increase was principally driven by our strong adjusted EBITDA performance, as well as strong collections activity to close out the year. Cash deployed for capitalized software development and other capex in the quarter was $6.5 million. One subsequent event of note from a cash perspective, in January, we received the second half of the earn-out payments owed to us by Molina as part of the Passport transaction, adding another $23 million of available cash to our balance sheet, but not yet reflected in the $215.6 million cash balance at the end of Q4.
We have no upcoming debt maturities until late 2024 and continue to expect our operating cash flow to be positive across all of 2022 and beyond, giving us the ability to continue to invest in differentiating our core services while maintaining a strong and a flexible balance sheet. Turning now to our 2022 outlook. On the top line, we again come into the year with strong visibility and the vast majority of revenue at the midpoint of guidance under contract. On the bottom line, we come into the year with our unit cost profile right where we want it and with our recent Clinical segment go-lives ramping nicely toward run-rate profitability.
As Seth noted, our outsized growth rate is driven principally by a higher mix of Performance Suite products, and these have lower Year 1 margins that progressively move higher annually over three years. Given these dynamics, we are focused on absolute adjusted EBITDA dollars, and the midpoint of our outlook represents 28% year-over-year growth in dollar-based adjusted EBITDA compared to our strong 2021 results. Now, let me turn to guidance. For the full year, we expect total revenue of $1.12 billion to $1.18 billion.
With respect to full-year adjusted EBITDA, we are forecasting a range of $80 million to $90 million. We anticipate deploying approximately $25 million to $30 million in cash for capitalized software development across the year. For the first quarter of 2022, we are forecasting total revenue of $280 million to $295 million and an adjusted EBITDA of $20 million to $25 million. Finally, we anticipate some modest seasonality in performance payments this year, with the first and third quarters of the year projected to be slightly higher revenue and EBITDA than Quarters 2 and 4.
With that, we are ready to take your questions.
Questions & Answers:
Operator
We will now begin the question-and-answer session. [Operator instructions] And our first question will come from Ryan Daniels of William Blair. Please go ahead.
Ryan Daniels -- William Blair & Company -- Analyst
Yeah. Good evening, guys. Thanks for taking the question, and kudos on a very strong year and outlook. Seth, maybe I'll start with one for you.
Can you talk a little bit more about the up-sell to Molina maybe as a case study just in regards to any learnings on the upsell process and how that could translate into similar growth opportunities into other accounts in the future?
Seth Blackley -- Chief Executive Officer
Yeah, happy to, Ryan. So, you know, just in general, the way that things work with a situation like that or some of our other relationships is that we have two vectors for growth, right? One is if we already have the Technology and Services suite in place, which is the lower PMPM, we have an opportunity to talk to those markets where we're already live, already have their data, about the opportunity to convert that opportunity into the full Performance Suite, which obviously has much higher PMPMs, as we've talked about, and ultimately has, I think, better savings for our partner, the payer, but also higher margin for us over time. So, that's one vector. The second vector is around just new geographies, right? So, we already have a relationship with a couple of states.
We have a relationship with corporate. They're willing to introduce this to the other states, and there's an opportunity to go do that. And obviously, with Molina, we've had a little bit of both in this announcement. And I think what's interesting, which we try to continue to talk about, Ryan, is that we've got within our top handful of customers, 40 million lives.
And if you think about a $35 PMPM on those 40 million lives, obviously, that's $15 billion-plus, higher than $15 billion of opportunity, and that would be kind of a fuller penetration opportunity. But we are methodically looking at whether it's with the relationship you mentioned or any of our others with those 40 million lives, those kinds of opportunities. And so, we'll see, I think, more of those over time, and it's a great tailwind to our growth in addition to obviously adding new logos.
Ryan Daniels -- William Blair & Company -- Analyst
Yes. And the reason I ask, I mean, it's a great case study, and the data point you just mentioned is such a large opportunity for you. What, especially when you have the relationship on the technology side and have the data and can kind of validate the potential savings, what tends to be, if anything, the roadblock to moving to the Performance Suite?
Seth Blackley -- Chief Executive Officer
Yeah. It's -- you know, look, I think we do have good track record. It is all about creating value, to your point. We have to prove the value.
We have to prove we're a good partner. We have to do what we say we're going to do and execute. So, we've had a good track record of doing that. From there, it really is about two things.
One is sort of dynamics within that organization, how much pressure are they feeling if it's an organization that wants to drive savings. Or secondly, how good of a job can we do at proving that we can help drive incremental savings or opportunities. And the barriers on the second one really is just about -- the first one sort of market-driven. The second one would be really around proving the actuarial case around the savings.
And it takes a little bit of time to do that, but we feel very confident in the fact that the value proposition is typically there. And so, we see lots of opportunity like this.
Ryan Daniels -- William Blair & Company -- Analyst
Got it. Thank you. And then one for John. As you move more of the business to the Performance Suite and just based on the new contracts you've sold, do you envision a larger percentage of your revenue coming from Performance-based fees in 2022 relative to past years?
John Johnson -- Chief Financial Officer
Hey, Ryan, it's a good question. On the whole, if you look over a number of years here, we have had an increase in our overall revenue moving toward the Performance Suite. So, the short answer is yes. I think we do expect that here in '22.
Two things that I'd just point out on that. One is obviously significant opportunity on the top line. And two, while it takes, as you know, a couple of years maybe to get to full run rate, the opportunity for dollar PMPM EBITDA on those performance fee contracts is among the highest in our portfolio of products. So, we really like that opportunity.
Ryan Daniels -- William Blair & Company -- Analyst
Great. Thank you. And then one last one, Seth, for you. I ask this every few quarters.
But I'm curious, if you look at the pipeline, if you're seeing any inflections in demand for different products or different end markets, whether it's Medicare, Medicaid, commercial. Just kind of what are you seeing as you look in the pipeline on a go-forward basis? Sorry, I got something caught my throat.
Seth Blackley -- Chief Executive Officer
No problem. It's the time of year. Ryan, we do see, I'd say, an inflection in the pipeline over the last really year or two. And it really, I think, is across all three solutions right now.
We've had really good success across all three. I'd say, if I wanted to point out particular places of inflection, where we can guarantee our results through our Performance Suite, whether that's in New Century or with our newly announced Evolent Care Partners relationship, I think those are particularly interested in the marketplace. And within that group of solutions, we've seen, I would say, cardiology and oncology as high-cost specialties and now end-of-life as places where the payer risk-bearing provider community are looking for ways to drive down cost. If we can guarantee it and do it a way that's better for members, higher quality, there's a lot of demand for that.
Ryan Daniels -- William Blair & Company -- Analyst
Great. Thank you so much, guys. Nice quarter.
Seth Blackley -- Chief Executive Officer
Thanks, Ryan.
Operator
The next question comes from Anne Samuel of J.P. Morgan. Please go ahead.
Anne Samuel -- J.P. Morgan -- Analyst
Hi, guys. Congrats on the terrific results. My question was a little bit more on your longer-term revenue target. You did 36% growth this year when you back out the divestitures.
You're expecting to see north of 20% organic growth next year. Is it fair to think that maybe you can continue on a trajectory a little bit north of that mid-teens in the future?
Seth Blackley -- Chief Executive Officer
Yeah, Anne. It's a great question. And when we get a fair bit, we obviously have been trending well above. We're not changing the target right now on the mid-teens, but we have been beating it, and we want to continue to set numbers and expectations that we can exceed.
And we're focused on doing that each and every year. And for Ryan's question, it's just a fantastic end market that we're selling into. And great products with great traction. So, we feel really good about continuing to do well on the revenue side.
Anne Samuel -- J.P. Morgan -- Analyst
That's great. And then I was wondering if maybe we can get a little bit more color on the new partnerships around lives and expected PMPM.
John Johnson -- Chief Financial Officer
Anne, I'll take that. This is John. I'll start with Blue Cross. That was the one that we referenced in the JPMorgan presentation back in January.
You expect that to be north of $50 million in revenue here, the 10,000 members. On Bright Health, about 330 incremental 1,000 members, and so 350 total. And PMPMs there will vary based on the markets and specific scope and line of business for serving a number of different markets with them. We think in the range between seven and 11.
And on Molina, they're expecting, as those migrations happen over the course of this year, but up to the Performance Suite and then going live in Nevada and Ohio, that will be an addition of north of 500,000 members to the Performance Suite at New Century ramping over the course of the year.
Anne Samuel -- J.P. Morgan -- Analyst
That's really helpful. Thanks. And maybe if I could just sneak in one more. I was hoping you could provide any color on the Cook County RFP that's up for renewal.
Seth Blackley -- Chief Executive Officer
Yeah. In Cook County, we continue to expect the decision sometime later in Q1, could be the last few days of February, it could be in March. We feel very good about where we stand relative to the process and excited to get that outcome back and expect it pretty soon.
Anne Samuel -- J.P. Morgan -- Analyst
Great. Thanks, guys.
Seth Blackley -- Chief Executive Officer
Thank you, Anne.
Operator
The next question comes from Charles Rhyee of Cowen. Please go ahead.
Charles Rhyee -- Cowen and Company -- Analyst
Yeah. Thanks for taking the questions, and congrats on the results. Maybe first, I just wanted to ask a little bit about the Blue Cross Blue Shield North Carolina contract here. And maybe talk about when we think about Performance Suite offering, I mean, I assume that's what you're already doing with your partners in Evolent Care Partners.
Are there any differences here? Or is that just a new part of -- a new member within the Evolent Care Partners? Anything structurally that's different serving North Carolina?
Seth Blackley -- Chief Executive Officer
Yeah, Charles, great question. So, it is very similar to what we're doing with Evolent Care Partners on the Pathways to Success side and some more, frankly, than what we've been doing for a while in North Carolina. What's different is that the nature of the arrangement with the private payer, in this case, is structured as an aligned capitation style arrangement does give us some incremental controls on the cost side, which we think allow us to drive incremental value and the way that the revenue recognition and, again, the margin dollar opportunities are, I think, are obviously higher. But the fundamental work that we're doing is a little different around the edges because of some of those incremental controls that we have, but it is pretty similar.
It's one of the reasons we feel very confident about our ability to drive the performance here both because we know that these specific members have been in the state for a long time and because it's very similar to the scope of work that we have been doing for a period of time. But for those reasons, it is a little different than our traditional ECP arrangement.
Charles Rhyee -- Cowen and Company -- Analyst
OK. That's helpful. And maybe to follow up, I think Ryan was asking -- kind of alluded to a little bit earlier, right? Vital Decisions, those lives are sitting in the Tech and Services suite. Obviously, you're taking risk on the oncology and cardiology.
Is it possible to take risk for end-of-life care? Or is that kind of unique in the way that kind of care is delivered for you to be able to do so?
Seth Blackley -- Chief Executive Officer
Yeah. I mean, it's a good question, Charles. The way we think about that is to use the Vital Decisions' capability with our Performance Suite lives within New Century, right? So, we already are in the Performance Suite situation and deploying Vital there against cardiology and oncology, where about 70% of end-of-life cost sit, to begin with. And so, that's the way we think about it.
For a host of reasons, we are not contemplating sort of taking risk directly just on end-of-life, although that could be an opportunity one day. What we're really focused on is the true integration into New Century around cardiology and oncology.
Charles Rhyee -- Cowen and Company -- Analyst
OK. That's great. And then, you know, maybe one last question on the guidance. Obviously, strong revenue outlook.
Can you give us any more segment-level revenue guidance as we think between Clinical Solutions versus Health Services? Like where would more of the growth would you expect to be coming from? It sounds like because of Performance Suite with Molina, maybe more of the growth we should expect Clinical Solutions side?
John Johnson -- Chief Financial Officer
You know, Charles, historically, over the last couple of years, the majority of our growth has come from the clinical side. As we look at '22, it's pretty balanced, given the strength of growth across the business.
Charles Rhyee -- Cowen and Company -- Analyst
OK. And would that be the same on EBITDA as well?
John Johnson -- Chief Financial Officer
I think you'll continue to see EBITDA profiles be somewhat similar to where they've been in the last couple of years in terms of EBITDA margins by segment.
Charles Rhyee -- Cowen and Company -- Analyst
OK. All right. Thank you.
John Johnson -- Chief Financial Officer
Thanks, Charles.
Operator
The next question comes from Matthew Shea of Piper Sandler. Please go ahead.
Matthew Shea -- Piper Sandler -- Analyst
Hey, thanks, guys. Thanks for the question, and congratulations on another strong quarter. I wanted to touch on Molina again. Encouraging to see the upsell motion but was particularly surprised with the full suite deploying in Nevada.
As you continue to penetrate Molina and potentially some of these other payers that you've proven out the value proposition with, do you expect that you could launch in new geographies with the Performance Suite from Day 1? Or do you still expect kind of an up-sell motion from tech-enabled services to the full suite?
Seth Blackley -- Chief Executive Officer
Yeah. Matt, I think, you know, you're going to see some of both is the short answer. We can do it either way. For the reasons we've mentioned in the past, sometimes the tech services way is an easier way to get started, particularly with, I think, a national plan because of the ability to scale very quickly and then come in behind in the ways that we might want to support select geographies.
I think in the case of a regional plan that's really trying to drive performance in a quick period of time, you also might see us go live straight with the Performance Suite. So, could go either way. And again, we like to have both options because it gives us flexibility based on the needs of our customers.
Matthew Shea -- Piper Sandler -- Analyst
Got it. And then circling back to Cook County. Curious on the PCG consulting partnership, if that was all -- at all related to winning the RFP. And if so or if not, I would love to just hear more about that relationship and the plans that you have for it.
Seth Blackley -- Chief Executive Officer
Yeah. Look, we're very excited about the PCG relationship. It's really all about our corporate commitment to diversity, equity, inclusion and also about making sure that, from a supplier diversity perspective, when you think about our operations around the country, we're meeting the needs and objectives of our clients and our partners. And so, really, it's all about that.
It's part of a very long-standing commitment we've had in that space inside of Evolent and outside, and we're going to keep the foot on the gas pedal for a host of reasons on the DE&I, ESG side of our work. And so, this will be one of many things that I think you'll see across the year.
Matthew Shea -- Piper Sandler -- Analyst
Got it. Thanks, guys. Congrats again.
Seth Blackley -- Chief Executive Officer
Thanks.
Operator
The next question comes from David Larsen of BTIG. Please go ahead.
David Larsen -- BTIG -- Analyst
Hi. Congratulations on a very good quarter. Can you talk a little bit more about the arrangement that you have, I think, in North Carolina? It sounds to me like it's a large primary care group. And are you bearing risk with that primary care arrangement? It sounds like you've actually created a virtual primary care solution.
Is that correct or not? And then was that -- did you say that was the first one of its kind on a large scale? Any color there would be helpful.
Seth Blackley -- Chief Executive Officer
Sure, David. Yeah. So, we are partnered up with actually a handful of groups in North Carolina, the primary care groups. Yes, with Evolent Care Partners, our model is to work with the payer community or with CMS to take and manage a population, the total cost for that population.
And the Pathways to Success program, we rev rec net revenue because it's more of a gain-share model. This is more of a capitation model. So, yes, absolutely, there's risk included in it. We feel really confident about the margin profile.
Similar to other Performance Suite opportunities, right, where the PMPM or margin profile in Year 1, we have very high confidence on what that's going to look like and how it will ramp in Years 2 or 3, which again has been the main driver of the acceleration of EBITDA that we've had at the company over the last couple of years, and this just snaps right into that same framework in the same model. So, we're very comfortable with it. It is a capitation model. We see a really interesting opportunity in North Carolina to expand what we've already started with here, but we also see opportunities to do this in other geographies under the same Evolent Care Partners model.
David Larsen -- BTIG -- Analyst
Great. That's very helpful. And then just one more quick follow-up. There are some primary care entities in the market that have been facing some challenges related to their Medicare Advantage margins, either from higher claims costs related to Medicare members being impacted by COVID and having longer hospital stays or perhaps some premium pressure in MA in some areas.
Can you maybe talk about what you're seeing there if anything? And how do you guard yourself against that type of a thing impacting your risk-sharing side? Thanks.
Seth Blackley -- Chief Executive Officer
Yeah. Yeah, so look, our model is a bit different than sort of the some of the other primary care models. Ours is more of a capital-light model, right? This is a network of physicians that we put together. We don't employ them.
And we have close to a decade of experience doing this. And it's pretty similar to what we've been doing for the last decade. A couple of years ago, we evolved a little bit in terms of how we set it up economically, but it's the same thing we've been doing for a long time. And we have a long track record and a lot of confidence in what we're doing.
And I think the short answer is, no, we're not seeing a spike in claims costs or issues associated with our populations. And some of that may be due to a different model, different geographies, etc. But no, we're not seeing that. We had really good results last year in the core Evolent Care Partners business, as we talked about recently, and having the same results over the past months as well.
So, we feel good about it. I feel like there's a lot of upside to grow it.
David Larsen -- BTIG -- Analyst
Great. Thanks very much. Congrats again.
Seth Blackley -- Chief Executive Officer
Thanks, David.
Operator
This concludes our question-and-answer session. I would like to turn the conference back over to Seth Blackley for any closing remarks.
Seth Blackley -- Chief Executive Officer
Thanks for everybody's time. We look forward to connecting on the road or virtually. Have a good night.
Operator
[Operator signoff]
Duration: 49 minutes
Call participants:
Seth Frank -- Vice President of Investor Relations
Seth Blackley -- Chief Executive Officer
John Johnson -- Chief Financial Officer
Ryan Daniels -- William Blair & Company -- Analyst
Anne Samuel -- J.P. Morgan -- Analyst
Charles Rhyee -- Cowen and Company -- Analyst
Matthew Shea -- Piper Sandler -- Analyst
David Larsen -- BTIG -- Analyst