Image source: The Motley Fool.
Walgreens Boots Alliance (WBA 0.57%)
Q4 2023 Earnings Call
Oct 12, 2023, 8:30 a.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Good morning. My name is Krista, and I will be your conference operator today. At this time, I would like to welcome everyone to the Walgreens Boots Alliance, Inc. fourth-quarter and fiscal year 2023 earnings conference call.
[Operator instructions] Thank you. Tiffany Kanaga, vice president of global investor relations. You may begin your conference.
Tiffany Kanaga -- Vice President, Global Investor Relations
Good morning. Thank you for joining us for the Walgreens Boots Alliance earnings call for the fourth quarter of fiscal year 2023. I'm Tiffany Kanaga, vice president of global investor relations. Joining me on today's call are Ginger Graham, our interim chief executive officer; Manmohan Mahajan, our interim global chief financial officer; and John Driscoll, president of U.S.
healthcare. In addition, Rick Gates, senior vice president and chief pharmacy officer of Walgreens; and Tracy Brown, president of Walgreens retail and chief customer officer, will participate in Q&A. All references to the COVID-19 headwind on today's call include U.S. vaccines, drive-thru tests, and OTC tests.
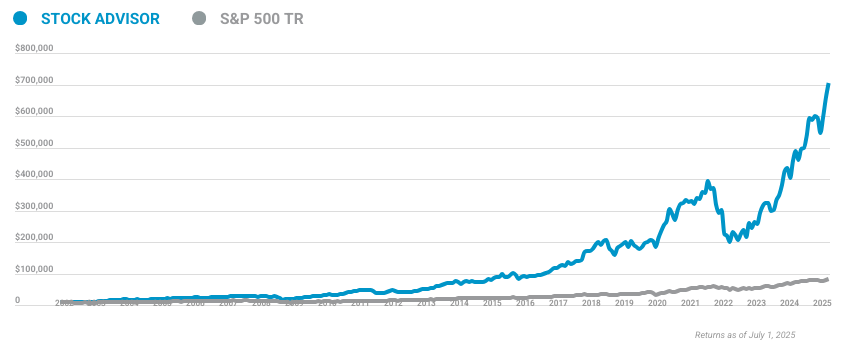
10 stocks we like better than Walgreens Boots Alliance
When our analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Walgreens Boots Alliance wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of October 9, 2023
As always, during the conference call, we anticipate making projections and forward-looking statements based on our current expectations. Our actual results could differ materially due to a number of factors, including those listed on Slide 2 and those outlined in our latest Form 10-K filed with the Securities and Exchange Commission. We undertake no obligation to publicly update any forward-looking statement after this presentation, whether as a result of new information, future events, changes in assumptions, or otherwise. You can find our press release and the slides referenced on this call in the Investors section of the Walgreens Boots Alliance website.
The slides in the press release also contain further information about the non-GAAP financial measures that we will discuss during this call. I will now turn the call over to Ginger.
Ginger Graham -- Interim Chief Executive Officer
Thanks, Tiffany, and good morning, everyone. The good news you heard yesterday is that Tim Wentworth has agreed to join WBA as our new chief executive officer effective October 23rd. We're thrilled to have Tim and believe he will make a meaningful contribution to the future of the company with his deep knowledge and expertise in healthcare. We've asked him to make a few comments this morning, and I would like to turn it over to him now.
Tim?
Tim Wentworth -- Incoming Chief Executive Officer
Thanks, Ginger. I'm excited to join the call today and even more excited to get to work after next week. During my nearly three decades in healthcare, I've led efforts to create innovative and flexible health services to meet the needs of health plans, employers, and government organizations as well as their employees and members. And you know whether building a team that grew the largest, most operationally efficient PBM in the country or helping to establish Accredo as the most significant specialty pharmacy in the United States, or helping to put together every Evernorth, a $100 billion-plus health services business, I've consistently built relationships and offered solutions both for customers who are looking for a trusted innovative partner who listens and for patients who are looking for access and affordability.
This impact was the direct result of having a winning team of employees and a culture that values patients. Now I know WBA. I have worked with Walgreens as a customer, partner, competitor, investor, and family member, and I understand the challenges ahead for us as well as for the healthcare industry. Walgreens was built on convenience, access, and trust and has unique advantages in today's healthcare environment.
I see the opportunities before us to build on our pharmacy strength and our trusted brand to evolve healthcare and the customer experience to deliver better outcomes at a lower cost. Now I've learned a lot over the recent weeks. As you might imagine, I've spent time with each and every board member, talking about the future and their priorities, learning about our challenges and opportunities, and most importantly, the importance of execution. Those discussions inform my own research.
And of course, I have my personal experiences. For example, just last week, Mave, a terrific store employee in Rochester, New York, professionally and cheerfully delivered to make a critical prescription to help my mother. It was the kind of experience I appreciate and everyone deserves. And I know that Mave is surrounded by the committed pharmacists and other team members, all of whom together can improve the lives of each person who walks through our door, in my mom's hometown, Walgreens, and Rochester, and in every store we operate.
All of these experiences together made my decision to join WBA, frankly, an easy one. There is a reservoir of goodwill for this company across communities and a substantial opportunity to return value to our customers, employees, and shareholders. Alongside the board, our team members, and partners, I'm enthusiastic about our future and realizing our healthcare strategy and vision. I'm humbled to serve as WBA's next CEO and look forward to speaking to many of you in the coming weeks.
Ginger, thank you, and thank you to the entire WBA board for this opportunity. I'll now turn it back to you.
Ginger Graham -- Interim Chief Executive Officer
Thanks, Tim. I'm excited and looking forward to working with you. While Tim won't be on the Q&A, I'm sure he will be talking with all of you soon after he joins the company. With that, let me turn to our business results.
My time here has been very focused on stabilizing our talent, addressing our level of spending relative to the scale of our business, and critically reviewing our capital allocation across the business. With the benefit of having been on the board, it has accelerated my ability to work with the team and make swift decisions and implement changes across many areas of our operations. We have focused on three near-term operational priorities. We must support our customer-facing activities, scrutinize every penny of spend that does not directly benefit the customer and improve cash management.
I will restate what we know and is critical to our future. We believe the fundamentals of our core business remain strong. We dispensed over 1 billion prescriptions annually across our retail and specialty pharmacies. We play a key role in healthcare delivery in this country.
78% of Americans live within five miles of a Walgreens or a Duane Reade and 58% of us are likely to visit a local pharmacy as the first step for a nonemergency health need. Our trusted brand, deep community relationships, and convenience form the foundation of our pharmacy business and our platform for growth as we expand throughout other areas of healthcare. I see significant opportunity to improve the cost base of this business. During the last 6 weeks, we have taken decisive actions to rightsize our cost structure.
We expect over $1 billion of cost savings during fiscal year 2024 based on the actions we have already taken and are in progress. Examples include: reducing our headquarter costs going line by line, expense category by expense category, and reducing all nonessential spend. We've reviewed and are reducing areas for contracted or project work. We are altering our store operating hours based on local market trends.
We are closing unprofitable stores. We're driving supply chain efficiencies, including using AI to more accurately forecast demand and optimizing our transportation network. We're also implementing centralized services that control inventory, reduce workload, and provide better customer support. We're taking a hard look at all projects and stopping those that are not essential.
These actions reduce expenses, but more importantly, they help focus our energy on the most important needs for the business and for our customers. We are more aggressively managing decisions that impact cash. This includes working capital management, targeting over $500 million of improvement and defining near-term capital expenditure reductions, which we expect will bolster our balance sheet and support our priorities. Let me give you some examples.
One major effort at Walgreens has been to introduce a perpetual pharmacy inventory system across the chain. As of last week, it is available to all 9,000 of our stores. This provides complete visibility of our inventory in the pharmacies and supports our work to reduce excess inventory and free up working capital. It also has many benefits for the pharmacy staff, and feedback has been overwhelmingly positive as it simplifies workflows reducing store level activities.
Another area where we have reduced working capital and impacted our workflow at the store level is related to regional micro fulfillment centers. These centers allow us to improve product availability, while, at the same time, reduce total inventory levels. Our 11th micro fulfillment center opened three weeks ago. These centers currently support more than 4,300 stores, filling over 2.3 million prescriptions each week across 29 states.
As we fill more prescriptions centrally, it frees up our staff to spend more time with customers, offering other health-related products and services and it relieves some of the pressure on store staffing. It is important to note that we have paused further expansion of our fulfillment centers to first drive improvements in the rollout, so we may fully realize the many benefits the centers offer: working capital reduction, inventory tracking and control, customer service enhancements, workflow improvement and reduction in cost to fill. The team has defined threshold requirements of performance before we move to implement the final five locations. There is significant opportunity to reduce retail inventory and optimize our retail product mix.
We are reducing SKUs, addressing slow-moving product categories, and moving e-commerce shipments to fulfillment by our stores, getting the delivery to the customer, in most cases, in less than one hour. This is augmented by real progress on our own brands, which offers a big opportunity that we have been slow to capture. All of these working capital improvements yield customer service benefits and workflow improvements for our staff. Cash is also influenced by our capital expenditure budgets, and we are reducing our capital expenditures in fiscal year 2024 compared to last year, down approximately $600 million.
We have already identified many of the actions required to deliver this improvement and to ensure that we execute all capital and project expenses are now being reviewed and approved centrally. One other important action I want to mention is our return to the office. I have recently communicated that our leaders are expected to return to the office this month, and all other team members are expected back in late November. We are convinced that our ability to act quickly, deliver priority projects, and respond to business demands will be improved by being together.
With that, I'll hand it over to Manmohan to review our financial results and our outlook for fiscal year 2024.
Manmohan Mahajan -- Interim Global Chief Financial Officer
Thank you, Ginger, and good morning. Fourth-quarter adjusted EPS came in near the low end of the range provided on June 27th and in line with our update on September 1st. Our results reflected a further slowdown in respiratory events, shifting consumer behaviors, driven by a challenging macroeconomic environment, and lower COVID-19-related contributions. Overall, we delivered 8.3% sales growth on a constant currency basis.
This includes $1.4 billion in growth in our healthcare business versus the prior year. Our U.S. retail pharmacy business grew 3.6% and our Boots U.K. business delivered 10.9% sales growth.
Adjusted EPS of $0.67 was down 18% on a constant currency basis. The 18% decline was driven by lower COVID-19 contributions, lower sale leaseback gains net of rent, and a higher tax rate. We saw positive results from underlying retail pharmacy performance, lower incentive accruals, strong international growth, and improved profitability in U.S. healthcare.
GAAP net loss of $180 million improved by $235 million compared to prior year. Remember that we had a $783 million noncash impairment charge in the year-ago quarter. The loss in the quarter was driven by charges for certain legal and regulatory accruals and settlements and onetime charges related to transformational cost management program. Now let's move to the year-to-date highlights.
Fiscal '23 sales increased 5.6% on a constant currency basis. Adjusted EPS of $3.98 was down 20.3% on a constant currency basis. Our results reflected lower COVID-19 contributions and increased labor investments. These challenges were partly offset by lower incentive accruals, growth in international and retail performance in the U.S.
GAAP net loss was $3.1 billion, compared to net earnings of $4.3 billion in fiscal '22. Fiscal '23 included a $5.5 billion after-tax charge for opioid-related claims and lawsuits. Now let's move to the U.S. retail pharmacy segment.
Comp sales growth was 5.7%, reflecting higher brand inflation and mix impacts in our pharmacy business and comp script growth. AOI was down 29.4% in the quarter, reflecting a 27% impact from lower COVID-19 contributions and a 17% impact from lower levels of sale leaseback gains net of rent, higher underlying pharmacy gross profit, and lower incentive increased 9.2% in the quarter, driven by brand inflation and mix impacts and comp script growth. A weaker-than-normal respiratory season and impact of Medicaid redeterminations resulted in a weaker overall prescription market during the quarter. Third-party market data showed flu, cold, and respiratory activity down 35% compared to the prior-year quarter.
Despite these weaker trends, compe scripts grew 1.6%, excluding immunizations. We administered roughly 400,000 COVID-19 vaccinations in the quarter down from 2.9 million in the prior year quarter. Excluding the impact of COVID-19, fourth quarter adjusted gross profit increased versus the prior year period. Turning next to our U.S.
retail business. During the quarter, the retail business was impacted by a weaker-than-normal respiratory season and a continued shift in consumer behaviors, driven by a challenging macroeconomic environment. As a result, comparable sales declined 3.3% in the quarter. There are three main drivers: first, an 80% decline in COVID-19 test kits impacted growth by around 160 basis points; second, weaker cough, cold, flu sales had an approximately 100 basis points impact; and lastly, we were impacted by approximately 60 basis points from summer seasonal weakness, as customers continue to pull back on discretionary spending, reflecting the challenging macroeconomic environment.
Looking at category performance, we saw a decline in health and wellness, while personal care and beauty both grew low single digits. Retail gross margin was impacted by elevated shrink and lower sales in higher-margin categories, such as cough, cold, flu seasonal, and COVID-19 test kits. Despite the pressure in the second half, gross margin grew by nearly 100 basis points in fiscal '23, on top of a 100 basis point increase in the prior year. Turning next to the international segment and as always, I will talk in constant currency numbers.
The international segment again performed very well in the quarter, delivering profit ahead of guidance. Sales increased 6.7%, with growth across all international markets. Boots U.K. was up 10.9% and Germany wholesale grew 3.5%.
Gross profit increased nearly 10%, outpacing sales growth. Boots U.K. experienced continued strong retail growth and improved pharmacy margin compared to the prior year period. Despite higher inflation and increased store-related costs, SG&A as a percentage of sales improved, benefiting from disciplined cost management.
These impacts resulted in adjusted operating income growth of 52%. Let's now look in more detail at Boots U.K. Comp retail sales increased 11.7%, on top of a 15.2% comp in the prior year quarter. Boots grew market share for the tenth consecutive quarter, approximately 1 percentage point versus the prior-year quarter, with gains in beauty and health and wellness.
Boots.com sales grew 29% year on year and represented over 13% of our U.K. retail sales. Turning next to U.S. healthcare.
U.S. healthcare segment results were in line with the guidance provided on June 27th, with AOI and adjusted EBITDA both up sequentially and year over year. The business continues to rapidly scale with fourth-quarter sales of $2 billion, reflecting the acquisition of CareCentrix, the acquisition of Summit Health by VillageMD, and growth in all businesses. Segment pro forma sales grew 19%, driven by VillageMD sales of $1.4 billion, up 17% on a pro forma basis.
The growth was led by higher value-based lives, expansion of the clinic footprint, and increased fee-for-service volumes as clinics mature. CareCentrix sales were up 24% on a pro forma basis, and Shields delivered pro forma sales growth of 29%. Segment gross profit improved 29% sequentially. Adjusted EBITDA was a loss of $30 million, an improvement of $103 million from the prior year quarter.
Turning next to the cash flow. We generated $2.3 billion of operating cash flow in fiscal '23, reflecting lower COVID-19 contributions, opioid settlement payments, and losses in our U.S. healthcare segment. Fiscal '23 capital expenditures of $2.1 billion increased by approximately $400 million compared to the prior year.
This was driven by growth initiatives, including VillageMD and the micro fulfillment center rollout. This resulted in free cash flow of $665 million. We also reduced debt by $2.6 billion in fiscal '23. As Ginger discussed, we are taking a number of actions to drive improvement in free cash flow in fiscal '24, including approximately $600 million in reduced capital expenditures and approximately $500 million benefit from working capital optimization initiatives.
I will now turn to our fiscal '24 guidance. We are guiding to fiscal '24 adjusted EPS of $3.20 to $3.50, down from $3.98 in fiscal '23. Before discussing underlying performance, I want to mention some key headwinds that we will face in fiscal '24. These include lower sale and leaseback contributions, a higher tax rate, and lower COVID-19 contributions.
We're also assuming continued macroeconomic pressure on the consumer and a weaker respiratory season compared to the prior year. Excluding the impact of these headwinds, our forecast assumes underlying growth which is primarily driven by two factors. First, we expect accelerating profitability in our U.S. healthcare business in 2024.
As the segment continues to scale with adjusted EBITDA expected to be at or around breakeven. Second, we expect U.S. retail pharmacy underlying adjusted operating income to be driven by immediate actions to improve the cost base and modest underlying growth in both retail and pharmacy. Let me now illustrate the larger moving pieces as we bridge from fiscal '23 to fiscal '24.
I mentioned three notable headwinds to adjusted EPS. Sale and leaseback is estimated to have a negative year-on-year impact of between 11% to 13%. As we have said before, we do not expect any contribution from sale and leaseback beyond fiscal '24. Tax rates will be higher in 2024, increasing by approximately 10 percentage points compared to 2023 due to higher international rates and benefits recognized in 2023 that are not expected to repeat in 2024.
Finally, we're projecting lower COVID-19 contributions that result in a 6% to 7% year-on-year impact. Excluding these impacts, we expect underlying growth of 9% to 12%, driven by accelerating profitability in U.S. healthcare and immediate actions to improve our cost base across the company. Let me now walk you through the 2024 guidance in greater detail.
Overall, we expect total sales in fiscal '24 to be up 1% to 4% on a constant currency basis. Adjusted operating income is expected to be down 5% to 12% on a constant currency basis. Let me now walk you through the assumptions and guidance for each of our reporting segments, starting with U.S. retail pharmacy.
U.S. retail pharmacy segment sales are projected to be flat to up 2%. AOI will be negatively impacted by approximately 8 percentage points from the lower COVID-19 contributions and roughly 11 percentage points of lower sale and leaseback gains. Excluding these impacts, the underlying business is projected to drive 5% to 10% AOI growth.
I will now take you through the key business drivers. First, we anticipate script volume growth driven by overall market growth. On reimbursement, we have roughly 75% of the contract signed for calendar year '24. We do expect reimbursement pressure to be less of a headwind in fiscal '24 than in fiscal '23.
We're projecting approximately 5 million COVID vaccinations in 2024. Quarter to date, we're well on track and have already administered over 3 million COVID vaccinations. In retail, we expect margins to benefit from our category performance improvement program and a roughly 1 percentage point increase in own brand penetration. At the same time, we're adopting a prudent approach.
We see a continuation of the challenging trends that impacted the second half of fiscal 2023. We're projecting flat comparable sales due to a milder cough, cold, and flu season year on year, lower COVID OTC test kit volume, and continued consumer pressure. We're also planning a higher level of shrink, which has been increasing in the last several months and continues to represent a serious systemic issue across the retail industry. Within SG&A, we expect to achieve over $1 billion of cost savings during fiscal 2024, as Ginger has already described.
Turning next to guidance for the international segment. Segment sales are projected flat to up 4% on a constant currency basis. We expect adjusted operating income of $745 million to $770 million, representing a constant currency decline of 18% to 21%. The year-on-year decline is entirely driven by property transactions during fiscal '23, which will not be repeated, and the pending sales of the business in Chile.
Excluding those impacts, we expect AOI growth to be flat to up 2%, with continued execution within Boots U.K. retail business held back by the impact of inflationary pressures. Now let's turn to U.S. healthcare.
We are focused on driving improved financial performance for U.S. healthcare in 2024. We expect fiscal '24 sales of $8.3 billion to $8.8 billion, reflecting first full year of Summit Health and ongoing growth in all businesses. On a pro forma basis, we see sales growth of 10% to 17% and expect fiscal '24 adjusted EBITDA to be breakeven at the midpoint of the guidance range.
This represents an increase of $325 million to $425 million compared to fiscal '23, driven by growth in full-risk lives, fee-for-service volume, optimization of the clinic footprint and realignment of the cost base at VillageMD, robust growth at Shields and Walgreens Health business growth, driven by scaling of our clinical trial business and healthcare services and through cost management. We assume an effective tax rate of approximately 19% to 20%, with the year-over-year increase driven by higher international statutory tax rates and benefits recognized in 2023 that are not expected to repeat in 2024. Interest expense is expected to decrease by approximately $80 million. In the first quarter, we will be lapping the prior year quarter's adjusted EPS of $1.16.
The following five factors are expected to have an outsized impact in the first quarter this year. First, we had a significant tax benefit in prior year period, which will not repeat in the first quarter of 2024. Second, we're expecting COVID-19 contributions to be lower in the first quarter, reflecting last year's omicron wave and seasonality. Third, we anticipate lower contributions from sale and leaseback activity.
Fourth, we're lapping elevated levels of labor investments in our pharmacy staff. Finally, we also expect a more normalized flu season in fiscal '24, peaking in the second quarter versus the early start in the prior year. Moving beyond the first quarter, we will see sequential improvement, and I will discuss the top four drivers. First, we're executing a series of actions to lower our cost base.
These will have limited impact on the first quarter, but will start to ramp in the second quarter. There is adjusted EPS benefit of $0.50 to $0.60 in the balance of the year compared to the first quarter. Second, in our U.S. healthcare segment, we expect profitability to improve from optimizing the clinic footprint, growing patient panels, and realigning costs.
Third, we expect growing contributions from retail initiatives, including sequentially improving retail comps and margin expansion programs. Finally, seasonality plays a role in our business, benefiting the second quarter, which is usually the height of the cough, cold, flu season in the U.S. and is when Boots U.K. sees significant profit driven by the holiday season.
With that, let me now hand it over to John to discuss our U.S. healthcare business.
John Driscoll -- President, U.S. Healthcare
Good morning, and thanks, Manmohan. Over the past two years, we've acquired or launched new businesses in primary care, multi-specialty, post-acute care, urgent care, specialty pharmacy services, population health, and provider enablement. Each of these businesses builds upon our strong foundation in retail pharmacy to tap into high-growth healthcare services. Walgreens uniquely has an advantage in convenience, consumer traffic, independence, and trust that will help us with our health plan and provider partners create solutions that deliver better outcomes at lower cost.
We connect daily with many of the patients that our plan and provider partners struggle to reach. Our goal is to be the independent partner of choice, not just in pharmacy, but also in healthcare services, where we can lower costs and help patients. Today, most of our customers come to Walgreens to meet their pharmacy needs. Increasingly and in the future, our pharmacy teams will be a critical part of how our plan and provider partners bend the cost curve.
So whether you're a health plan or a health system, you're dealing with one Walgreens and a suite of capabilities and services. Here are some of the ways that our U.S. healthcare assets work with Walgreens to better serve our customers and payer, provider, and pharma clients. Shield is working with our Walgreens Specialty Pharmacy to convert Walgreens locations to Shield's partner sites, collaborating with our contract pharmacies and delivering better adherence for patients on complex specialty drugs and better value for hospitals.
Walgreens Health and CareCentrix are partnering with Pearl Health to support providers who'd like to transition from fee-for-service to value-based care by leveraging Pearl's tech solutions with Walgreens' healthcare services. We'll accept full medical risk as we support physicians' patients by providing post-acute and home health solutions from CareCentrix and population health services from Walgreens Health. All of this is underpinned by Walgreens' engagement of our customers, ensuring them access to better care. Our clinical trials business, which launched just last year, leverages our pharmacy capabilities and data to recruit and execute on clinical trials for our pharma clients.
We will engage patients in all markets, including underserved communities. To date, we've signed 15 contracts and continue to see increasing demand for our services. CareCentrix provides an increasing number of post-acute services to health plans. Combining Walgreens convenient locations and CareCentrix health plan relationships and patient management, opens the door for a significant opportunity in durable medical equipment sales in our stores.
The U.S. healthcare segment has ramped to an $8 billion sales run rate in just two years. Our healthcare services aim to deliver better value for our payer and provider partners. We meet patients where they are, in order to improve access to lower-cost solutions.
While we have made progress on the build-out of our healthcare business, we are not satisfied with the near-term returns on our investments. We will continue to grow in 2024, but with a renewed focus on more profitable growth. We have seen some improved performance in the fourth quarter, with adjusted EBITDA sequentially increasing by $83 million. Our results reflect gross profit growth, with each quarter this year building on the prior with an enhanced focus on expense discipline.
We are taking swift action to unlock the embedded profits at Village and already see the benefit of improved capital and expense management with the addition of our new CFO at Village, Rich Rubino. VillageMD, Summit Health, and CityMD will be the most meaningful drivers of growth in fiscal 2024. It has taken us longer than anticipated to realize the cost synergies across the combined assets. We also need to solve for a less efficient cost profile and excellence in execution.
We believe that we can best enhance VillageMD growth and value by focusing on increased density in our highest opportunity markets and expanding integration of our digital assets. As we grow, we are constantly evaluating our footprint. With that, we plan to exit approximately five markets and approximately 60 clinics in fiscal 2024. These exits may take a variety of forms, including outright sales and hybrid equity arrangements as examples.
As we exit these nonstrategic markets, our long-term focus will be on achieving density in those regions with the greatest potential to drive future profitability growth and where we can best serve patients with our consolidated set of assets. The VillageMD model works, as evidenced by the consistent performance of reducing total cost of care and improving outcomes in our more mature markets. VillageMD has a Net Promoter Score of 89, which is one point higher than what I shared a year ago. We are also launching new virtual and less capital-intensive models.
In August, we launched a pilot program with CityMD and Duane Reade, where a Duane Reade Walgreens customer can click a QR code and set up a visit at CityMD or a virtual telehealth visit with a clinician. We plan to roll out this digital partnership across Manhattan in the fall. Our VillageMD business is a primary care-led risk-bearing platform serving all customers and payers, focusing on utilizing their technology platform to deliver the best health outcomes in a lower total cost of care. Growth in clinics translates into growth in full-risk lives as evidenced by the growth in member months in all markets and mature markets.
From fiscal year 2022 to 2023, VillageMD has grown full-risk member months by 40% across all markets and 24% in our mature markets. Even with the rapid growth of VillageMD clinics, we're seeing positive proof points of the business' ability to perform in full-risk arrangements. For our full-risk MA population in three mature markets, we've seen Village bend the cost curve across multiple payers. Going forward, as we focus on more profitable growth, we will build on positive clinical margin to deliver contribution margin on a consolidated basis.
Next, I'd like to discuss our latest Walgreens Health partnership. We're partnering with Pearl Health, a provider enablement company, that can help Walgreens expand our risk offering to more community-based primary care providers. Walgreens and Pearl together will provide a management services offering, with Walgreens providing prescription fulfillment, medication adherence, immunizations, care gap closures, and diagnostic testing. Integrating local Walgreens pharmacies translates into more access to members with chronic illness, and more opportunities to influence better patient outcomes.
This partnership enables physicians and health systems to work with us to manage the chronically ill in a much more targeted fashion. Pearl's access to doctors through the ACO reach program creates a care traffic control system that can deliver on our commitment to provide better healthcare at a lower price for plans and patients. This model is also capital efficient, scalable, and configurable nationwide. With this partnership, we are initially assuming risk for 9,000 lives in 12 markets.
Our existing Walgreens Health payer relationships have started with fee-for-service arrangements tied to care gap closures, clinical quality services, and screening. Successful performance with these services provides a sound foundation for moving up the risk continuum. We expect to develop a range of risk arrangements that will leverage our assets across the care continuum, including VillageMD, Summit, and CareCentrix, all building on our suite of clinical services available at Walgreens. With that, I'd like to pass it back to Ginger for closing remarks.
Ginger Graham -- Interim Chief Executive Officer
Thank you, John. The last several weeks have reinforced my confidence in the company's potential and also crystallized what actions must be taken to achieve it. We are focused on the right things. I am already encouraged by early results from decisions that advance our customer focus, eliminate cost, and conserve cash.
While we have a challenging year ahead of us, as Manmohan said earlier, our plan anticipates 9% to 12% growth in adjusted operating income from our underlying business. This comes in large part from our aggressive actions to manage costs we control. Of course, none of this would be possible without the hard work and dedication of a vast team of people here at WBA. They are doing the work, and they've moved quickly to respond to the realities of the business.
I'm thankful for their responsiveness and commitment and for the opportunity that lies ahead as we set up WBA for a successful future together. Now I would like to open the line for questions. Operator?
Questions & Answers:
Operator
[Operator instructions] Your first question comes from the line of Lisa Gill from J.P. Morgan. Please go ahead.
Lisa Gill -- JPMorgan Chase and Company -- Analyst
Thanks very much. Good morning, everyone. I just really wanted to understand two things a little bit better. First, John, when you talk about the ramp and the challenges to profitability, one, when we think about that improved profitability, the exit of those markets in the 60 clinics, is that contributing to better AOI as we think about 2024? And then secondly, trying to better understand where you see the biggest opportunities from a challenge perspective, you talked about a lot of positive at Pearl, you talked about the turnaround at Village.
Obviously, CareCentrix did really well this quarter. But can you maybe just talk about what are some of the other challenges you feel like you need to overcome to really truly make this a profitable business?
John Driscoll -- President, U.S. Healthcare
Sure. I think -- Lisa, thanks for the question. If you think about the cost reduction, that's only one piece of what we're doing at Village City and Summit. It's really a three-pronged strategy.
We are rightsizing the footprint and getting our expenses in the right place. There are revenue synergy opportunities, and we're seeing consistent growth in core revenues, which indicates that there's some opportunity on the margin side, which we are quickly getting after. And then the rest of U.S. healthcare, actually, we're seeing substantial growth and building profitability in CareCentrix Shields our analytics business, our U.S.
healthcare business. So we're seeing substantial demand clinical trials is doing quite well. And so I think, as a portfolio, we have -- we are very confident in our ability to perform in '24. If you look at those revenue numbers, we've got the revenues.
Now we're going to get at some more effectively -- some of the embedded profits.
Lisa Gill -- JPMorgan Chase and Company -- Analyst
And then just as it ties into kind of what everybody is talking about on the retail side, right, and I know you've given some guidance there. But as we think about expectation of scripts coming down, I would think that maybe there's an opportunity for more scripts to be pulled through into Walgreens. I understand respiratory, etc. But maybe if somebody can comment, Rick, if Rick is on the call.
How do you think about that pull-through and opportunity on the scripts, excluding what we're seeing on the respiratory side? I know that the talk was 75% of relationships are signed on reimbursement, but reimbursement is expected to be down. Like what are going to be some of the big drivers beyond the $1 billion of incremental cost saves that we can actually see drive the operating profit in your core pharmacy business?
Rick Gates -- Senior Vice President, Chief Pharmacy Officer
Yeah. And Lisa, this is Rick. It's a great question. And I'll kind of give the building blocks to script growth that we're expecting this year.
Obviously, we saw a weaker end of the fiscal year from market growth, specifically around cough, cold, flu, some of the respiratory, and some of the Medicaid redetermination, which shows some lower utilization from consumers. So the primary driver of the market coming back in line with what the expectations are from IQVIA and others. And so that's really what we've seen as we started into the first quarter of the fiscal year and market is going to be a big underpinning to what we do. But we continue to advance our adherence programs that are really driving incremental script growth, partnering with health plans and others to really drive better adherence.
And obviously, that does help on the script side. You're also going to see some access initiatives, especially going into calendar year '24, which should be some tailwinds for us. I think some changing dynamics in the marketplace or having individuals choose more open access and things that should give us access differently than what we've seen in the past. And the last one would be that we're really focused on potential for file buys and opportunities given some of the changes in the marketplace.
So I think there's a bunch of drivers that really give us confidence that we have tailwinds behind us in the scrip [Inaudible].
Operator
Your next question comes from the line of Charles Rhyee from TD Cowen. Please go ahead.
Charles Rhyee -- TD Cowen -- Analyst
Yeah. Thanks for taking the question. I wanted to ask about Tim coming on board here. Obviously, it seems like it was a fairly quick turnaround process.
Maybe you can give us a little bit more insight into the -- that kind of hiring process sort of when it was identified? And also here, obviously, starting in a week and a half or so, the company has given guidance. Any kind of sense on his involvement in sort of the business planning for the coming year? Anything there? And then also, obviously, you've given a lot of details in preserving and generating greater cash flow, obviously, through working capital reduction, etc. Any thoughts from the board on sort of the dividend policy at this point?
Ginger Graham -- Interim Chief Executive Officer
Thanks, Charles. Let me start off with the process around Tim. We, as a board, engaged a global executive search firm and spent quite a bit of time with them talking about what we believe were the important characteristics, attributes, and experiences of someone who would lead an organization of this impact and magnitude. We did review dozens of candidates.
There was quite an extensive search process that was undertaken. And we then narrowed it down to a top few, where personal interviews were conducted with those individuals. We did a very aggressive background and reference check with the primary candidates and then have had, what I would call, very extended conversations in a broad sense about philosophy, background, experiences, the future, the market dynamics, the capabilities required and about the ability to manage a very complex global organization. As Tim mentioned in his comments, every single board member has been involved.
I would say that we've done a very extensive evaluation through the process. And we did decide in the process that Tim was a very striking candidate for us on a number of fronts. Obviously, we were clear that we were looking for someone who had extensive background in healthcare, and Tim brings that pharmacy provider, payer networks, distribution. He really does understand a surround sound of the feedback that we get from the market about Walgreens and its many businesses.
He also has managed scale and complexity before, which I think is very important. This is a $140 billion business. It's global. It has many possibilities, but someone has to be able to manage the strategic and the operational aspects of that.
And I think you heard from him, even in his quick comments, he's very patient and customer-focused, which to me is a primary importance because that passion for the business, the understanding we have on human lives, the importance of our discipline, our safety and compliance, our quality, our personnel and the love he has of the store, those are big wins the company. So I personally am thrilled I've had -- I don't know how many hours with Tim. And it's a lot, and he and I are not done yet. We actually start together next week in a very extended work session.
So I think the board is excited as Tim conveyed his excitement, and we're all looking forward to him starting. Obviously, that won't happen again now until the 23rd. So you -- second question you asked was his involvement in all of this. Obviously, we've only recently come to this agreement between us.
And so Tim has not been involved at all in the business or the operations. He's not been a party to forming the 2024 plan. although he and I have had extensive discussions about what the opportunities are, the business capabilities, and our challenges, I think he mentioned maybe in his comments as well, that he comes in eyes wide open. So I think that's very important.
But Tim is not a party to this plan. He is a party to what we believe is possible, and he understands the assumptions we're making and he can't wait to get here. The third question I think you asked was the board and its discussions about the dividend. So as you might imagine, this is a very important topic to the company.
We have a very thorough process as a board that we review every year. And at this point, the board has made no changes to the dividend policy.
Operator
Your next question comes from the line of George Hill from Deutsche Bank. Please go ahead.
George Hill -- Deutsche Bank -- Analyst
Yeah. Good morning, guys. This is kind of a two-part question that go together. I guess, can you talk about -- if we think about the segments, how we should look at apportioning the $1 billion in cost savings and kind of the other side of that is the the cut in capex seems pretty severe.
It's taking $0.5 billion or so out on a sub-$2 billion number. How should we think about from a segment perspective, kind of where the capex cuts are coming from and kind of how they're being apportioned? And I don't know if you can kind of give any examples specifically of the bigger sources of cost-cutting savings or the bigger sources of capex savings.
Manmohan Mahajan -- Interim Global Chief Financial Officer
Yeah, sure. So let me start with the cost savings. We're expecting at least $1 billion of cost savings. And I think the way you need to think about this is majority of this is going to be coming from our U.S.
retail pharmacy business. And three or four components, let me just walk through them real quick. Ginger talked about, we're looking at all costs related to headquarter support office, and we're going line by line. So that's one.
We are closing unprofitable locations, and that's going to be accretive in the year. We have optimized store hours in certain locations to match with where the local market already is. And I think the other big component of this is we've looked at all the project spend and all the projects that exist across the company. And I think the focus is there twofold.
More importantly, it's how do we focus the organization on customer-focused initiatives so that we deliver more value. But then obviously, reducing the spend on the income statement. So that's on the cost side. Look, on the capex side, I'd say if you look at the trend we've seen, you go back to maybe fiscal '22, I think we were at around $1.4 billion in the year.
We increased to -- this is '21, sorry. So -- and then we went up $300 million. And again, last year was the peak of 2.1. And so what we're trying to achieve here is getting back to kind of the normal levels of capex here, Two parts that are going to contribute into this again is, one, as John talked about, we're very focused in our healthcare segment.
on profitable growth. And so we will see a lower level of capex or growth capex coming out from U.S. healthcare care segment. And then if you look at a couple of drivers of the capex on the U.S.
retail pharmacy, micro fulfillment centers as well as our digital transformation some of those things are coming to fruition. And Ginger talked about taking a pause on micro fulfillment center so that we increase the productivity and achieve the desired results there first. So those are some of the factors, high level that are driving the capex reduction.
Operator
Your next question comes from the line of Kevin Caliendo from UBS. Please go ahead.
Kevin Caliendo -- UBS -- Analyst
Thanks for thanks for taking my question. The 60 clinics that are closing, sort of what was the driving factor there? Why were they not successful? Was it competition in the marketplace? Was it payer relationships? Like why weren't you able to drive volumes in those markets? What happened there? What can you learn from that?
John Driscoll -- President, U.S. Healthcare
Kevin, it's a fair question. I think the way to think about the 60 clinic reductions is that some of them will be closed. In some cases, we're going to transition those to affiliate relationships, but it comes down to how quickly can we unlock profitable growth. And in the Village City Summit, it's about concentration of power and relevance within certain markets.
Every one of our clinics actually shows month-over-month growth, but we don't see the growth coming fast enough in certain markets. And so we're going to pivot there and be very focused on where we can drive the most profitable growth. We're growing through the rightsizing of our footprint and some of the changes in our relationships, but our strategy going forward will be really focusing on markets where we see that momentum and scale and at a level that we want to see to drive the profits and the margin expectations that we want. So it's really more of a discipline around focusing on markets where we can go deep and continue to grow on a compounded serious way profitably.
Kevin Caliendo -- UBS -- Analyst
OK. That's helpful. Can I just ask a quick follow-up on cash flow. Is the right way to think about it? I know you didn't provide fiscal '24 free cash flow, but should we take the $655 million add to $600 million and reduced capex, $500 million benefit in working cap and then adjust for net income? Is that like a rough range of where you think it would -- should come out for fiscal '24?
Manmohan Mahajan -- Interim Global Chief Financial Officer
Yeah, sure. Look, as you understand, as you rightly pointed out, we do not generally provide guidance on the free cash flows. But we have outlined, we do expect significant growth. And what we did here is we've carved out two significant drivers year on year.
But having said that -- and there was -- let me add a third one to that as well. Just on the U.S. healthcare, we are expecting in fiscal '24 at the midpoint of the range to be breakeven on the EBITDA. And when you look at that year-on-year, that is a significant improvement on the cash as well.
Having said that, we're also looking at other offsetting items. So we just want to make sure you have kind of the three -- we do expect significant improvement and you have those three key drivers there.
Operator
Your next question comes from the line of Brian Tanquilut from Jefferies. Please go ahead.
Brian Tanquilut -- Jefferies -- Analyst
Good morning. I guess, John, just a question on VillageMD, right? You're clearly showing some expectation for meaningful year-over-year improvement there or at least the whole Walgreens Health segment. As I think about the fact that you're opening new clinics, how does the J-curve factor into this, right? Because I'm just trying to bridge to that significant improvement when you're opening new clinics, probably you will lose money.
John Driscoll -- President, U.S. Healthcare
Sure. Well, first of all, I think we've essentially stopped the opening of new clinics. But remember, the J-curve really refers most clearly to Village. With Summit and City, we've got consistent growing revenues that balance that a bit and actually help kind of develop -- show a better profit profile.
And then we've got solid growth building quarter over quarter with Shields, CareCentrix, our analytics business, our clinical trials business, and U.S. healthcare. So I think you've got to think about it as a portfolio. The J-curve specifically impacting the new clinics that we are in the early stage clinics for Village, but we've got a lot of other levers to pull or really advantages in the momentum and the margin profile, improving margin profile across the other businesses.
Operator
Our next question comes from the line of Elizabeth Anderson from Evercore ISI. Please go ahead.
Elizabeth Anderson -- Evercore ISI -- Analyst
Hi, guys. Thanks so much for the question. One thing that's been obviously a hot topic this year is utilization. Obviously, you guys have a mixed model that both has fee-for-service as well as value-based care lives.
Can you talk through us how you sort of those inflections in utilization impacting the VillageMD overall -- business overall? And then secondly, can you just comment more generally on sort of any additional deleveraging plans you have for this year?
John Driscoll -- President, U.S. Healthcare
I think on the utilization, utilization is our friend, obviously, at City and at Summit and has been more of a headwind in Village. The good news from a Village perspective is that even with that increasing in utilization post-COVID, that we are, particularly in our mature markets, showing an improved margin profile on our full-risk lives. And so it's -- the way we solve for what's a benefit of having a two-part portfolio is continuing to convert more of those fee-for-service lives to full-risk lives with a better margin profile and optimizing our cost base so that we can get the full value of that improvement in revenues.
Manmohan Mahajan -- Interim Global Chief Financial Officer
Yeah. I think on the question around deleveraging, a couple of thoughts there. Number one, we're absolutely committed to our investment-grade rating. And as we've said, one of the key areas of focus here in the last six to eight weeks for me and Ginger has been cash management.
I've gone through that as to how we're going to drive the improvement there. And last I would point out is we continue to have a portfolio of investments, which we look at simplification and optimizing. That provides us flexibility.
Operator
Our final question comes from Eric Percher from Nephron Research. Please go ahead.
Eric Percher -- Nephron Research -- Analyst
Thank you. I'd like to turn to the topic of labor and ask to what extent you're seeing headwinds from labor cost? And I think there's probably a bit of a reminder on the onetime costs you see on fiscal year '23 versus fiscal year '24.
Manmohan Mahajan -- Interim Global Chief Financial Officer
Yep. Maybe let me start with the onetime costs. So look, we have significant savings here that we're going to achieve in fiscal '24. And obviously, there is going to be a cost associated with it.
But when I look at the cash flow impact in the year within '24, we see a positive impact, net-net, from a cash flow perspective of cost savings initiatives net of the cost associated with it. On the labor cost, yes, look, we have seen investments in the last year and a half. If you think about Q1, Q1 would be the last quarter where we would see headwinds from a lever investment perspective because most of these investments were in place starting second quarter last year. Apart from that, I think normal business course investments and labor will continue.
Operator
And we have no further questions in the queue at this time. Ginger Graham, I'll turn the call back over to you for closing remarks.
Ginger Graham -- Interim Chief Executive Officer
Thanks so much, and thanks, everyone, for joining the call and your questions. We really appreciate the feedback and the support. We are clear on our challenges and our priorities, and we are focused on the future. We're looking forward to your further questions.
So please reach out to our Investor Relations team. Thanks very much.
Operator
[Operator signoff]
Duration: 0 minutes
Call participants:
Tiffany Kanaga -- Vice President, Global Investor Relations
Ginger Graham -- Interim Chief Executive Officer
Tim Wentworth -- Incoming Chief Executive Officer
Manmohan Mahajan -- Interim Global Chief Financial Officer
John Driscoll -- President, U.S. Healthcare
Lisa Gill -- JPMorgan Chase and Company -- Analyst
Rick Gates -- Senior Vice President, Chief Pharmacy Officer
Charles Rhyee -- TD Cowen -- Analyst
George Hill -- Deutsche Bank -- Analyst
Kevin Caliendo -- UBS -- Analyst
Brian Tanquilut -- Jefferies -- Analyst
Elizabeth Anderson -- Evercore ISI -- Analyst
Eric Percher -- Nephron Research -- Analyst