Image source: The Motley Fool.
Signify Health, Inc. (SGFY)
Q4 2021 Earnings Call
Mar 03, 2022, 8:30 a.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Good morning. My name is Juan, and I will be your conference operator today. At this time, I would like to welcome everyone to the Signify Health fourth quarter 2021 earnings conference call. [Operator instructions].
Thank you. At this time, I will hand over to your host, Jennifer DiBerardino, head of investor relations. Jennifer, you may begin your conference.
Jennifer DiBerardino -- Head of Investor Relations
Good morning, and welcome to Signify Health's fourth quarter and full year 2021 earnings conference call. This call is being webcast live, and a recording will be available on the events page of our investor website at signifyhealth.com through May 3, 2022. Throughout the call this morning, we will be referencing the financial tables that appeared in our press release dated March 2, 2022. In addition, the fourth quarter and full year 2021 earnings call summary slide presentation we have posted to the events page of the IR website.
This morning, we will discuss Signify Health's business outlook, and we will also make certain statements about our future performance, including projections about our future financial performance; our anticipated growth strategies; anticipated trends in our business and our outlook, including estimates for total GAAP revenue, total adjusted EBITDA, in-home evaluations, bundled payment program size, and bundled payment weighted average savings rate. These statements are only predictions based on our current expectations and projections about future events and constitute forward-looking statements within the meaning of the federal securities laws. There are important factors that could cause our actual results, level of activity, performance or achievements to differ materially from the results, level of activity, performance or achievements expressed or implied by the forward-looking statements. Please note the cautionary language about our forward-looking statements as presented in our earnings press release and in our annual report on Form 10-K, which will be filed later today.
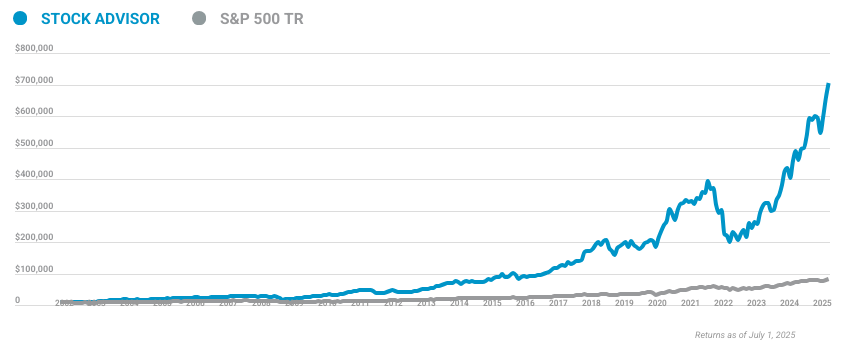
10 stocks we like better than Signify Health, Inc.
When our award-winning analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Signify Health, Inc. wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of January 20, 2022
That same cautionary language applies to the statements made in this conference call. We will also discuss certain non-GAAP financial measures, including adjusted EBITDA and adjusted EBITDA margin. Reconciliations to the relevant GAAP numbers for these non-GAAP measures are included in the earnings release filed on Form 8-K yesterday and also in our Form 10-K, which will be filed later today. As a reminder, we intend to participate in industry or sell-side sponsored conferences.
In lieu of issuing a press release to announce each conference, we will be posting our conference attendance on the events page and calendar of our investor relations site at signifyhealth.com. I encourage you to register for alerts on the investor site so that you receive an email notification each time we add a conference, other events or other updates to the investor relations calendar. Joining me on the call today are Kyle Armbrester, chief executive officer; and Steve Senneff, president and chief financial officer. Kyle will provide a business overview, followed by Steve with a financial overview.
We will have an operator-facilitated question-and-answer session after our prepared remarks. Now I will turn the call over to Kyle.
Kyle Armbrester -- Chief Executive Officer
Thank you, Jennifer. Good morning, and thank you for joining us. As I sit here this morning and reflect on the past 14 months, I'm proud of and thankful for all we've achieved. We successfully managed through another year of the pandemic, and we continue to evolve with our clients as they turn to us to support them in new ways.
Our accomplishments were many and, to name a few, we are recognized by Fast Company's annual list of the World's Most Innovative Companies. We launched new products and programs like transition to home and our partnership program, and we continued to successfully execute operationally to exceed our financial targets each quarter. On Tuesday, we closed on our first significant acquisition as a public company of Caravan Health, a leader in enabling accountable care organizations, or ACOs, to excel in population health management and value-based payment programs. We went through a robust diligence process to find Caravan and feel this is a great match as they share our passion for partnering with provider organizations to share risk and drive better patient outcomes.
While a lot changed with Signify in 2021, what remained constant is our dedication to driving forward our vision of transforming the U.S. healthcare system from fee-for-service to value-based payment. Yesterday evening, we announced our financial results for the fourth quarter and full year 2021 and guidance for another strong year in 2022. For 2021, revenue grew by a strong 27% to $773 million, and adjusted EBITDA increased 37% to $171 million from a year ago, largely driven by our in-home evaluation, or IHE volume growth and our home and community service segment, or HCS.
For 2021, we performed over 1.9 million IHEs, reflecting significant expansion with our clients that will continue to drive IHE volume growth into 2022 and beyond. Results in our episodes of care or ECS segment for 2021 reflected the ongoing impact of COVID-19 with its variants driving pressure in program size and savings rate. We expect these impacts to lessen over time as COVID cases continue to decline, but we have factored in some ongoing impact into our 2022 outlook. We are proud of our significantly improved outcomes we've helped to achieve for beneficiaries and the savings we've generated for our provider partners in the BPCI-A program and with our commercial clients.
Provider partners are committed to bundled payment programs, and we believe CMMI is also committed and will announce a new iteration for 2024 within the next 12 months. We are very excited about the opportunity we have with Caravan Health and our ongoing efforts to expand our reach in value-based care. The combination enhances the value proposition to providers as our services will have a multi-payer applicability to a larger portion of a provider's panel. By multi-payer, we're referring to our deep relationships in existing contracts with private insurers and state and federal governments.
A strategic focus for Signify Health has always been driving more participation and success in value-based payment arrangements by integrating episodes of care into total cost of care models. Episodes of care help providers manage the cost of specialist care within total cost of care models. We believe these two payment models are synergistic and help maximize total savings and clinical outcomes. We view the highly anticipated CMS announcement last week about a refinement of the direct contracting model, now called ACO Realizing Equity, Access and Community Health or REACH as extremely favorable to a combined Signify-Caravan business model.
ACO REACH is tightly linked to achieving improvements in clinical outcomes by addressing social determinants of health and reducing inequities. The REACH approach is consistent with other ACO models and will extend the pathway for providers to assume total accountability for the quality and cost of their patient's care. Signify's in-home evaluations are specifically designed to collect social determinants of health data and enable the connection of patients to services. And together with Caravan, we believe we have the right set of capabilities to meet all of the model requirements set forth by CMS.
Models such as the Medicare Shared Savings Program and REACH create important stepping stones along the pathway for primary care practices, and we've recommended to CMS a model focused on chronic condition bundles that would complement MSSP and REACH and provide specialty providers a similar stepping stone to risks and rewards of advanced alternative payment models. Participation by all providers, primary care and specialty, is essential to achieving the innovation center's goal of all patients being aligned to an accountable relationship by 2030. We believe no organization is better suited to achieve CMS' goals than Signify Health. We look forward to a successful integration of Caravan Health into our operations and the ability to provide another complementary value-based model to our client base, while expanding our provider networks across both lines of business, episodes, and ACOs.
Turning to home and community services. 2021 was a great year for the business, and we believe the momentum we have will carry forward into 2022. The value of our in-home evaluations for both our customers and Medicare Advantage members remains meaningful. Customers have asked us to do more, and one of several ways we are meeting that demand is through our partnership program we announced in January.
We believe in connecting individuals to the right follow-on care, whether that's seeing a primary care physician or a behavioral health provider after the in-home visit or activating home care, transportation, or food assistance after an acute episode. Developing a partner ecosystem with solutions that connect care and drive alignment among providers is critical for us to deliver more integrated experience. For our partners, we provide an opportunity to accelerate innovation through a platform that is projected to engage more than 2 million people this year through our IHEs. Additionally, partners have an opportunity to participate in the episode of care programs we manage.
Our initial focus is on partner technologies and services that support behavioral health, remote patient monitoring, social determinants of health, member engagement, distribution channels to employers, and care optimization. We are proud to work with our partners who share a vision and are eager to see innovation resulting from this program. Given investor focus on possible regulatory scrutiny of in-home evaluation work since the OIG report last September, we would like to note that the recently released Medicare Advantage rules Part 1 and 2 contain no reference to in-home evaluations and no proposed changes that would negatively impact our business model. We also see the CMS request for comment on the collection of standardized social determinants data as a positive for our in-home evaluations.
We capture a range of social factors that can impact beneficiary health and are working with our MA plan clients to identify and address these types of needs for their members. The more social determinants data MA plans and CMS have, the better they are able to design programs to meet those needs. We continue to believe the value and independence of our comprehensive in-home evaluations for MA plans as a tailwind. We view our recent announcement, that Optum expanded their volume commitment with Signify through 2026, as another very positive sign that they and our broader client base are tapping Signify Health versus in-sourcing because they recognize and continue to recognize the value they derive from our services.
As a result, we believe that in-sourcing risk of volume is very low. To meet increasing IT volume demand, in 2021, we grew our network of physicians, nurse practitioners, and physician assistants to over 10,000. As we increase volumes in certain geographic areas, recruiting and credentialing can experience delays. But largely, we're not experiencing the same clinician labor issues being reported more broadly.
As we have often said, a significant benefit of our flexible network is that we credential our providers in multiple states, allowing us to deploy them wherever evaluation demand requires, including rural communities. The value of our logistics and routing technology included within our proprietary iPad application makes it easy for our clinicians to do what they value most: spend quality time with patients instead of dealing with administrative issues in a facility setting. Beyond clinicians, technologists are in high demand, and lead time to fill these rules have been extended with elevated compensation packages. To alleviate this challenge, we are opening a technology center in Ireland to recruit and retain technologists in a market plentiful with talent.
We have created an Irish legal entity, chosen an office location in Galway and have been recruiting for key roles. We expect to have a core team in place by this summer. We are excited about the opportunity to have an additional source of qualified talent to add to Signify. In closing, we are very pleased with our 2021 results and many of our accomplishments, which establish a strong foundation to expand upon as we move through 2022 and beyond.
When we filed for our IPO a little over a year ago, we outlined a bold vision to drive transformation of the U.S. healthcare system from fee-for-service to value-based care. Our 2021 performance and acquisition of Caravan Health have advanced us in realizing that vision. We simplified participation in highly complex payment programs and enable health plans and providers to successfully transition to value-based payments.
We provide comprehensive and highly valued in-home evaluations while facilitating services in and around the home to create synergies between our HCS and ECS businesses. With the addition of Caravan Health, we add further functionality, broader populations and innovation to our platform to drive increased value for our customers and patients. I will now turn the call over to Steve to walk you through our fourth quarter and 2021 financial results.
Steve Senneff -- President and Chief Financial Officer
Thank you, Kyle, and good morning, everyone. I'm happy to report on our fourth quarter and full year 2021 financial results. We had another record revenue and adjusted EBITDA year, delivering over 20%-plus growth, strong EBITDA performance, margin expansion, and significant cash generation. From a capital perspective, we raised more than 600 million in the successful IPO and, very quickly thereafter, executed on a refinancing that provided us with even more financial flexibility through better terms and a larger revolving line of credit to support our strategic plans.
Strength in our home and community services segment drove performance in the fourth quarter and for the year ended 2021, reflecting substantial expansion with clients, supporting our belief that clients continue to see significant value in the services that we provide. In episodes of care services, we continue to deliver strong savings to our partners across the BPCI-A program and our inaugural commercial clients, while ensuring individuals receive excellent care within their episodes. We continue to see the impact of COVID on skilled nursing facilities and in-patient rehab facility utilization due to the COVID waivers put into effect on the public health emergency. Additionally, the omicron spike in the fourth quarter continues to weigh on program size and savings rate, which is reflected in our 2022 guidance.
Over time, we do expect this impact to lessen. As I walk through the results, I'll be referring to the tables that appeared in the earnings press release issued yesterday as well as the earnings presentation posted on the events page. As you can see in Table 1, we had total revenue in the fourth quarter of $181.4 million, compared to 193.5 million in the same period last year. HCS revenue grew in the fourth quarter of 2021 by 5% to $156.2 million.
Total evaluation volume for the fourth quarter was approximately 473,000, including virtual evaluations. The fourth quarter reflected more typical seasonality, as we had been expecting and indicating over the course of 2021. Fourth quarter 2020 IHE volume reflected a COVID-related catch-up from earlier in the year, when, as previously indicated, in-home evaluations were temporarily paused and virtual evaluations were rolled out. We have great momentum in evaluation volume as we head into 2022.
Still on Table 1, fourth quarter 2021 ECS revenue was $25.2 million, as compared to $44.7 million in the same period last year. The decline was related to the adverse impact of COVID-19 on our program size and savings rate. The delta and omicron variants and CMS' automatic elimination of any episode with a COVID diagnosis, even though those patients were asymptomatic or only had mild symptoms and may have had no bearing on the success of the bundle, had an outsized impact on program size. We delivered significant savings for bundles in spite of the ongoing COVID impact, and we have the analytical tools and provider partnerships required to drive even more savings as COVID becomes less prevalent moving forward.
Moving to Table 4. Total company adjusted EBITDA for the fourth quarter was $40.2 million, compared to 38.9 million for the fourth quarter of 2020, reflecting the aforementioned HCS and ECS revenue puts and takes. Back to Table 1. Fourth quarter total net income was $32.4 million, compared to $0.7 million for the same period a year ago.
Our strong operating performance, in addition to the $36.7 million quarterly reevaluation of our equity appreciation right agreements or EARs, drove net income this quarter. We marked the EARs to market each quarter, and the credit in the quarter reflects the lower value of our stock price at year-end. As Kyle mentioned, we are very excited about the extension of Optum's volume commitments through 2026. In return for the incremental volume, we entered into a floor agreement with Optum that provides for a minimum dollar value in relation to the ultimate settlement of the EARs.
Optum must satisfy the relevant volume minimums over time in order to earn the floor. And as such, at year-end, we did not record a liability related to this instrument. We expect that the floor will become irrelevant as we continue to execute on our strategies and our progress is recognized in the stock price. There is an accounting requirement for the EARs to reduce the revenue based on the valuation of the floor when issued and over the term of the contract.
We will mark the floor to market going forward, and any changes in valuation will be reflected in the other income or expense line. For 2022, the revenue reduction related to the floor will be approximately a full percentage point reduction to reported revenue, but we exclude this impact in our calculation of adjusted EBITDA, resulting in no bottom line impact. Turning to full year results. 2021 was a banner year for Signify Health, as we grew the top line 27%, while delivering 37% adjusted EBITDA growth and 160 basis points of margin expansion.
Results for full year 2021 [Technical Difficulty] the continued overall strength in our home and community services segment with increasing demand across many clients driving strong IHE volume of 1.92 million for 2021. Virtual evaluations as a percentage of total IHEs totaled 17% in 2021, as compared to 36% in 2020. We anticipate that virtual evaluations as a percentage of the total will be slightly lower than 17% for the full year 2022. With client demand at record levels, we are projecting that IHE volume will be between 2.39 million and 2.42 million for the full year in 2022.
Episodes of care services results for 2021 reflect the COVID-19 impact on healthcare utilization, savings rate and discharge patterns reported in connection with the reconciliations received in June and December. As we exited 2021, we were on track for a $6 billion bundled payment program size run rate before COVID exclusions. Taking into account the fourth quarter spike in omicron and the uncertainty around future variants, we felt it was prudent to forecast additional COVID exclusions for 2022 and now estimate weighted average program size to grow from 2021 levels by between 500 million to $1 billion, depending on the impact of COVID. We expect the savings rate to return to our historical 25 to 50 basis points range of annual improvement during 2022.
With Caravan adding 10 months of revenue from savings generated from over 500,000 ACO lives, we expect the ECS segment to return to strong growth in 2022. Therefore, we are projecting ECS segment revenue, including Caravan, to grow in the mid-20% to low 30% range for the full year 2022. Moving on, as you can see in Table 2, we ended the year with $678.5 million in unrestricted cash, a substantial increase from 72.6 million a year ago, which reflects IPO proceeds of over $600 million. We funded the cash portion of our $190 million acquisition of Caravan Health on March 1, 2022, with cash on hand.
We ended 2021 with debt outstanding of $338.4 million and 173 million in capacity under our new revolving credit facility. Given our strong cash position at December 31, 2021, which exceeds our debt levels, we ended the period with negative net leverage. We have tremendous momentum going into 2022 and are providing the following revenue and adjusted EBITDA guidance ranges for 2022, which includes Caravan Health results for 10 months of ownership in 2022: total GAAP revenue in the range of 948 million to $971 million and total adjusted EBITDA in the range of 212 million to $222 million. We feel very good about our 2022 outlook and expect margin expansion of 25 to 70 basis points.
Quarterly revenue phasing in 2022 will have some slight differences from 2021, as the Caravan acquisition will only be included for 10 months of 2022, with only one month of actuals in the first quarter of 2022. As a result, total first quarter revenue, including Caravan, will represent 21 to 22% of the full year revenue. As we build the capacity for the full year record revenue, we expect the first quarter margin to be about 2 to 3 percentage points lower versus full year 2021 margin. Including Caravan, we expect the first half revenue to represent roughly 48 to 49% of full year 2022 revenue and the second half to represent about 51 to 52%.
We look forward to integrating Caravan Health into our operations to expand our product portfolio and value-based care payment programs. Now I'd like to turn the call back to Kyle for closing remarks.
Kyle Armbrester -- Chief Executive Officer
Thanks, Steve. I'd like to take this opportunity to thank our team at Signify for their positive and compassionate focus on the individuals we serve and all of their contributions to expanding and solidifying our business model in 2021. As mentioned at the beginning of the call, we have a long list of accomplishments of which to be proud. We welcome Caravan Health to the Signify team and look forward to their contributions to help health plans and providers close gaps in care, so that people can remain in their homes and enjoy more healthy, happy days.
I would also like to thank all of our stakeholders who are on this journey with us for the value we fully expect to generate over the long term. Now I'll turn the call over to the operator to take your questions. Operator?
Questions & Answers:
Operator
[Operator instructions]. And your first question comes from the line of Michael Cherny from BofA. Please, Michael, your line is now open.
Unknown speaker
Hi. This is Charlotte on for Mike. Thanks for taking my question. I just want to start out looking at the mix of IHEs and in-person versus virtual.
Could you provide any more color on that and then just the impact to margin?
Steve Senneff -- President and Chief Financial Officer
Yes. So thank you for your question. The impact -- so last year was 38% -- or two years ago, it was 38% last year. We cut that to about 17%.
So this year, for '22, we didn't really guide to it. I think it will be somewhere slightly less than 17%, but it was -- still given where we are, what we saw in the first quarter with some of the omicron spikes and stuff, we're still using virtual pretty heavily. So it's somewhere going to be slightly less than what we did in 2021. From a margins perspective, again, it's more of a revenue.
From a margin percent perspective, they're very similar in our costs profile. And so we don't think that's going to impact our margin percent in a significant way, and that's why we're confident in our 25 to 70 bps margin improvement for the year that we forecasted.
Unknown speaker
Great. And then just a follow-up. If you could provide any more color on the visibility into the ECS growth rebound.
Steve Senneff -- President and Chief Financial Officer
Yes. So look, Q4 was -- we got hit pretty hard with the omicron viruses. And as I said on the call, the challenge with that is that any episode that has a diagnosis of COVID, even if it's a domestic and nobody -- or very mild cases, we may have delivered incredible savings on that episode. But if it's a COVID diagnosis, it gets removed from our program size.
And so that's something that we're going to be working with CMS on as we move forward and hopefully get that removed at some point this year. And so it was a pretty big impact for us with the entire COVID in '21. We do feel and see that we will start to have some rebound there. We're not going back to -- as I said on the call, we don't feel it's prudent to go back to our $6 billion run rate.
We don't think it's going to be that big of a quick a return. We still have that ability, but it's -- with the carryover from what we saw in omicron, we're trying to be a little bit more conservative there and saying that we believe that 500 to 1 billion of program size will come back in 2022.
Unknown speaker
Great. Thank you.
Operator
Thank you. Your next question comes from the line of Anne Samuel from J.P. Morgan. Please, Anne, your line is now open.
Anne Samuel -- J.P. Morgan -- Analyst
Thanks so much. Your commentary on the REACH program was really encouraging around value-based care. I was just wondering how we should be thinking about what the read-throughs might be for the BPCI-A program and how you're thinking about that?
Kyle Armbrester -- Chief Executive Officer
Yes. Great. Good question. I would say just a few things.
One, CMS has been pretty consistent, and we just delivered a big white paper to them that we've been unpacking for several months with Harvard and Brandeis and UPenn, a bunch of thought leaders talking about the future of value-based care, which is, as they publicly said several times, integrating ACO in episodes of care. And what's important on the ACO front, obviously, gives you the broad-based population health, total cost of care, big spend under management, but lower overall savings rates potential, whereas the bundles or the episodes obviously attack the specialty care and the post-acute care in a more focused manner. And so bringing those two things together and working through attribution problems and building a more sustainable value-centric infrastructure to save the Medicare Trust, which is under extreme pressure. The CBO said in 2026, that might be insolvent.
And then CMS has said, by 2030, they want everyone in Medicare in a value-centric contract. And so what we view bringing episodes in ACO together and why we did the Caravan deal was to accelerate that, number one. With respect to REACH, we're very enthused for two main reasons. One, social determinants and thinking about health equity in a more holistic care model has been in our DNA since day one.
And so we are well positioned to bring a really differentiated approach to folks who are interested in participating in the REACH program. And number two, we've been planning and preparing for direct contracting/total cost of care movement with respect to our R&D and our expansion efforts. And so we think the Caravan acquisition positions us extremely well for the move into REACH. And frankly, we think that Signify is the best organization in the country to help CMS achieve its goals of moving more folks into -- or all folks in Medicare toward value-centric contracts by 2030.
Anne Samuel -- J.P. Morgan -- Analyst
That's really helpful. Thank you. And then maybe just one on Caravan. Can you help us understand, as we think about the contribution to your numbers this year and going forward, how should we be thinking about growth and margin expansion opportunity for that business over time?
Steve Senneff -- President and Chief Financial Officer
Yes. Look, we're excited. It's very much like the episodes business is from. As the savings rates improve over time, a lot of that's going to drop to the bottom line.
So we're excited about the margin expansion. It's one of the things that I had mentioned on the call. We think heading into 2023, we could potentially double the EBITDA contribution from Caravan for those exact reasons.
Anne Samuel -- J.P. Morgan -- Analyst
That's great. Thanks, guys.
Operator
Thank you. Your next question comes from Sarah James from Barclays. Please, Sarah, your line is now open.
Sarah James -- Barclays -- Analyst
Thank you. I wanted to clarify the comments you made earlier about not experiencing the same labor pressures as the rest of the industry. Does that mean that there's no step down in labor costs assumed in your '22 guide?
Kyle Armbrester -- Chief Executive Officer
Yes. We've -- so I'll clarify the first comment, and then I'll let Steve talk about the step down in cost point. We've been very fortunate. Our model is, one, distributed, right? So we have nationwide access.
We credential clinicians in multiple states, move them around when and where volume kind of dictates as we launch and expand our services. And so that flexibility model has been great for us. Like it's not -- folks can sign up for shifts when they want. They can move to different states through parts of the year.
So obviously, it's been a tailwind for us in the pandemic and brought us with a bunch of new talent, which is why we've been able to successfully scale and hit all the capacity constraints that we talked about, number one. Number two, clinicians are turning to us because we're allowing them to spend an hour of really high-quality time focused on care with individuals, right, and they're divorced from all of the administrative burden that they face so often if they're running their own practice or working in a bigger health system, dealing with claims, dealing with getting bills paid, dealing with scheduling, dealing with all the prior authorization workflow. With us, because of our technology suite, they wake up, have our iPad application that we've built out with all the logistics and routing technology that allows them to go throughout the day, spending time, an hour inside these homes with real quality time helping to diagnose folks and then connect them back to care. So we feel very good about that.
Steve, I'll let you talk about just COVID accounting for labor and the model maybe.
Steve Senneff -- President and Chief Financial Officer
Yes, so on the -- I get asked that a lot on the inflationary pressures. And so like every company, we have our challenges in that area. But I think as Kyle said, we've got a very flexible model that's allowed us to manage that. And it's a great part of the modeling.
So we have areas where there's significant demand and we'll do special incentives and things like that. But we haven't seen significant pressures that are impacting the P&L or anything that we can't manage. That's why we, again, are confident that we can do the 20 bps to 70 bps -- 25 to 70 bps or margin expansion despite any pressures. We also mentioned we've seen quite a bit of pressure on the technology side.
So one of the areas that we've been able to go and find more talent is opening up the Ireland office. So we expect that to be a big part of our go-forward opportunity as well in that area.
Sarah James -- Barclays -- Analyst
Great. And if I could, just one more. Can you give us a little insight on how you think about the adoption curve within your existing client base, maybe how you're seeing that trend from '21 to '22. And then as you think about moving out to CMS' goals in 2030, how much opportunity there is to capture more business within your existing client base?
Kyle Armbrester -- Chief Executive Officer
Yes, that's a great question. I would say that what drove us to do care analysis was our client base. We were listening to them. They mentioned both the payers in the health system, so that we need a multi-payer solution for me to go in and actually bridge this gap between the health systems and the health plan.
And they'd use Signify as a key enabler of that. And so I think there's substantial growth opportunity inside our existing client base. And frankly, it's where we're focused on initially, cross-selling and combining episodes, total cost of care and bringing that multi-payer approach. The issue, and what I mean with multi-payer, if you show up with a single-payer contract at a health system with its own set of guidelines and rules and reporting and data ingestion, you've got a percentage of panel issue, right? And you need somebody -- someone like a Signify that's going to connect the dots with all of our payer contracts, standardize a lot of that workflow, have consistent unified reporting and allow us to offer a more integrated approach on the data and analytics side for the providers that are actually engaging in care.
And so what we anticipate doing is bridging all of those strong ACO connection and relationship that Caravan's built out that takes a genuine total cost model, bringing in our episode infrastructure and then working with our plans to bring that multi-payer approach, where, obviously, CMS is the biggest payer and is the biggest participant in the bundled payments in the ACO program. Tying all that together and growing that into our existing very large, very scaled, very successful, very high NPS health plan business that we have on the in-home side is where we're going to be focused over the next several years.
Operator
Your next question comes from the line of Kevin Caliendo from UBS.
Kevin Caliendo -- UBS -- Analyst
So I want to understand a little bit your revenue-per-visit trends. Your virtual visits are going to be down. What are you assuming for price per IHE visit for 2022? Do you expect it to trend up? Trend down?
Steve Senneff -- President and Chief Financial Officer
Yes. It's going to trend up, although there's a couple of factors if you just aggregate it and look at it in total. It's going to say it's relatively flat. There's two things.
The EAR impact is going to hit the HCS side. And so that's going to impact that number. And we have a little bit of a mix impact as well in total, where some of our incredible volume that we're getting from -- coming from some clients with a slightly lower pricing. And so that's really, in an aggregate, you're going to see it's relatively flat.
But when you look at it by client, you're going to see that it continues to increase.
Kyle Armbrester -- Chief Executive Officer
And I would say --
Kevin Caliendo -- UBS -- Analyst
I'm sorry.
Kyle Armbrester -- Chief Executive Officer
Yes, I'm sorry, Kevin. Yes, the other two things that where you'll see certain phases in there, and we mentioned this on the last call, we've got more diagnostics and preventative service device revenue coming in as we've got more diversified devices going into the mix this year. And then a big initiative that we've been doing for several years that our clients are very focused on is returning to care. And so getting folks book back with a specialist or book back to their primary care doctors, sending all of that information over digitally, we see that as a big synergy with Caravan too because we'll have all that digital connectivity into these health systems.
So that return to care expansion that we've talked a lot about will be phased into that mix as well.
Kevin Caliendo -- UBS -- Analyst
All right. That's helpful. I'm guessing in the mix terms, that would that be United and sort of the reup with United, did that have an impact on this?
Steve Senneff -- President and Chief Financial Officer
There wasn't any price changes there, but obviously, there's a significant volume coming from there. And so again, our higher-volume clients are typically going to have slightly lower pricing, and so you're going to get some mix component in there.
Kevin Caliendo -- UBS -- Analyst
Fair enough. One quick follow-up. You had said you've been working with CMS to get the COVID diagnosis headwind removed. Any chance there's potential for retroactive adjustments?
Kyle Armbrester -- Chief Executive Officer
Yes. We're in open dialogue with them right now, not -- I don't think we're in a spot to comment on. But they certainly have, in the past, done retroactive on other things. They're very reasonable.
They're very data-centric. I would also mention, our health system clients are bringing this up, too. This isn't just us mentioning that the health system clients are -- they're rightfully frustrated. As Steve mentioned, if someone's in for an episode, they go through the procedure.
The health system does everything right. They manage the post-acute appropriately, they get them back to the home. And then on day 89 of the episode, they asymptomatically test positive with COVID, they get bounced out. That's super frustrating for a health system that's investing millions and millions of dollars to do genuine care redesign.
We're just at another phase of the pandemic, too. And I would say that CMS has been very reasonable, very data-centric, and a tremendous partner on this front. And so we're very hopeful, I should say, that we'll be able to move past the current kind of policy here in short order.
Kevin Caliendo -- UBS -- Analyst
Great. If I can ask one last quick one. I apologize for asking three. Is the cadence for this year different than you would normally expect? I mean we don't have a ton of history to go back on.
And I'm just wondering if there is anything specific around 2022 in terms of the cadence or if Caravan is impacting the cadence a little bit? Just any color on how we should think about that even going forward beyond 2022.
Steve Senneff -- President and Chief Financial Officer
When you're talking about cadence, are you talking about kind of the quarterly phasing?
Kevin Caliendo -- UBS -- Analyst
Yes, the quarterly cadence. I'm sorry, I didn't make it clear.
Steve Senneff -- President and Chief Financial Officer
Yes. So yes, as I mentioned in the call, so we think, obviously, because the way the Caravan is going to be more back half loaded because we're only going to have 10/12 of the year included, only one month in quarter one. So that's why it's a fairly typical -- you're going to have your ECS with Q2 and Q4 that are going to be the higher quarters, just because that's when we get the recon. Yes, I would say the HCS is relatively consistent.
It's going to be probably a little bit less. And that's why in total, we said first quarter, just to get everyone grounded, we think it's going to be 21 to 22% of the total. And then the first half, 48 to 49. And then we should be kind of back, Q4 will be our softest quarter just because of the way that the HCS volume typically takes place.
So other than -- in the past, we've had some of the dynamics changed because of the COVID impact. And so nothing really to call out on that this quarter out. We also called out that margin percent. If you look back at '19, '20, '21, '22 is not going to be any different.
Our margin percent is typically the lowest percent to start of the year, and that's just because we're ramping up and building all the capacity. So just wanted to call that out as well.
Kevin Caliendo -- UBS -- Analyst
That's really helpful. Thanks, guys.
Kyle Armbrester -- Chief Executive Officer
Yes. Great question. Thank you.
Operator
Thank you. Your next question comes from the line of Cindy Motz from Goldman Sachs. Please, Cindy, your line is now open.
Cindy Motz -- Goldman Sachs -- Analyst
Thanks. Congrats on the quarter. Thanks for taking my question. I just wanted to follow up a little bit on Kevin's question about the implied average revenue per visit.
So I'm getting like about $3.25 for this quarter. So it usually goes up first quarter. So, Steve, I was just wondering like do you expect the same kind of ramp that maybe we saw some '20 -- like fourth quarter '20 to first quarter 2021? And sort of maybe flat for the year overall? And then my second question was just on ECS. To get to that 20% revenue that you're talking about, it looks like we do have to look at more the higher end of the sort of average program size guidance as well as the -- the savings rate in line.
Am I right about that? Thanks.
Steve Senneff -- President and Chief Financial Officer
Yes, just to reiterate on the first question back on the HCS. It's going to be relatively flat, as I mentioned, if you just do the total calculations. If we looked at it by client, you're going to see this continues to raise. And again, it's really two things: the impact from the EAR, because that's just taking revenue straight out of HCS.
And it's a technical accounting. We back it out of EBITDA. So there's no impact there. And then the mix issue.
And it's really those two issues. There's no other dynamics going on there as other than us, as Kyle brought out, we continue to have additional penetration with our devices, with our new devices and more return to care. So we feel really good about the direction that, that's heading. And then on the ECS kind of range that we put there in the mid-20s to low 30s.
Look, we ran a bunch of different scenarios there. So just to make sure that we could have some flexibility on program size, on savings rate and folding in Caravan into the mix. So we feel comfortable where that's at now. And obviously, as the quarters move on, we'll report out and how things are trending.
Obviously, some of these things that we've been talking about on what happens with CMS and the announcements coming there could impact that as well. So we'll keep everyone well informed.
Cindy Motz -- Goldman Sachs -- Analyst
OK. That makes sense. And just if I could have one more follow-up. In terms of the EBITDA margins for the segments, obviously, HCS is doing pretty well and looks like it hit already like 30, 31% margins there, and ECS is certainly more challenging.
Do you expect the sort of ECS margin rate to improve over the next year? And then also to, I guess, HCS to remain stable? Or how do you see the margins, the segment margins going? Thanks.
Steve Senneff -- President and Chief Financial Officer
Yes. So look, on the ECS side, there's one thing that's -- in particular that's really driving that one. Obviously, as adding Caravan to the mix is nice, adding -- as the savings rates bounce back, we're going to see that margin improve because that's going to drop straight to the bottom line. But we are -- I'd like to call out that we still are making pretty significant investments in the commercial side.
And so that's one that we've been saying is like we're really going to start to see that in the '23, '24, '25 return on investment there. So that's one that we're going to have another year, I would call it, another year of investment on the ECS side, but we look to breakeven in '23.
Cindy Motz -- Goldman Sachs -- Analyst
OK. Thanks. Makes sense.
Operator
Thank you. Your next question comes from the line of Jessica Tassan from Piper Sandler. Please, Jessica, your line is now open.
Jessica Tassan -- Piper Sandler -- Analyst
Hi. Thanks for taking the questions. So I just wanted to ask one on Caravan. It's our understanding that they've consolidated from kind of 12 collaborative ACOs in 2020 to six in '22.
Can you just help us understand when and why that consolidation occurred? And then just how are you thinking about ensuring collaboration at the local level, given the geographic dispersion of some of these ACOs? Thanks.
Kyle Armbrester -- Chief Executive Officer
Yes, great question. That consolidation is one of the things that I was most excited about doing the deal. And frankly, it's one of the most innovative things that they've pulled together. And so what they, did in collapsing the 12 down to six to five, was pool more risk, right? And so it wasn't that they lost clients.
They were just taking the existing clients and putting them in these bigger collaborative ACOs. They are regionally centric, and there's a lot of engagement and participation and coordination in those regions where they all fit. And the purpose of the collaborative is just like an insurance company. As you take more lives on, you can shield yourself from downside risk.
And so any -- the wins of any one particular hospital health system in one particular quarter aren't going to impact the overall collaborative. And so when they go in it together, it provides a more stable, consistent, and balanced program. And frankly, it's -- the innovation that Caravan pulled off is helping to spread the total cost-of-care model throughout so much of the country. And so we were very enthusiastic about that innovative approach they pulled off, number one.
Number two, they have a big technology component of their business, and it was, again, one of the things that had us most excited called Caravan Coach. And it's an overlay pay sheet that sits inside the provider workflow that notifies and alerts them on the most urgent and emergent things they need to do. And each and every month, they are learning from surveillance throughout the entire ACO network that they're managing in all of the collaborative how to drive more efficiency, more effectiveness, and to drive a better provider and patient experience. And so they are actively in there coaching folks.
They're active in there doing change management inside the health systems on their technologies, how they enable and power that, but they very much have a strong account management and partnership model with these health systems to help drive performance. And that was very appealing to us. I've said many times that I think technology is absolutely necessary, but not sufficient to drive real impactful change in healthcare. And so what we're most excited about, and we've heard from several of the Caravan clients already, is Signify bringing that nationwide network of clinicians, bringing the post-acute experience, bringing the ability to do condition capture, which is big in the ACO market now.
We're going to turbocharge a lot of these resource-strapped health systems to perform even better inside their ACO contracts, which I think, one, will drive shared savings; but number two, will help us to expand and sell more health systems that are always looking for contracts with payers, too. And so Signify, again, can bring that multi-payer contract chassis. So we're very excited about the future and what we're going to be able to connect here. And the technology assets and the team that we picked up from Caravan, after a year-long diligence process inside the total cost-of-care space, we felt like was the absolute best fit for Signify, where CMS and our payer clients and our health item clients are going in the future.
Jessica Tassan -- Piper Sandler -- Analyst
That's really helpful. Just a quick follow-up. So it sounds like Signify plus Caravan are really well situated for ACO REACH. Interested if you expect that participation in ACO REACH to be in addition to or instead of participation in MSSPs? Thank you.
Kyle Armbrester -- Chief Executive Officer
Yes, good question. I think, number one, it's too early to tell. The announcement obviously just came out last week. I would say though, I expect some -- right now, Caravan has some clients in basic, some in enhanced.
Our first priority is to move as many over to enhanced as possible, more downside risk, better upside for us and the clients in the enhanced models were big fans of the enhanced model. Number two, we're focused obviously on shared savings this year and maximizing better patient outcomes while driving shared savings for the clients. Then I think we're going to go specifically client by client, both our episode clients today, the existing ACO clients and take a look at enhanced versus ACO REACH and what makes the most sense for them. And I don't think it's going to be the same for everybody.
There's a lot of nuance. Every health system is different. What we have is a great standardized platform that regardless of REACH or enhanced is going to be able to drive success for these folks. And so what we're diving in, we had our first session yesterday, I'm sorry, with the Caravan team going through all of their clients, our clients and starting to map out a strategy of how to best drive success for each of them.
And what I'm most excited about is ACO REACH gives us more optionality, right? It's getting another value-centric program that we're going to be able to expand and drive performance then, too. And that's great for the health system clients who are nuanced and each of them very different with respect to their skill set and their competencies and how they want to perform in value-based care.
Jessica Tassan -- Piper Sandler -- Analyst
Thanks again.
Operator
Thank you. [Operator instructions]. Your next question comes from George Hill from Deutsche Bank. Please, George, your line is now open.
George Hill -- Deutsche Bank -- Analyst
Yes. Good morning, Kyle. And thanks for taking the question. And my ACO REACH question was just asked, so I can put that on the back burner.
But I guess as it relates to the HCS segment, Kyle, I think there's still a lot of investor concern, I guess, about the long-term horizon of this business. And I think a lot of investors are looking for a regulatory clearing event to kind of like bless the long-term sustainability of the HCS business. I guess I'd like what you think -- I'd like to hear what you think about that. I kind of thought that the early rate notice from CMS talking about social determinants of health could have been that.
Just there do seem to be some investor questions about it. Would just kind of love to hear how you think about it and kind of what removes kind of that negative sentiment that I think is serving the capital valuation right now.
Kyle Armbrester -- Chief Executive Officer
Yes. Great question. So we've been in constant dialogue with CMS for years. There's been nothing, just to be clear, in the rate notice for years about -- years and years about anything to do with major overhauls to risk adjustment or any pressure on the in-home segment.
And so we deeply believe it's a big overreaction in the market, and couldn't agree more that it's an unnecessary overhang, number one. Number two, we've been in great conversations with CMS, where they've been direct with us saying, look, we are big supporters of in-homes. What we want to see is continued more follow-on care, more social determinants of health engagement like you all are doing. And so that road map of what we built into is exactly what they are doing.
And then number two, on the growth side, we've also been in talks with CMS, and we just got into the MSSP program about expanding in homes and their viability to other value-centric programs. And so we will be launching in-home services alongside those Caravan ACOs, right? And it's going to be a big differentiator of how we drive better shared savings, better condition capture, and better engagement for individuals in the same way that Signify has always been doing it, looking at the entire continuum of care from the homes, all the way to the facilities. And so I think it's a huge overreaction that folks think some massive changes that are coming to risk adjustment. None of our plan clients are concerned with it.
They've all been really engaged with us and focused on how to make sure that we're maximizing when we find a condition, doing something that's great for the individuals, whether it's a de novo diagnosis or getting them back to a specialist or closing out a few food and security. There is nothing more safer than getting to go into an individual's home and seeing the reality of what they're facing on a day-to-day basis. And CMS is thrilled that it is a free benefit that Medicare beneficiaries are getting as part of the Medicare Advantage program. And all of our conversations with CMS have been on how to expand that free benefit to other parts of the Medicare population.
As I just mentioned, we're going to be doing that through our MSSP engagement. But we're seeing no regulatory pressure at all and think it is a complete exaggeration that there's some bogeyman hiding out there that's going to overhaul this part of the business.
Steve Senneff -- President and Chief Financial Officer
Yes. The proof point really from our client's viewpoint is just the amount of volume that they continue to give us. Like Q4 was an incredible quarter for us, because that's usually a big drop off for us as we wind down the year. We still actually grew over 2020, which had the big COVID impact where we were doing a big percentage of our volume in Q4.
And then as everyone is seeing, we're guiding to about 2.4 million evaluations in 2022. So really getting a lot of momentum with our clients to drive more and more IHE volume.
Kyle Armbrester -- Chief Executive Officer
Yes. And to Steve's point, every single one of our clients is sitting down and asking how we can get into more homes and do more in the home. So that's across the board. And so there's no signs of this business slowing down.
If anything, again, we're having conversations about how to take this into managed Medicaid, commercial populations, other group accounts. They're including our services and our holistic care model and their bids through different group accounts. So we are very bullish on the continued growth and expansion of this business.
George Hill -- Deutsche Bank -- Analyst
It's great color. I think you guys framed the answer better than I framed the question, but I appreciate it.
Operator
Thank you. We currently have no further questions. I will hand over back to Kyle Armbrester for any final remarks.
Kyle Armbrester -- Chief Executive Officer
Great. Thank you, everybody, and thanks to the entire team for a great 2021. Thank you guys for participating in the call and your continued interest in Signify Health. If you have any additional questions, please reach out to Jennifer.
Have a great day.
Operator
[Operator signoff]
Duration: 57 minutes
Call participants:
Jennifer DiBerardino -- Head of Investor Relations
Kyle Armbrester -- Chief Executive Officer
Steve Senneff -- President and Chief Financial Officer
Unknown speaker
Anne Samuel -- J.P. Morgan -- Analyst
Sarah James -- Barclays -- Analyst
Kevin Caliendo -- UBS -- Analyst
Cindy Motz -- Goldman Sachs -- Analyst
Jessica Tassan -- Piper Sandler -- Analyst
George Hill -- Deutsche Bank -- Analyst