Image source: The Motley Fool.
Oak Street Health, Inc. (OSH)
Q2 2022 Earnings Call
Aug 03, 2022, 7:30 a.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Good morning, everybody, and welcome to today's Oak Street Health 2Q 2022 earnings conference call. My name is Drew, and I will be coordinating your call today. [Operator instructions] I'm now going to hand over to Sarah Cluck, head of investor relations to begin. Please go ahead.
Sarah Cluck -- Head of Investor Relations
Good morning, and thank you for joining us today. With me today are Mike Pykosz, chief executive officer, and Tim Cook, chief financial officer. Please be advised that today's conference call is being recorded. And the Oak Street Health press release, webcast link and the other related materials are available on the Investor Relations section of Oak Street Health's website.
Today's statements are made as of August 3 reflect management's view and expectations at this time and are subject to various risks, uncertainties and assumptions. In addition to historical information, certain statements made during today's call are forward-looking statements. Please refer to our 2021 annual report on Form 10-K and other periodic reports filed with the Securities and Exchange Commission, where you will see a discussion of certain risks, uncertainties and other important factors that could cause the company's actual results to differ materially from these statements. Certain statements made during this call include non-GAAP financial measures.
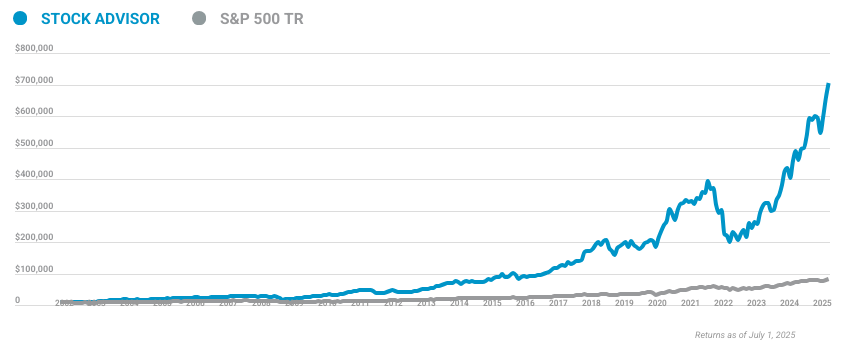
10 stocks we like better than Oak Street Health, Inc.
When our award-winning analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Oak Street Health, Inc. wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of July 27, 2022
These non-GAAP financial measures are in addition to and not a substitute or superior to measures of financial performance prepared in accordance with GAAP. Please refer to the appendix of our earnings release for a reconciliation of these non-GAAP financial measures to the most directly comparable GAAP measures. With that, I'll turn the call over to our CEO, Mike Pykosz. Mike?
Mike Pykosz -- Chief Executive Officer
Thank you, Sarah. Thank you, everyone, for joining us this morning. Joining me on today's call in addition to Sarah, Tim Cook, our chief financial officer. I want to first thank our team for the impact they make every day for our patients, hearing as well daily by the stories of our team members literally saving Oaktree patient lives.
We continue to be pleased with our performance in 2022 with Q2 performance above the top end of guidance range for revenue, at-risk patients and adjusted EBITDA. It remains a difficult operating environment in healthcare more broadly and is a testament to our team that we're able to continue to drive strong results. A key enabler of our success at Oak Street Health is how the components of our model, reinforce each other, create a platform where the whole is much greater than the sum of the parts. For example, our unmatched patient experience enables our B2C patient acquisition model.
In other words, patients join Oak Street because we often have concierge level patient experience in no additional costs. We are able to offer a differentiated patient experience because of the investment we make in our patients care, giving patients more time and easier access with our care teams while providing support navigating the healthcare system more broadly. We're able to make this investor in primary care because our care model keeps patients healthier, significantly improving health outcomes and lowering medical costs, leading to savings, which we retain through our value-based contracts. We're able to execute our care model because our focused de novo go-to-market approach, which enables us to consistently run a model specializing on older adults with operations staffing and custom built technology to meet our patients' needs.
And we're able to successfully execute our de novo go-to-market approach because our consumer-focused average model allows us to add patients without having to rely on buying or partner with existing physician groups. The reinforcing nature of our model provides a barrier to entry and a durable competitive advantage. Traditional primary care providers are not able to provide a differentiated care model or patient experience we do at Oak Street, as they're operating off an undifferentiated and less effective fee-for-service chassis. The components of our model also formed the basis of our focus at Oak Street.
As we discussed previously, we have four key objectives for the Oak Street, as we execute on our mission to rebuild healthcare -- as we execute on our mission to rebuild healthcare it should be. First, provide the best care anywhere; second, deliver unmatched patient experience; third, grow the number of patients we serve; and fourth, be the best place to work in healthcare. As proud as we are of our success to date, we also know that we continue to improve on all of these dimensions. And as we continue to invest in our model, we'll further our differentiation compared to traditional primary care and improve our center economics.
While COVID is obviously still with us. Over the last quarter, it is continuing to recede from the dominant challenge [Inaudible] to a persistent but manageable part of our everyday approach. This has allowed us to continue to focus on executing on all of our objectives. Prior to the pandemic, we had a consistent track record of improving our performance against all of our objectives, which led to a corresponding improvement in our unit economics.
We're excited to be in a stretch where our focus is consistently on the drivers of our long-term success as opposed to dealing with the day to day changes in our operating environment caused by the onset of the pandemic. We're optimistic we will be able to retain the focus on the drivers of our impact in center economics going forward. The operating environment in Q2 remains challenging across a number of dimensions. It is a very challenging in labor market.
We continue to navigate this environment, and our center opening plans remain on track. We are not expecting to be impacted by labor shortages. We are pleased with our performance in both the first half of the year overall and in the second quarter in particular. In the second quarter, we generated record revenue of $523.7 million in the quarter, exceeding the high end of our guidance range.
Our revenue growth continues to be driven by our organic B2C marketing approach. Medical claims expense trended in line with our expectations in the second quarter. Additionally, prior periods have developed favorably, positively contributing to Q2 EBITDA. Cost of care, which includes care team labor, marketing and corporate costs were all in line with expectations.
These factors all contribute to an adjusted EBITDA loss of $53.1 million for the quarter, which is $9.4 million favorable to the top end of our Q2 guidance. We achieved these results despite continued headwinds from direct costs from COVID hospitalizations and a negative retrospective trend adjustment by CMS to our direct contracting revenue. We believe this speaks to the effectiveness of our care model in driving improved patient outcomes and thereby significantly lowering third-party medical costs to our patients. Tim will cover the specifics on medical costs and others in shortly.
Our performance in the first half of the year continues to be in line with the projected center ramps for 2022 by cohort we shared earlier this year. As a reminder, our guidance this year is based on center level performance within that range. Performing favorably to our guidance for the first half of the year means we are achieving the center-level performance we set out. Continually performing along these center ramps going forward will create an outstanding financial return on the capital invested in new center development.
We are pleased with our performance in the first half of the year and what it means for our center level results. We are optimistic about the investments we're making continue to improve our platform and excited to continue on our journey to transform healthcare. With that, I'll turn it over to Tim to cover some more of the details regarding our financial performance in the second quarter.
Tim Cook -- Chief Financial Officer
Thank you, Mike, and good morning. As Mike shared, we were pleased with our second quarter as we delivered results above the high end of the guidance for at-risk patients, revenue and adjusted EBITDA. In terms of membership, our at-risk patient base, the key driver of our financial performance grew by 51% to 134,000 patients driven by our B2C marketing model and growth in the number of our centers. At the end of the first quarter, we operated 144 centers, an increase of 49 centers or 51% versus the 95 centers we operate at the end of the second quarter of 2021.
Capitated revenue of $516.1 million grew 49% year over year, driven by growth in our at-risk patient base. Capitated revenue in the second quarter of 2022 included a $3.7 million reduction related to prior periods due to the retrospective trend adjustments made by CMS as part of the direct contracting program, which were partially offset by favorable developments in Medicare Advantage. Adjusting for prior period impacts in 2022 and 2021, capitated revenue grew 56% year over year in the second quarter. Total revenue grew 48% year over year to $523.7 million.
Adjusting for prior period changes, total revenue grew 56% year over year in the second quarter. Our medical claims expense for the second quarter of 2022 of $391.6 million, representing growth of 39% compared to the second quarter of 2021. Medical claims expense in the second quarter of 2022 was lower by $10.9 million related to a reduction in prior period medical claims expense, as the cost for Q1 2022 have developed more favorably than our expectations. When adjusting for prior period changes in 2022 and 2021, medical claims expense grew 53% year over year in the second quarter, 200 basis points slower than our comparable capitated revenue growth.
COVID continues to impact our medical costs. We estimate that COVID represented $18 million in year-to-date medical claims expense. For new patient economics, we continue to see risk scores that are more consistent with historical periods, albeit not at pre-pandemic levels. We'll have a more complete sense of these risk scores when we receive the midyear updates later this quarter.
At this point, new patient medical costs appear better than 2021 levels, but also on a pre-pandemic levels. Given our performance to date, the impact of both COVID costs and new patient economics are consistent with our expectations included in our full year guidance. Our cost of care, excluding depreciation and amortization, was $98.9 million for the second quarter, an increase of 48% versus the prior year, driven by growth in the number of centers we operate and the number of team members supporting our significantly larger patient base. Sales and marketing expense was $42.6 million during the second quarter representing an increase of 65% year over year as we continue to invest in this area to support patient growth and a much larger footprint of centers.
Corporate, general, and administrative expense was $94.9 million in the second quarter, an increase of 28% year over year. Excluding stock-based compensation, which is partially inflated due to the treatment of our pre-IPO management equity plan, corporate, general and administrative expense grew 38% year over year. The majority of this year-over-year increase is related to an increase in headcount as for our growth. When factoring into prior period changes to revenue, we improved our corporate, general and administrative expense excluding stock-based compensation as a percent of our total revenue by approximately 110 basis points in Q2 2022 compared to Q2 2021, continuing our expected trend of declining corporate costs as a percent of revenue.
I will now discuss three non-GAAP financial metrics that we find useful in evaluating our financial performance. Patient contribution, which we define as capitated revenue less medical claims expense, grew 91% year over year to $124.5 million during the second quarter. Excluding the impact of prior period revenue and medical costs, patient contribution grew approximately 71% year over year. Platform contribution, which we define as total revenue less the sum of medical claims expense and cost of care excluding depreciation and amortization and stock-based compensation, was $34.1 million, an increase of 580% year over year.
Excluding the impact of prior period revenue and medical costs, platform contribution grew approximately 230% year over year. As an individual center matures, we would expect both platform contribution dollars and margins to expand as we leverage the fixed costs associated with our centers as well as improving our per patient economics over time. Adjusted EBITDA, which we calculate by adding depreciation and amortization, transaction and operating-related costs, onetime litigation costs, and stock-based compensation but excluding other income to net loss, was a loss of $53.1 million in the second quarter of 2022 compared to a loss of $53.5 million in the second quarter of 2021. Adjusted EBITDA benefited from the net prior period favorability in the quarter due to favorable development on Q1 medical costs.
We finished the second quarter with significant liquidity in the business, in line with our internal expectations. As of June 30, we held approximately $550 million in unrestricted cash and marketable securities. For the six months ended June 30, cash used by operating activities was $179 million, while our capital expenditures were $40 million, both of which are in line with our expectations. We expect over the course of the year that our adjusted EBITDA loss will approximate our uses of operating cash flow.
While those figures diverged in the first half of the year due to working capital seasonality, we expect them to converge over the second half of the year. Moving along to our 2022 financial outlook. We are increasing our full year guidance for at-risk patients and total revenue. We now expect year-end at-risk patients in the range of 155,000 to 158,500 patients and a total year -- the full year total revenue range of $2.125 billion to $2.145 billion.
We are reiterating our full year 2022 guidance for centers and adjusted EBITDA. While we are encouraged by our year-to-date performance, I'd highlight two factors impacting our adjusted EBITDA. The first is COVID, which remains an uncertainty, particularly in light of the case surges and the resulting medical cost experienced in Q4 of 2020 and Q4 of 2021 and the most recent rising cases. The second factor is the retrospective trend adjustment related to direct contracting mentioned earlier that negatively impacted revenue for year-to-date 2022.
We assume this adjustment, which reduced direct contracting revenue for all participants by approximately 7.5% and flowed entirely through to our adjusted EBITDA will continue for the remainder of the year. To provide more context, CMS set direct contracting PMPM rates for Q1 2022 based upon an estimated cost trend for direct contracting eligible patients. In May, CMS revised those PMPM rates based upon actual cost trend from Q1 2019 compared to Q1 2022. The actual cost trend was significantly lower than the estimated cost trend, resulting in the reduction in the PMPM rates, CMS pace.
This reduction was retroactively applied to January 1, 2022, for all direct contracting participants. CMS will revise our calculation each quarter and if the actual cost trend varies meaningfully from the estimated cost trend, CMS will adjust rates higher or lower as appropriate. Thus, as I said, while we are pleased with our first half results, medical cost development, in particular, we have reiterated our adjusted EBITDA range at a prudent in light of these exogenous uncertainties. For the third quarter of 2022, we are forecasting revenue in a range of $535 million to $540 million and an adjusted EBITDA loss of $90 million to $95 million.
We anticipate having 158 to 159 centers and an at-risk patient count of 143,500 to 144,500 including direct contracting patients at September 30, 2022. We remain optimistic about the momentum and the underlying trends we are seeing in the business. And with that, we will now open the call to questions. Operator?
Questions & Answers:
Operator
Thank you. [Operator instructions] Our first question today comes from Lisa Gill from J. P. Morgan.
Lisa, your line is now open.
Lisa Gill -- J.P. Morgan -- Analyst
Thanks very much. Good morning, and thank you for all the detail. I just want to go back to thinking about higher patient volumes and the impact on revenue and EBITDA. One of the things that stuck out to me is that you talked about the fact that risk scores are still not at pre-pandemic levels.
But while maintaining EBITDA and increasing revenue, I'm just curious as to how those -- the profitability of those new patients look? And then how much of this is being offset based on your comment around opex?
Mike Pykosz -- Chief Executive Officer
Yes. Thanks for the question. Yes, Tim said -- this is Mike to put the voice of name. As Tim said, we're between where we were in 2019 and where we were last year on new patient economics.
And so as we shared at the beginning of the year, that was a key factor that we wanted to get more experience with as we saw how and things return to normal from what was a pretty abnormal 2020, 2021 from a patient economics perspective. And so we're pleased to see them returning more to the normal side than from where they were before. And I feel comfortable with this level of economics. And I think that, again, to your point, with our business is always puts and takes around new patients and existing patients and different trends.
And so I think we were pleased with the performance in the first half of the year that without new patients coming in, kind of to the same level there in 2019, we're still ahead of the high end of our ranges on EBITDA. And that speaks to the overall performance over across all of our patients.
Lisa Gill -- J.P. Morgan -- Analyst
And Mike, as we think about the cost side, you made the comment that you weren't having issues with hiring people for new facilities, but are you seeing an elevated cost when we think about labor cost or even on the supply side as we've seen inflationary costs across the board, your one company that didn't call that out specifically. I'm just curious if you're seeing an impact there.
Mike Pykosz -- Chief Executive Officer
Yes. It's still, I talked about a little bit of a very tight labor market. And labor is a relatively small portion of our total cost structure. So we spent a little over 10% of our revenue on our care team labor.
So it's very different than a big hospital system or a home health company or one of those companies that are obviously north of 50%. And so selectively, we'll revisit compensation for roles. And we've always done that, and we'll continue to do that to make sure that we're competitive and attracting great people to our team and retaining great people on our team. But because labor is a relatively small part of our of our cost structure, and we think any investments we make in our team will be able to offset with kind of over performance other places.
And there's nothing better in our mind than investing in our team and paying for those investments like keeping our patients helping out the hospital.
Lisa Gill -- J.P. Morgan -- Analyst
Great. Thanks for the comments.
Operator
Our next question today comes from Ryan Daniels -- sorry, apologies, from William Blair. Your line is now open.
Ryan Daniels -- William Blair and Company -- Analyst
Yeah. Thanks for taking the questions. Mike, maybe a big picture one for you. Just in regards to the M&A activity we've seen in the space.
I'm curious if Walmart is a retail partner has amplified their desire to expand clinics and wanted to get an update from you about the performance of your Walmart clinics, which have been in operation now.
Mike Pykosz -- Chief Executive Officer
Yes. Thanks for the question, Ryan. We certainly see the same headlines. From our perspective, one thing we really love about our model and the market one is, it's just an absolutely massive market opportunity for us [Inaudible].
And we talked about this before, but we look at where we are successful today with the demographic patients and the type of markets we're stressful today, and that creates a market opportunity of 30 million Medicare patients, which will require 10,000 centers. We have a fraction of that today. So what that means is we can really keep doing what we do over and over again without having to look for adjacencies or new opportunities and drive sustained growth for a decade and beyond. So again, we really feel like we're a fortunate place of having a very proven profitable model and a huge growth trajectory.
That said, as we talked about when we went to the partnership, we were intrigued by the partnership with Walmart because we can run the same care model inside a Walmart center versus just inside an Oak Street Center. And so we should be able to generate same patient economics. And so the other key driver of results right how many patients we're serving. And the reality is, in most Walmart, a huge percentage of people in the community, including all their adults are shopping to Walmart, it tends to be a similar demographic to what we serve.
And so we thought that was a great way to kind of be in a convenient location and get to know a lot of people. And I would say the results are still TBD on the pile. I know it's been around for a bit of time. But again, the bar is not, do they perform like an Oak Street Center, right? We can open up as many Oak Street Center as we want.
What -- and the bar is, are they performing significantly better than the Oak Street Center to kind of support a partnership, which obviously will be more complicated to doing yourself. And in hindsight, it was a not an ideal time to try that type of partnership. If you remember, we opened those centers up really in the high of the pandemic. And people weren't necessarily excited about someone walking up to them when they walked into the store and started up a conversation with that, right? And generally the mindset was kind of stay out of my bubble.
And so I think that we still want to see the results play out a bit longer to -- from our perspective, just say, "hey, is this something that we'll make a meaningful enough difference." I still think the -- kind of the rationale behind it, I think saw a lot of merit again. One of the key drivers is bringing in patients. And we've seen over and over again, the more people we meet, the more people we can kind of show our centers to the more we'll join his patients. So I think the logic behind it still makes sense from our perspective.
I think just seeing that logic actually play out the results and so kind of TBD.
Ryan Daniels -- William Blair and Company -- Analyst
OK. That's very helpful. And then going into another partnership and maybe a broader question, I wanted to get an update on AARP. And then more broadly, just your marketing initiatives and kind of how you've settled in on a digital versus community outreach model now that we've effectively returned to normalcy, have you been able to the cadence of spending and what kind of returns are you seeing from the various media channels for customer acquisition? Thanks, guys.
Mike Pykosz -- Chief Executive Officer
Yes, Ryan. Thanks for the question on that one. We definitely settle into all of the above approach on patient acquisition. The way we think about it is how can we bring patients in under kind of our cost per acquisition target and generate a CAC:LTV ratio that we want to generate, which is -- I think shared before, is kind of north of what you would see in most kind of tech recurring revenue businesses.
So we really love the return on the investment we're getting in our marketing. And so something like digital and Facebook and Google and those types of channels. As long as we're generate means below our kind of bid numbers, which we have done, we know that we'll bring on patients at a really strong cost of acquisition, we'll keep doing that, right? At the same time, as long as our field-based teams are bringing in a minimal number of patients per kind of outreach executive on average, right, that will generate the cost of acquisition we need. And we'll continue to look for opportunities to optimize both of those channels, right, to the extent we can increase productivity of our field team.
That'll just bring in more patients at a very similar cost, which again would have both improved our CAC, but also more importantly, improve our unit economics. And the same thing on the central channels. And so for us, it's not about kind of finding a balance between the channels. For us, it's about kind of maximizing the number of patients within each channel under our CAC threshold.
And again, I think there's opportunities to do both. If the ARP -- specifically I think -- ARP, I think, is an enabler, and I think will be a long-term tailwind on both of those dimensions, right? Because it is the most trusted brand for older adults. It's in probably well-known brand. And we've definitely identified.
One of our challenges is people are taught in life if something is too good to be true than it is, right? And no one has added the correlator. Something that's going to be true that it is except for Oak Street Health, which is actually real. It doesn't roll off the time quite as much. And so our goal at ARP is to have a partner that is very trusted that kind of works with us and it's exclusive, obviously, nationally with Oak Street.
And so we think that will be a long-term competitive advantage. And to your point, we continue to ramp up more marketing channels and to get more and more work what we do, the more and more people hear about ARP, the more benefit we'll get from that brand.
Operator
Our next question comes from Justin Lake from Wolfe Research. Your line is now open.
Justin Lake -- Wolfe Research -- Analyst
Thanks. Good morning. I wanted to follow up, Tim, on your comments around direct contracting. Just want to make sure I heard that right.
You said a 7.5% change in cost trend in terms of what CMS is reimbursing on. First, is that correct? And then second, given the economics, I think you were saying we're going to be breakeven, give or take this year, maybe slightly profitable. What does that do to the economics in your mind to DCD from a margin perspective this year?
Tim Cook -- Chief Financial Officer
Thanks, Justin. So you did hear me correct that the change in revenue was 7.5%. And just to give you some more context there, coming into Q1 of this year, CMS estimated that the total trend from 2019 to 2022 would be 16%, not annualized, of course, just 16%. What they calculated based upon Q1 expenditures and again, it's just one quarter's worth of data was only 7%.
And it's not as simple as subtracting as you actually get the ratio of them. And when you do that math, you get to about 7.5% reduction. We will see as the year rolls on, whether or not Q1 was indicative of full year medical costs. Said another way, Q1 costs may have been lower for a variety of reasons, which impacted that calculus for Q1, but as we see claims out of Q2 and Q3, we will see how those -- how that does or does not change that -- the retrospective trend adjustment.
On the impact to our patient base, the good news theoretically is if you're getting paid less on a revenue perspective, that should mean your costs are lower. And we did see -- as you can tell from our release in Q1, we did see some benefit both in the MA book and direct contracting book for medical costs, and we still run a good margin on those patients. So they are not -- our direct contracting patients are better than breakeven so we do generate economics more consistent with our MA book. I know it's different than other participants, but just as, again, a difference in our approach to caring for patients and I think the others have.
So doesn't -- it obviously impacts our expectations on full year economics. We will see how cost trend for direct contracting patients in all of our patients, frankly, for the remainder of the year. And that will be obviously a key driver in where we end up in the range.
Justin Lake -- Wolfe Research -- Analyst
OK. And just to be clear, in the first quarter, even with that 7.5% reduction, you're saying that given what you know about claims, you were still slightly profitable on those numbers?
Mike Pykosz -- Chief Executive Officer
Yes, Justin, not slightly. I mean our direct contracting performance is, as we shared before, pretty consistent with our MA performance. So yes, obviously, we have a 7.5% reduction in what you thought revenue is going to be. That does impact the profitability, though, Tim's point, at least for Q1, bad costs are coming in favorably as well, which helps offset it.
We're not assuming that favor really continues into Q2 from a bad costs perspective. Obviously, we hope it does. And so again, I think I would reiterate this today. Again, it is a profitable book for us and it wasn't slightly profit.
I think others have had less success in the program. We've seen similar levels of profitability to MA in the program. And so even with this revenue reduction, if it continues throughout the year, we feel good about our participation in the program. And I think I want to reiterate what Tim said, I mean, Medicare saw a much lower trend than they expected Q1 over Q1.
We're assuming that continues. But if it doesn't continue, right, they revise it retrospectively every quarter, right? So we're still -- there's still three quarters left of more data. So I want to make sure that's clear that we feel like we're managing it appropriately, but a lot of you play out.
Operator
Our next question comes from Jamie Perse from Goldman Sachs. Go ahead, Jamie.
Jamie Perse -- Goldman Sachs -- Analyst
Hey. Good morning, guys. I wanted to spend a minute just on the guidance. Your range this year -- to start the year is built around two key variables, COVID trend; and the new patient economics.
Can you give us a sense of where you are in the range for those two variables? And what you're assuming in the updated guidance for the second half?
Tim Cook -- Chief Financial Officer
Yes. So Jamie, for COVID costs, as I mentioned, we were -- this is Tim. Thanks for the question. We were $18 million year to date.
Last year, our total COVID costs were roughly about $40 million, probably better to think about on a PMPM basis last year. It was about $40 PMPM, the number of months. This year -- I don't think that we've disclosed a number of months, but we're talking -- it's much lower, obviously, just given where -- if you take it ratably you know that we've grown our patients a fair bit. So we are seeing lower COVID costs all in.
That being said, if you remember from our guidance, we had -- the low end of our guidance was consistent with 2021 performance, which would have been $40 PMPM. High end was sort of halfway between 2021 and 2019, so call it $20 PMPM. So we're trending in the range of that on COVID costs. On new patient economics, I would say it's pretty comparable on the COVID side, obviously unrelated, but just from a general direction perspective, kind of in line with the midpoint -- as you can tell, given our performance thus far, right, midpoint, the upper half of our range.
Jamie Perse -- Goldman Sachs -- Analyst
OK. And in the second quarter, you guys beat your internal EBITDA expectations adjusting for some of the out-of-period changes, you mentioned that MLRs were in line with expectations. So it sounds like some of that came from items further down the P&L. Can you just give us a sense of where that occurred, if it's sustainable, if you're getting leverage somewhere faster than expected? Or if it was more about timing?
Tim Cook -- Chief Financial Officer
Sure. So there was -- there obviously was the benefit of the Q1 medical costs and say, Q2, in line with our expectations to your point. The incremental benefit above and beyond that is just conservatism within our cost forecasting. So the biggest cost we have is labor.
And this market is obviously -- again, as we discussed, we're not immune to the labor challenges. We have -- we are more than sufficiently staffed in our business, but we probably haven't ramped hiring as much as we otherwise would a normal year, just given the competitive dynamics in the marketplace. And there's probably a little bit of tailwind there, frankly, not tremendous, but some benefit there and then timing of new centers is obviously going to impact that. So just really a combination of those two dynamics.
Operator
Our next question comes from Gary Taylor from Cowen. Your line is now open, Gary.
Gary Taylor -- Cowen and Company -- Analyst
Hey. Good morning. Just want to go back to direct contracting for a second, make sure I understand everything. If we take the $3.7 million, I think you said, divide that by 7.5%, it's like $49 million.
So did you say that was -- it would imply like $49 million of revenue. Do you say this went all the way back to the beginning of direct contracting back in April '21. So with the trailing 12 that adjustment impacted this quarter?
Tim Cook -- Chief Financial Officer
Gary, it's Tim. Two things on that. No, it goes back to January 1 of this year. So they'll revise it in May for Q1.
We'll get another notice here at some point late in August that will -- if to the extent that their updated math suggests that there's a further deviation, they will also revise it all the way back to January 1. So this is -- the direct contract is a bit different than MA. And MA, they set rates to the rate notice. Those rates are set and so for the following year.
There is a similar component or dynamic within direct contracts where they do that. But during the course of the year, they retrospectively look back and assess that rate, which is not ideal from our perspective because it can create the volatility we're talking about, but that's just the realities of the program. On the $3.7 million -- remember, that is the out-of-period component, so that would be one quarter. But I think you're thinking about it roughly correct.
There was some offset from our MA book. So the actual impact was probably a little bit larger than under recontracting, but from a net basis, you're thinking about it correct.
Gary Taylor -- Cowen and Company -- Analyst
OK. And when do you reconcile the first full year of direct contracting? And just -- I think that's in the 3Q. But I just wanted to understand when I think you're carrying both receivables and payables related to contracting. So my thought is when you reconcile both of those dollar amounts come down.
So I just wanted to maybe sort of front run for the Street a little bit, how that might look like so people aren't surprised or confused when we see that 3Q balance sheet.
Tim Cook -- Chief Financial Officer
Sure. So Gary, we will settle 2021 in Q3 of this year. I think we've already received the final -- not just the final statement, but sort of the 2021 readout and cash gets settled in Q3. So our working capital follows cash settlement and to your point.
So in Q3, we would expect the receivables related to 2021 direct contracting and the payables on the medical cost side to both release from the balance sheet. And obviously, the net margin is the difference, and then we'll have an incremental accrual for Q3, right, as you'd expect. But there will be an impact because you're releasing nine months and you're accruing -- or excuse me, yes, nine months in accruing an incremental 3% for Q3.
Operator
Our next question comes from Jessica Tassan from Piper Sandler. Your line is now open.
Jessica Tassan -- Piper Sandler -- Analyst
Thanks so much for taking the question. So I was just hoping to follow up on two things. First off, on marketing, can you just discuss kind of the extent to which B2C marketing has recovered? Where we're even at baseline pre-pandemic? And just to what extent have the cadence of those events recovered at each of your centers?
Mike Pykosz -- Chief Executive Officer
Yes. Thanks for the question, Jess. We are still between where we were last year and where we were in 2019 as far as the number of events per center, but we keep ramping that up. So again, all of our marketing release, the best, is really B2C.
So we always think about central channels such as digital marketing and kind of more traditional marketing approaches. And that is ongoing and something that we had increasing success with since the pandemic and ready to develop those capabilities. And then obviously, we have our kind of more traditional community-based average model. We are ramping up the activities in the community, but we were really clicking on all cylinders in 2019, and a lot of our relationships took years to develop.
And the reality is, for a lot of groups that hope seniors, they stopped doing it in 2020. They didn't do it in 2021. Some senior living facilities haven't hired back their -- that coordinator that they had prior. So there are a lot of changes to work through.
And then when they hire those people back, we need to go for that relationship and educate the groups about Oak Street and then get access and run events. And so we feel like moving in the right direction. We're still guardedly optimistic that we'll get the community out back to Oak in 2019 over time. But it's never going to be a step function up because it really is about kind of every center and every team member forming relationships, rebuilding relationships, getting the events set up.
And then once you have the events set up, you meet people, it takes multiple interactions, generally, some of the schedule a visit. And then a month after the visit, they'll finally flow through to our at-risk membership. So again, it's about building the pipelines and kind of keep taking incremental steps forward, which again, we we're guardedly optimistic about. And we're kind of performing from an average perspective where are we expected to coming into the year.
But I think we still feel there's a lot of upside from where we formed today. We're going to execute to get that upside. It will happen overnight.
Jessica Tassan -- Piper Sandler -- Analyst
Got it. That's helpful. Thank you. And then just on direct contracting, do you guys feel like you're effectively kind of confined with certain medical cost ratio just due to the quarterly reconciliation.
And then is there anything about ACO REACH that would make that program more attractive or just have more margin or margin potential relative to direct contracting. Thanks again.
Tim Cook -- Chief Financial Officer
Sure. Sarah -- Jessica, sorry -- I just want to remind myself not the call you Sarah [Inaudible] Jessica, so I apologize, and I'm looking at Sarah again. So I got to disassociate you to. Sorry, Jessica.
It's Tim. On the MLR front, for direct contracting patients, no, I'd say the way that revenue is reset is based upon overall cost trend in the broader market. And we hope, given -- or we expect, given the strength of our platform that we should be able to manage trend better than the overall market. So we should still be able to expand margins.
And they're -- I mean, obviously, there's going to be an impact to profitability, but we still feel as though we can manage these patients to a better MLR than the market at large. So that would be point one on that component. Sorry, can you just, Jessica, ask your second question again? Sorry, ACO REACH and the dynamics there. The simple answer is, we believe that the changes as part of ACO REACH will be neutral to favorable to Oak Street.
There's a lot to learn about changes they'll make to the risk score cap and a few other dynamics. From what we do know, which the changes to the discount applied to the program in the outer years is favorable. Previously, that discount would grow 5% over time. Now it will, I think, cap out at 3.5%.
So that's favorable relative to where it was before. I believe there may have been some adjustments to the quality withhold. That being -- so those are net positive. We will see what changes, if any, happen on the risk score cap and how that may or may not impact us.
So a lot to learn those changes start to come in, I want to say, 2024 and 2025. So we've got some time before they're a reality one. And then two, we will -- we just need to see some more information before we can better assess what the impact is going to be to our business.
Operator
Our next question comes from Elizabeth Anderson from Evercore Capital. Your line is now open.
Elizabeth Anderson -- Evercore ISI -- Analyst
Hi, guys. Thanks so much for the question. I was wondering if you could talk about some of the drivers in cost of care. Obviously, that's come in a little bit better than our expectations so far this year, but the implied guidance in the back half of the year has a bit of a step-up.
I mean I know your patients are ramping, you're opening more centers, but you can talk about the puts and takes on that line. That would be super helpful.
Mike Pykosz -- Chief Executive Officer
Yes. I mean cost of care is honestly pretty straightforward from a budgeting and projection perspective from us. When we open a center, we have a standard staffing that a new center has. And as a center ramps patients between a brand-new center with no patients all the way to a center that is full, we have a standard ramp of when we add certain team members, right? So you add your staffing care team at a certain time, your third care team, your fourth care team based on patients.
So really, the two drivers of our direct cost of care is; one, rent and kind of everything associated with center outside of labor and labor. And we add labor at the same ratio across all of our centers. And so those ratios and kind of how we hire really hasn't changed from the first half through the second half of the year. So to the extent, we're growing faster.
We'll add care team members faster, but obviously, that's a good thing for the business overall. And the opposite is true. And we really do it at center level, not at the company level.
Elizabeth Anderson -- Evercore ISI -- Analyst
Got it. That makes sense. Thank you.
Operator
Our next question comes from Michael Ray from Morgan Stanley. Your line is now open.
Michael Ha -- Morgan Stanley -- Analyst
This is Michael Ha. Thanks for the question. I just wanted to revisit Gary's question on cash flow and working cap. I know you had mentioned net working cap should converge in the back half of the year.
And with direct contracting, there seems to be some new balance sheet dynamics at play for 3Q, but just taking a step back, it looks like net working cap historically in 2Q is positive, but this quarter it's down $50 million year to date, it's down $100 million. Can you talk about what's driving this unusual negative net working cap? Is it DC related or maybe some other payer timing-related dynamic and well that you've been out in the back half?
Tim Cook -- Chief Financial Officer
Yes. So thanks, Mike. This is Tim. You're correct.
Direct contracting is a big contributor there, just given that we continue to carry all of the 2021 profitability related to the program on the balance sheet. We would expect that to release in Q3, as I mentioned, and that would be one of the tailwinds to cash flow or operating cash flow in the second half of the year. The other is related to the timing of full year midyear payments. And again, as we cut the quarter off at June 30, the timing of those things and -- or excuse me, full year midyear and just general plan settlements, those timings of those, as we discussed, can fall either pre or post the quarter and obviously because of the balance sheet at June 30.
So there's nothing abnormal from our minds. We will see how things develop in second half year. But as we said, generally speaking, adjusted EBITDA, operating cash flow moved pretty consistently together and -- for the full year. And we would expect to see that converge in the latter half of the year.
One thing I'd just remind folks is the mid-year payments come in Q3. So that is a relatively large source of cash that we don't have in the first half of the year. So that's another big tailwind in the second half of the year and one of the things that drives the adjusted EBITDA loss to mirror operating -- use of operating cash flow.
Mike Pykosz -- Chief Executive Officer
I mean just build on that, if you look at 2020, 2021 and then obviously for us years before being public, generally, EBITDA has been a good approximation of operating capital. Actually, EBITDA -- operating capital has been slightly more favorable in prior years than EBITDA. And we have the same dynamics in the first half year, the second half of year in those years. So we don't feel there's anything different this year.
And keep in mind, in 2021, cash and operating -- sorry, EBITDA and operating cash flows were still had that same dynamic. And we've carried the 2021 EBITDA. We haven't got the cash yet, right? So I think that there's no differences in timing that we see. I think it's just a question of always the first half of the year is from cash flow perspective, the second half of the year is better and it nets out.
So we expect that dynamic to continue. There's nothing abnormal so far about this year that we've seen.
Michael Ha -- Morgan Stanley -- Analyst
Got it. Thank you for that. Just one more on my end and a bit of a high level one. As I think about kind of future upside leverage for Oak Street.
And I understand the past, you've communicated that your standards at maturity could see at-risk patient occupancy around 70%, 75%. But I think that was before -- direct contracting before the new patient outreach playbook you implemented. Just looking forward, how should we think about your at-risk patient occupancy levels ramping up in your centers?
Mike Pykosz -- Chief Executive Officer
Yes. I mean I think that that you're referencing was we shared in January, I believe, that centers that we're nearing capacity, we're making $8 million in kind of 4-wall contribution. And those centers kind of aggregate or, I think, on average about 75% full, right? That was -- and so those ones are still growing, right? We'll keep growing them up. Theoretically, over time, all of our tenants will get to 100% full of at-risk patients.
We recognize that that is a kind of a ceiling, right? We're never going to put more patients on to a care team. We don't want to lower the experience or quality of care. We can't add more care teams in our exam rooms for them to work out of. So that's kind of -- that kind of comes your maximum, right? And so we have a couple of centers there, but -- and others will get there, but we'll keep adding patients until we do get there.
So I don't know -- I think certainly there's upside to the extent that if we keep performing the same level on a patient contribution perspective and fill all of our centers up, then we'll obviously have more opportunity to improve the kind of mature four-wall margins of our centers. And then obviously, one of our -- I think our biggest opportunities for kind of upside is pulling ourselves up faster, right? So instead of taking kind of six, seven years to get to those levels, let's get there in a couple of years, right? So that is why I think we are so focused on the sales and marketing approach. Again, we select a number of levers to pull, including getting our community marketing back toward 2019, continuing to improve our brand, leveraging the ARP partnership, etc. But we feel like that's a huge opportunity for us both to get the kind of a handful of centers that are going to near capacity to full capacity, but also get the rest of our centers to get there faster.
Operator
Our next question comes from Sandy Draper from Guggenheim. Your line is now open.
Sandy Draper -- Guggenheim Partners -- Analyst
Thanks very much. Most of my questions have been asked and answered, so I really appreciate all the detail. Just one quick question and then a follow-up on ACO REACH. Can you just remind me, and I apologize if this is -- you've gone over this multiple times.
Just what the exposure is to DC, whether we think about it in terms of lives, revenue, EBITDA, but just trying to think about that. And then if I heard you correctly, on ACO REACH, is it too early to call whether the same type of quarterly revision is going to happen under that model? Or is it -- we just don't know the exact details? Thanks.
Mike Pykosz -- Chief Executive Officer
Yes, Sandy. Thanks for the question. On your first one, we have released a breakdown between direct contact and MA risk lives. I think we have shared this.
The majority of at-risk lives are Medicare Advantage, right? And that's just based on the demographic patients we serve and the plan choice they make, most of them have chosen Medicare Advantage. There's also some dynamics where not all of our traditional Medicare patients flow through the direct contracting right away, keeping that number a bit lower. So still the Medicare Advantage is a big driver of our at-risk business. Although, obviously, we -- as I shared earlier, we really like the economics of the direct contracting in the ACO REACH program.
In our understanding, and obviously, as Tim said earlier, they're still releasing all the details on ACO REACH, but I don't -- we don't expect any change to this quarterly process. And what I want to make sure we're pointing out -- because obviously, this is a big factor in new to the market. It's not a situation where they do one quarterly reconciliation and it changes, right? And so what's always going to happen is you're going to have the least data for what the actual trend is going to be after Q1 because you have one quarter over one quarter. So they're comparing first quarter 2019 to first quarter 2022.
And obviously, in their analysis, which keep in mind, Q1 actually still isn't fully complete for CMS when they did, estimate what Q1 2022 will be. So there's a lot of -- there's a lot of estimates going on there. In that estimate, trend did come in significantly lower than they expected and frankly significantly lower than we see in medical cost trend historically, right? That would be historically low Medicare trend. And if it persists, and we are assuming in our financials, how we book the first half of the year and how we're thinking about guidance that it does persist and persist, then there is lower revenue for the program.
As we said, we'll still be profitable in the program even with that lower revenue. And in Q1, we did see lower medical costs across the board in Q1. We're not necessarily assuming that in Q2, as we go Q2 nor are we assuming that -- can use it in the back half of the year. So they will double the data points that they face that trend off of when they release the update in a couple of weeks.
Then they will update it again after Q3, and they'll update it again after the end of the year. So when they actually release the final, they'll quadruple the number of data points they have today. So again, we want to make sure we're being prudent and assuming that this revenue decrease maintained and not necessarily taking also the corresponding benefit in medical cost reduction, it would be a very low annualized trend in Medicare. It's possible -- it's certainly possible that it persists for the year.
It's also possible that it goes back. In other ways, it is a more accurate way than what they do for Medicare Advantage. For Medicare Advantage, they -- it is easier as a corporate company, the way they do Medicare Advantage because you know what your rates are going to be coming into the year. But if it ends up being a higher trend year then you needed, I think the lower trend here you get a benefit, right? This way, actually, what happens in reality is kind of how you're graded.
So in some ways, it's actually a more accurate way to do it, albeit after one quarter over one quarter of data. I think it creates a little bit more variability. And given this is the first time we're all doing it, I think we want to be prudent in how we think about that variability.
Sandy Draper -- Guggenheim Partners -- Analyst
Thank you.
Operator
Our next question comes from Whit Mayo from SVB Securities. Your line is now open.
Whit Mayo -- SVB Leerink Partners -- Analyst
Thanks. Reflecting back on 2020, 2021, I think you guys have certainly indicated that there have been a lot of distractions with COVID that has precluded you from perhaps ramping and investing into all of the care delivery initiatives that you would want to, you had to stand up a bunch of vaccination distribution support, there was telehealth. Just a lot of things I don't think you're supporting today. Is there anything that you can point to this year in terms of some of these new initiatives that you're doing that you haven't been able to do with the distractions, anything beyond marketing and community outreach, anything more care delivery focused?
Mike Pykosz -- Chief Executive Officer
Yes, absolutely. I'd probably say there's like three main improvements that we're focused on this year for care delivery and things that I think all three, we would have pulled forward without the pandemic. One, and we talked to this in our last call, but is the continual integration of Rubicon. So we're very excited about kind of having a fully integrated virtual specialty platform.
We think that's going to really continue to improve patient experience, lower specialist costs. And most importantly, really drive better quality of care by just having that kind of integrated specialty list approach. So that's something that we discussed. We really expect to kind of hit its stride sometime in the fourth quarter and kind of be fully implemented going into 2023, and we're -- again, we're optimistic about the process and approach and the savings is going to generate.
That's one. Number two is, I think there's a set of improvements to Canopy. One thing we love about our technology approach, as we continue to bring in more and more decision support, more and more clinical protocols and really take off more and more kind of the base decision-making from our providers and leverage all the teams to execute that, and that brings up more and more provider bandwidth to focus on the more challenging patients that you think you can't protocolize right? When you take our -- we call our most challenging patients, our VIP patients. And we take those patients, there's a number of factors.
You generate multiple chronic illnesses, social factors, behavior factors, etc. that it's impacting those patients, and that's what creates such a high risk of them going to the hospital. And so you never have a protocol, right, or a check the box of activity that's going to manage those patients while you need the expertise of the entire team working together and really [Inaudible] about how we keep that patient in the hospital. And the more you can free up the bandwidth to do that, by taking some of the base stuff like checking the boxes on to people get to preventive screenings and use metrics, the more that can be driven by protocol technology in the better, right? And so we continue to step forward on the technology to enable that.
And I think we're kind of -- we're past now what I would call the kind of more check the box around kind of heat screens, colonoscopy, mammogram, etc. Now we're moving on a more efficient support around kind of the disease management. So with these types of conditions here are the recommended drug regimens, etc. And again, it's not that actually don't know those things, but it reduces variability, ensures that every doctor, every day, every patient is practicing evidence-based standards.
Always ensures we have the best standards updated. And then it takes a lot of that pressure off of our doctors to remember off of those things. So we're really excited about that effort. That's kind of number two.
The number three is softer. It's just more of the bandwidth, right? It's more of the focus, right? And again, to the point I made before, if you can really be focused on how do I create an unmatched patient experience? How do I greet everyone, delight every patient every day? And how do I make sure that I'm really practically planning how to keep my patient out of the hospital. If I'm doing that, you'll generate great results, right? It's harder to do that when you're trying to navigate infection control protocols and staffing, you're trying to learn new telehealth protocols, etc., etc., etc., right? So I think there's just that final component really does make a difference.
Operator
Our next question comes from Kevin Fischbeck from Bank of America. Your line is now open, Kevin.
Kevin Fischbeck -- Bank of America Merrill Lynch -- Analyst
Great. Thanks. I was wondering if you could talk a little bit more about cost trend in the quarter. It looks like -- it sounds like you guys are saying that the quarter came in largely in line with your expectations.
I guess when we looked around and listening to other managed care companies, they seem to be talking about core volume not coming back the way they would have thought in the quarter, lot of the providers had weak volumes relatively speaking. So just a little more color about kind of what you're expecting and what you saw as far as utilization in the quarter?
Tim Cook -- Chief Financial Officer
Kevin, it's Tim. Thanks for the question. Yes, you track others better than I do. So it's always working to know what they were expecting versus what we were expecting and therefore, how actual results played out relative to expectations.
We did see, generally speaking, lower -- as Q1 developed, obviously, a lot of COVID costs, as we mentioned, with the Omicron's spike in January and February. I think January was the highest COVID month in the history of the company, somewhat aided by the fact that we've grown our patient population a lot, but still a lot of COVID dollars. We saw non-COVID utilization lower in Q1, and that's the release that we saw in Q2. As we took our approach to Q2 from an accrual perspective was similar to Q1.
So we will see how Q2 ultimately plays out. I will say utilization looks a little more normal for us in the quarter. You can imagine, given the growth of our business, the air bars around normal are probably wider than they would be for a larger plan with a relatively steady patient population. So I'd say, look, we're optimistic believe.
We'll see how Q2 develops just as we saw Q1 develop.
Mike Pykosz -- Chief Executive Officer
Kevin, the only thing I'd add to that, I think when we think about this at Oak Street, something I think about it, different than maybe a health plan, we look at medical costs that we control, right? And yes, you don't control, then we don't control COVID surges. But everything our care model is directed to do is to manage chronic illness keep our patent out of the hospital. We are actively seeing our patients and changing the trajectory of their care. And I think we're doing a two-level depth that obviously just helping that's not in their capability state, that's not in their progression state.
That's not what they do. And so we talk about medical costs, certainly internally, we never talk about -- this is what the trend happened to us. We talk about we drive medical costs lower by lowering hospitalizations. And when we're generating strong results, low 80K, and which corresponds to strong MLRs, like we have our team.
And when those are going up, we talked to our team about how do we kind of double down and -- to the question I answered before about the care model, how do we improve our care model results. So I just want to make sure we point that out. You hear me talk about the trend. I'm not speaking about what's happening in the macro market and more thinking about how are we executing our model and how is that driving great results.
And I think that is what we do and what we're very proud of is, I think we think we have the best care model anywhere for older adults with chronic illnesses and that makes a big difference in their care, right? And we think that can kind of overshadow any kind of smaller macro trends, which is kind of, again, different than what a health line is looking at.
Kevin Fischbeck -- Bank of America Merrill Lynch -- Analyst
Right. That's helpful. And then, Tim, I guess, you guys mentioned a number of -- I gave a number of numbers. And then sometimes, it looks like you were giving them on a gross basis, sometimes on a net basis.
So like I think you said that the favorable development was actually $10 million versus the $7 million, you talked about in the press release, and it sounds like you were kind of netting that against direct contracting. But then when you mentioned direct contracting of $3 million, it sounded like you were saying that that number was even net of some favorable number maybe on the M&A side. Is it possible to kind of give like the gross numbers and all of these things and help understanding kind of what exactly -- how is that going to think about these out-of-period numbers?
Tim Cook -- Chief Financial Officer
Kevin, you're right. So the $7.2 million in the press release is the net of the $3.7 million of revenue headwind in the $10.9 million of med cost capability. We are not breaking out the components of each of those. And the reality is there's always going to be interplay between MA and direct contracting.
And this quarter it was pronounced because of the retro trend adjustment, but I just want to highlight that if folks are doing the math and trying to do some -- I think Gary is trying to do some of this -- some implied math around direct contracting dollars or impact that it would be larger than just the $3.7 million on space.
Operator
Our next question comes from David Larsen from BTIG. Your line is now open, David.
David Larsen -- BTIG -- Analyst
Hi. What are you looking at for June volumes and then also July volumes. It's my understanding that in June, volumes are up a lot in hospitals. Are you seeing that? Is that continuing through July.
How are you thinking about the BA.5 variant? And when do you expect to reach EBITDA breakeven, please? Thanks a lot.
Mike Pykosz -- Chief Executive Officer
Yes. Thanks for the question. So the point I made a second ago, when we think about hospitalizations for our patients, again, I don't necessarily think the macro trends of what's happening in the broader market, including commercial and Medicaid, etc., and even healthier Medicare apply to us. So when we look at what's happening with hospitalizations for patients.
And again, to Tim's point, when there's massive COVID waves, obviously, we impacted by that. But when we look at our hospitalization to 80K, and we look at that as an indicator of our performance. All of our providers and our center team members are bonus based on their performance against admissions per thousand, right? So that's one of the key metrics of Oak Street Health. We keep our patient [Inaudible] a hospital.
And we mean and we feel like that's what our care model does. And so again, I don't -- we're certainly not going to share -- July results ready by -- again, I don't think that necessarily reading into what's happening with hospital volumes more broadly always translates to what's happened with Oak Street and our patient population in our care model results. To the COVID question, we obviously do our best to make sure our patients are vaccinated and make sure our patients are boosted. And our patients do get covered that they get the therapeutics like [Inaudible] that can make a big difference in their health trajectory.
And I'd like to think that we're making a difference there. But that said, when you look at kind of the COVID rates of hospitalizations for Oak Street, we're in 20 states, a little bit more weighted toward the Great Lakes and Mid-Atlantic region, just given historically where we opened up first. But generally kind of our COVID costs are going to be in relative proportion to what is the hospitalization rates in those communities that we have patients today. And as we get more and more national, that will kind of keep approaching kind of the more national levels.
And as we've shared, we will be breakeven 2025 or prior.
David Larsen -- BTIG -- Analyst
OK. Great. Thanks very much. Appreciate it.
Operator
Our next question comes from Craig Jones from Stifel.
Craig Jones -- Stifel Financial Corp. -- Analyst
Hey. Thank you. I think originally, you had said for platform contribution margin this year, around $68 million. I think you've done $74 million so far.
Is still a good number? Or has that gone up?
Tim Cook -- Chief Financial Officer
This is Tim. I'd say our expectations for the year are unchanged on that.
Mike Pykosz -- Chief Executive Officer
I think we are over time. So I want to be respectful of our schedule and other's time and think we should end the conference.
Tim Cook -- Chief Financial Officer
Yes. Yes, we do need to hop, unfortunately. We're past the hour. Craig, hopefully, that was the extent of your questions and appreciate everyone's time this morning and look forward to connect again.
Operator
[Operator signoff]
Duration: 0 minutes
Call participants:
Sarah Cluck -- Head of Investor Relations
Mike Pykosz -- Chief Executive Officer
Tim Cook -- Chief Financial Officer
Lisa Gill -- J.P. Morgan -- Analyst
Ryan Daniels -- William Blair and Company -- Analyst
Justin Lake -- Wolfe Research -- Analyst
Jamie Perse -- Goldman Sachs -- Analyst
Gary Taylor -- Cowen and Company -- Analyst
Jessica Tassan -- Piper Sandler -- Analyst
Elizabeth Anderson -- Evercore ISI -- Analyst
Michael Ha -- Morgan Stanley -- Analyst
Sandy Draper -- Guggenheim Partners -- Analyst
Whit Mayo -- SVB Leerink Partners -- Analyst
Kevin Fischbeck -- Bank of America Merrill Lynch -- Analyst
David Larsen -- BTIG -- Analyst
Craig Jones -- Stifel Financial Corp. -- Analyst