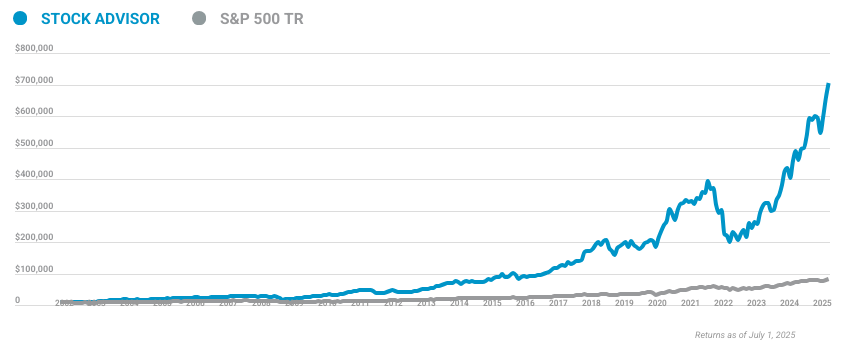
Image source: The Motley Fool.
LHC Group Inc (LHCG)
Q3 2019 Earnings Call
Nov 7, 2019, 9:00 a.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Ladies and gentlemen, thank you for standing by. And welcome to the LHC Group Q3 2019 Earnings Conference Call. [Operator Instructions]. I would now like to hand the conference over to your speaker today, Senior Vice President of Finance, Eric Elliott. Sir?
Eric Elliott
Thank you [Indecipherable]. I'd like to welcome everyone to LHC Group's Earnings Conference Call for the third quarter ended September 30, 2019. Everyone should have received a copy of our earnings release last night, if not, I would like to highlight that we have posted that along with some supplemental information on the quarter and year-to-date for 2019 on the Quarterly Results section of our Investor Relations page. The supplemental deck as well as a copy of the earnings release, the 10-Q, and ultimately a transcript of this call when available can be found on this page. Our supplemental deck includes all of our reconciliations and breakdown of adjustments. We will refer to these non-GAAP measures during our call today.
In a moment, we'll have some prepared comments from Keith Myers, Chairman and Chief Executive Officer; Josh Proffitt, Chief Financial Officer; and Don Stelly, President and Chief Operating Officer. Before we start, I would like to remind everyone that statements included in this conference call, in our press release, in our supplemental financial information may constitute forward-looking statements within the meaning of the Private Securities Litigation Reform Act. These statements include but are not limited to comments regarding our financial results for 2019 and beyond. Actual results could differ materially from those projected in forward-looking statements because of a number of risk factors and uncertainties, which are discussed in our annual and quarterly SEC filings. LHC Group shall have no obligation to update the information provided on this call to reflect subsequent events.
I'm pleased to introduce the Chairman and CEO of LHC Group, Keith Myers.
Keith Myers
Thank you, Eric, and thank you, everyone, for dialing in and participating in this morning's call. Over the last 25 years, LHC Group has reached a number of significant milestones. On September 23, we hit one of our more important ones yet. We reached an average daily census of 100,000 patients.
Our 32,000 team members serving at locations throughout the nation are directly responsible for this outstanding accomplishment. It's a testament to their hard work, dedication and commitment to excellence in all that we do. Their unwavering commitment to providing the highest quality and service in our industry represents many miles, many long hours, providing care 24 hours a day, 7 days a week for the most vulnerable members of our society.
Because of the work they do each day, so many people have been loved, comforted, and provided a sense of hope and a better quality of life. It's quite a responsibility, which we feel we should be part of, and which we fully embrace as a leading national healthcare services organization, committed to being an indispensable assets to every community we are privileged to serve. Growing from a central act of one nurse, my wife, Ginger cared before elderly neighbors on a voluntary basis, before and after the shift at our local hospital 25 years ago to now a leading national healthcare services organization caring 400,000 active daily patients isn't a celebration of the numbers. It's a recognition that everything we do starts with a genuine desire to help people and make lives better through the consistent delivery of high quality and compassionate care to every patient and every family we have privilege to serve.
Our people have always been and remain our greatest assets and their experience and expertise will be critical in the clinical care models we have designed to thrive as an organization under the new PDGM model. So turning to PDGM, last week's final ruling by CMS was a significant improvement for the home health industry compared where we started in the early stages of their real rule-making process.
We are pleased to see that CMS has reduced the proposed prospective payment adjustments based on assumed behavioral changes to 4.3%, a reduction of approximately half from their original proposed adjustment in the proposed rule earlier this year. By doing so, CMS has lessened the burden on the industry and the risk to Medicare beneficiaries who depend on home health services during the transition to a drastically new model that represents the most significant change in reimbursement methodology for more than 20 years, since the Balanced Budget Act of 1997.
This is a positive development for LHC and for the industry and most important for the elderly patients we serve who represent the most vulnerable members of our society. Over the course of this year, we were able to build tremendous support on the Hill with important champions in both chambers of Congress and we spent a considerable amount of time in direct discussions with HHS and CMS leadership which we greatly appreciated.
With respect to the legislation and for the great work to-date to secure support of S.433 and H.R. 2573, LHC and industry secured 1/3rd of the Senate and 13 bipartisan cosponsors and nearly 1/3rd of the house and 14 bipartisan cosponsors.
This successful achievement of such broad based congressional support demonstrates the appreciation and understanding of the value we provide to our healthcare system as a whole and the recognition by Congress of the importance of the value of the care we provide to patients and families in their homes. I want to thank our many sponsors, who have supported the regulatory and legislative changes on the PDGM. We believe their strong support send a clear message of their understanding of the need to preserve access to home health services to all Medicare beneficiaries, particularly in rural areas, which was helped -- which helped to bring a heightened sense of awareness to the issue.
I would also like to thank CMS Administrator, Seema Verma and her staff as well as that of HHS leadership from multiple meetings with us and their willingness to work collaboratively and to listen to our concerns. While we are pleased with the improvement in the final rule, we remain concerned with the lack of transparency, and CMS's use of assumptions to establish payment policy and adjustment.
We urge CMS and the Office of the Actuary to be fully transparent with data used to make any future payment adjustments, so that high quality home health providers in the industry may provide valuable feedback in the construct of new payment policies.
We continue to see value in encouraging CMS to be more transparent in the calculation of payments to providers under the Medicare Home Health benefit, and in our ongoing support for payment reform that is evidence based. We are a big proponent of the focus PDGM places on patient characteristics.
More importantly, PDGM recognized as a critical role that in-home healthcare plays as the most appropriate and most efficient setting for delivering high quality care in the privacy and comfort of the home or primary place of residence of those we serve. This ruling and a couple of others I will touch on also reinforce the importance of accelerating our joint venture strategy and securing our seat at the table with new payer models and value-based arrangements.
While LHC is fully prepared and has completed extensive testing of our clinical care model systems and overall operations to begin to operate under PDGM, the final rule provides a measured approach in the first year that will be of LHC and the industry time to adjust to the new model. The certainty of this approach as presented in the final rule provides LHC with a strong position and clarity for the growing number of patients we serve each day.
Now, I'd like to spend a few moments on the detailed work we have been doing to be prepared for PDGM. There has been a lot of commentary in the industry about how providers will offset the adjustments under PDGM. For some, it's been a financial pathway to living with PDGM. For LHC Group, we've created a clinical pathway to thrive under PDGM. We have an executive clinical leadership team that has been working on PDGM preparedness for almost a year now leading into the implementation of the pilots we talked about on our last call.
On the week of July 15, we went live with our pilot locations. These pilots crosswalk the 153 current payment groups in the new 432 different PDGM payment groups, and looked at how we could improve efficiencies in care delivery, and how we can better manage and care of our patients in order to maintain our industry-leading patient outcomes and satisfaction.
We also tested increasing the use of telephonic teaching and training visits. The care model we developed is patient-specific based on co-morbidities, functional scores and diagnosis. Each category model also represents a frequency that historically yielded the best outcomes for patients with similar characteristics in scores. To ensure we maintain our industry-leading quality, we will be increasing our overall patient encounters.
We will accomplish this by increasing utilization of telemedicine in our care models. The technology, I mentioned a moment ago, proved to be very effective in the pilots. With this new proprietary technology, we are giving clinicians access to best practice benchmarks for optimal outcomes in the palm of their hand at point of service, thus enabling them to make better clinical data driven decisions with [Indecipherable] patient care at the point of service.
As a result, we expect we will be able to deliver care in a more efficient manner and deliver optimal outcome. One last point on PDGM, and it's a big one for our organization, we see these changes as a real opportunity for growth.
We've read of some providers already laying off therapists and cutting back on other clinical staff. We are opening onboarding and training centers across the country in anticipation of this growth to ensure that we have the clinicians necessary to continue to deliver on our high standards of quality care.
PDGM isn't the only big change that is happening in the industry. In late October, CMS also released its final rule on the phase-out of the request for anticipated payments or RAPs starting in 2020 and full implementation in 2021. The RAP has been targeted by CMS and the Hill for some time as part of the efforts to eliminate the on both pay and chase. And it's been a way for many people to get into the business with Medicares financing their business venture. Combined with the 230 day payment periods under PDGM, the elimination of the RAP should lead to more consolidation in the industry than we've experienced in the last two decades. It will hit cash flows hard for the smaller agencies, but for the larger agencies, such as LHC, we would expect minimal impact.
In late September, CMS released its final rule-making changes to discharge planning requirements for home health providers that should make patients more engaged in their care transitions from the hospital to other care settings. This was a long overdue step and the industry welcome these changes.
There are a couple of aspects that are worth noting that demonstrate how well we are positioned to benefit. Under the new discharge planning rules, patients and their families are required to have information necessary to make informed decisions about their post-acute care option including data on quality measures. Home health agencies also required to provide relevant data on quality measures. As the industry's leader in quality and patient satisfaction, LHC Group can be front and center with patients and their families, as well as our existing referral sources.
On October 9th, HHS published proposed changes to the physician self-referral law, commonly known as the Stark Law and to the Anti-Kickbacks Statute. The proposed rules are coordinated by CMS and HHS and OIG. This announcement wasn't as widely covered are discussed in the investment community as recent ruling are for the most part the home health industry. But these proposed rules are some of the most significant changes to these laws in many years.
For LHC Group, they have the potential for positive changes on our joint venture strategy and more specifically to our participation in value-based arrangements. The proposed Stark Law changes will include new exceptions to enable value-based care arrangement and the Anti-Kickback Statute changes would modify existing Safe Harbor, create new Safe Harbors and create new exception. Some of the AKS Safe Harbor changes would be for value-based arrangements, patient engagement, CMS sponsored models and personal services among others.
There are common threads in all of these rules and changes and they are all winners for LHC Group. For one, the shift care into the home and encourage payment models built on delivering value They will also lead to significant consolidation in the industry based on the level of quality patient satisfaction, extent of partner referral relationships, and financial strength. To put a finer point on how much consolidation we're expecting, I will highlight a recent article in the home healthcare views that cited numerous [Indecipherable] industry sources predicting that PDGM and the elimination of the RAP alone will be to the closure of over 30% of existing home health agencies.
For those of you who have followed us closely, we've been able to deliver strong growth over the last few years. When I look at the growth potential of LHC Group for 2020, 2021 and beyond across a national platform that extends across 35 states today and the District of Columbia reaching 60% of the population aged 65 and over, I'm even more excited.
I see our growth coming in many forms. Some of [Indecipherable] selling them right now such as legacy LHC, organic growth, post conversion, Almost family locations and our M&A activity. Others are just beginning to ramp up, such as revenue synergies and growth strategies with Almost Family and our bi and tri-levels de novo growth. And on other such as our managed care relationships, value based arrangements, the ACO business and future consolidation opportunities, we have only scratched the surface of what we can do.
Here's Josh to provide highlights on our financial results and 2019 guidance. Josh?
Joshua L. Proffitt -- Chief Financial Officer
Thank you, Keith, and good morning everyone. Thank you all for joining our call. As always, I'll begin my prepared remarks by saying how much I appreciate all of our clinical professionals across the country and what they do each and every day. It is a privilege to serve you as you tirelessly serve others. I would also like to thank our home office support teams whose level of commitment and service to the field is greatly appreciated.
I am so proud to work alongside and to support you all. It is because of all of your hard work and execution that we were able to report yet another strong quarter of results. I would also like to thank our executive clinical leadership team and our teams in our PDGM pilot locations for leading the way to ensure that our 25-year unwavering commitment to industry leading quality and clinical outcomes remains the number one priority as we approach another new reimbursement model. Our supplemental financial information posted on the website provides more detail on the breakdown among sector performance, guidance and assumptions. I will reference that supplemental deck in my summary remarks this morning. For the third quarter financial results, here are the big takeaways. Revenue across all segments for the quarter met or exceeded our expectations, especially on the Legacy LHC assets. We continue to see slower growth in the AFAM home health assets which we expected due to the continued system conversion that will end in the fourth quarter. Our adjusted earnings per share was $1.26 in the third quarter. These results included $0.05 in tax credits and $0.06 in improved implicit price concession in our Hospice segment due to better cash collections, especially on recent acquisitions.
While the hospice implicit price concession was a benefit to Q3, it brings our annual and prolific price concession amount in line with our annual expectations. Looking ahead for a moment to Q4 EBITDA, to normalize the run rate, you have to adjust the $3 million Q3 hospice benefit and the $3 million we received from our Medicare Shared Savings Payment in our HCI segment that we receive every Q3. When taking each of those into account, we do expect normalized EBITDA growth in Q4. As it relates to EPS for Q4, we expect the tax rate to be approximately 27% to 28%.
Now, back to the third quarter highlights. Incremental margin improvement has continued across our hospice and HCBS segments on a year-over-year basis. Organic growth continued to lead the way for us with an 11.1% increase in home health admissions excluding AFAM. Our industry-leading quality and patient satisfaction scores were the main factors here as well as the incremental growth we've generated from previous acquisitions and joint ventures. In addition to the accelerated growth, we anticipate from PDGM disruption in the marketplace that Keith discussed earlier, another significant incremental organic growth opportunity as we head into 2020 is of course our expected admissions acceleration from the Almost Family locations.
In the 130 Almost Family locations fully converted to LHC Groups instance of Homecare Homebase prior to the third quarter, we demonstrated sequential organic growth in home health admissions of 1.2% in the quarter as compared to the second quarter despite the fact that Q3 is typically a seasonally lower volume quarter than Q2. Another very positive trend in AFAM admissions growth is that sequential same-store growth from Q3 2019 to Q4 2019 is currently pacing to be approximately a positive 2%
growth as compared to a negative 3% from Q3 of '18 to Q4 of '18 as we are winding down our system conversions.
Turning now to Page 8 of the supplemental deck, I would note that our adjusted consolidated gross margin of 37.3% in Q3 was a 30 basis point improvement year-over-year and a 100 basis point improvement through the first nine months of 2019 versus 2018. Consolidated adjusted G&A expense as a percent of revenue was 26% in the third quarter, which was down 150 basis points from the 27.5% in the same period a year ago, and down 130 basis points from the second quarter of 2019.
Our adjusted consolidated EBITDA was 11.3%, which is up 170 basis points year-over-year and up 110 basis points from Q2. This improvement across all metrics continues to be broad based. Pages 10 through 16 of the supplemental deck highlight the results and Page 6 notes the key stats by segment.
Of note, I would particularly like to briefly highlight the improvement we have continued to experience in each of our hospice and HCBS segments. With regard to hospice for the first nine months of 2019, we are now delivering a 12.3% EBITDA margin, which is attributable to lower G&A expense, solid volume growth in 2019, and improved cash collections on our hospice receivables. In regards to our HCBS segment, we are pleased with our 7.2% EBITDA margin in the third quarter, which was driven by improvements in gross margin and G&A expense.
Turning to Page 21 of the supplemental deck, we've outlined a number of our debt and liquidity metrics, including the fact that adjusted free cash flow was $108.6 million for the nine months ended September 30. DSO's were slightly up in the third quarter to 50 days from 47 days in the same period a year ago due to a build up of AR in recent home health acquisitions.
However, we fully expect to collect on those receivables once the channels are in place and for DSO's to remain in the 45 to 50 day range that we previously projected for DSO's in 2019. Today in 2019, we have either completed or announced acquired annualized revenue of $86.7 million through joint ventures, both new and extensions of existing partnerships, as well as strategic acquisitions and tuck-in acquisitions.
Our earnings release highlighted these recent transactions, including the continued extension of our relationship with Life Point Health that has been a source of significant growth for us since the inception of our systemwide partnership we entered into in 2017. This latest announcement with LifePoint represents the beginning phase of bringing the former RCCH home health and hospice assets into our LHC Group LifePoint partnership. We cannot be more pleased with how our partnership with LifePoint Health has progressed from 30 locations with annualized revenue of approximately $70 million in 2017 to now 49 locations with annualized revenue of over $120 million today.
As Keith alluded to earlier, the impact of PDGM is expected to create a historic opportunity to consolidate the home health industry in 2020 and beyond through higher organic growth from market share gains and through inorganic growth acceleration. With the M&A environment expected to heat up and our value proposition expected to become even more compelling among our partners and potential new partners, we possess a strategic asset in our capital structure and available liquidity. Net leverage at quarter end was 0.93 times adjusted estimated EBITDA for 2019. With over $245 million available on our credit facility and an accordion feature that can provide an additional $200 million of capacity, we are well positioned to remain in growth mode.
As you noticed, we are increasing our EPS guidance for full year 2019 to a range of $4.35 to $4.45 while affirming our revenue and EBITDA guidance. The increase in EPS guidance is mainly due to the tax credit, as well as our improvement in hospice and HCBS margins that I spoke of earlier. The details of this guidance are on Page 17 of the supplemental deck. At the midpoint of this range, we are expecting adjusted EPS growth of 23.9%, net service revenue growth of 16.9%, and adjusted EBITDA growth of 34% as compared to last year.
Turning now to a few brief thoughts on PDGM. As we have mentioned in the past, we fully believe and reaffirmed with our pilot locations that we can offset around half of the revenue impact from the previous 8% cut while offsetting the rest with our cost reduction initiatives. Now that the behavioral adjustment has been reduced to 4.3%, we believe we will mitigate the cut from a revenue standpoint and have EBITDA upside related to our cost reduction initiatives. In summary, the key components of our growth story remain intact. LHC organic growth continues to exceed our long-term targets with market share gains built on
quality and patient satisfaction differentiation.
Post-conversion growth at Almost Family home health locations is ramping up and generating the growth we anticipated, and our de novo growth strategy is also accelerating.
Combined with the strong momentum in our joint venture partnerships and a robust acquisition pipeline, we are well positioned to capitalize on the significant consolidation that PDGM and the elimination of the RAP payments will bring in an industry that for now remains largely fragmented.
We are excited about the potential we have for LHC Group to capitalize on the potential market share that will be created from this consolidation. That concludes my prepared remarks, and I'm happy to answer any questions during Q&A. I'm now pleased to turn the call over to Don.
Donald D. Stelly -- President and Chief Operating Officer
Thank you, Josh, and good morning everyone. No doubt, we are where we are today because of the hard work and commitment from our 32,000 team members who care for patients and families that we are privileged to serve each and every day. Simply put our heartfeltly thank you for all that you do.
In my time this morning, I'd like to focus on organic growth at LHC legacy locations as well as the recent converted Almost Family locations as well as a little detail on the clinical pathways that we've taken to prepare for the PDGM changeover. Our organic growth continues to exceed our long-term targets with home health admissions up 11.1% for the quarter and 8.6% for the year, and hospice admissions up 2.1% for the third quarter and 5.9% for the year.
This growth, which we have typically targeted [Indecipherable] improvements made to the home and community-based services businesses earlier this year that we talked about. From our segment results on page 14 of the supplemental deck, you can see that our home and community-based services segment adjusted EBITDA margin was up 460 basis points from last year and up 170 basis points from the second quarter. We do expect the improvement in this business line to continue.
Our quality scores, which are outlined on Page 20 of the supplemental deck, we continue to see strong same-store LHC quality scores in October at 4.65 and Almost Family improving to a quality score of 3.82 in October as compared to 3.78 in July.
As of today, 87% of the Almost Family home health locations have been converted to the LHC Group instance of Homecare Homebase and have completed with the conversion of the payroll process in these coordinate with Lawson. As Josh noted earlier, we are seeing an incremental growth to the fully converted locations and definitely expect to see more to the balance of this year and into 2020. Together with the incremental improvement in the quality scores for Almost Family, we are now moving to the stage of capturing revenue synergies from this acquisition.
There is one final but important aspect of PDGM that I want to cover, and that's how we execute everything that Keith and Josh mentioned from a clinical perspective, and at the same time, maintain our high standards of quality and clinical excellence. The answer lies an increase in patient encounters and touches while becoming more efficient with our home visits. We have proven this to work in our pilot locations with quality metrics, improving or remaining consistent since of our high now. I cannot say enough about the clinical team and the painstaking process that we went through all 432 clinical groups under PDGM to develop these best pathways for each patient that we're going to care for. For the last year plus we said that we will be ready for PDGM no matter what and we are. We are ready from a clinical perspective to ensure that patient encounters will actually increase with the right clinical protocols and models of care that have been tested in the pilots that we've mentioned.
We are ready with a highly motivated and committed team to ensure that quality and patient satisfaction will continue to lead the industry and fulfill the critical need that patients, families, and hospital partners know is best met through in-home care. And we're ready for what we believe will be a historic opportunity for market share gain and consolidation that even us has not seen in the last two decades.
Again thank you to all of my LHC Group family colleagues and thank you for listening on our call today. Latif, we are now ready to open the floor for Q&A.
Questions and Answers:
Operator
Thank you. [Operator Instruction]. Our first question comes from the line of Brian Tanquilut of Jefferies. Your line is open.
Brian Tanquilut -- Vice President, Healthcare Services Equity Research
Hey, good morning guys. Keith, I guess my first question for you, as I think about Almost Family, it seems like the growth there is still a little bit negative, but shows an improvement in the ones that have seen the conversion. If you don't mind just walking us through how do you think the growth will progress over the course of the next 12 months? And then what is it that happened with those 130 locations? Just qualitatively if you can share with us what changes happened as you converted that drove that upside over Q3 versus Q2?
Keith Myers
Don, you want to take the first part?
Donald D. Stelly -- President and Chief Operating Officer
Yeah, this is Don. I think first of all, we all along, we talked about the conversion to this instance being a distraction and it was. I mean you got to think in these agencies they're already taking care of patients and doing the day-to-day necessity and then we add this on top of it. But the real answer lies in the quality improvement, the clinical processes, because we have to remember, other than our internal benchmarks, which we use with SHP, the quality results that we report are in arrears. But the referral sources, the physicians, the hospital partners see it concurrently. So we're having a much better product for sale number one. Number two, with that conversion behind us in the sales force having the product and having the metrics that we overlay, there is much greater efficiency and proficiency in the sales cycle. So you add those two together and that's what we're seeing and I think it really gives us a lot of confidence that we're going to bode in 2020.
Brian Tanquilut -- Vice President, Healthcare Services Equity Research
That makes sense. And then I guess, Josh, as I think about the margin performance in the home health business, is there anything you would call out as I look at the gross margin line declining 90 basis points year-over-year?
Joshua L. Proffitt -- Chief Financial Officer
Yeah, no, Brian. Again, thanks for the questions. Nothing I would call out, I mean the 90 basis points year-over-year is just your typical wage increases, merit increases. things of that nature on the gross margin line. I'm very pleased that we're still able to leverage more of our G&A and our back office infrastructure and deliver an almost 11% EBITDA margin which is consistent from year-over-year period. And that's a really good EBITDA margin for our Home Health segment. As we highlighted, other segments continue to grow, but to be at around 11% EBITDA margin for home health, we feel really good about that.
Brian Tanquilut -- Vice President, Healthcare Services Equity Research
And then my last, I'm sorry, go ahead.
Keith Myers
Brian I could just chime in on that you know that thinking back of the whole history of LHC, certainly from the time we went public in 2005 to now, that's been a consistent theme all along. We've always, we've always had a little more of our dollars going to the patient care level and have done a better job of controlling G&A. I mean it's a -- I think that will just always be the case. We're very much a clinically driven organization, and so we've from the very beginning, even before we went public, when I was trying to manage finances and Ginger was managing the clinical team, trust me, the priority was spending dollars in the clinical team at the bedside of patients. So I just think that's, that's where we are. But we do a good job of controlling G&A and we're going to continue to do that.
Brian Tanquilut -- Vice President, Healthcare Services Equity Research
No, that's definitely true. I guess my last question Keith, as I think about your comments on PDGM and sort of the efforts that you're putting through to prepare for that operationally, does anything change with the cut being cut in half in terms of your views on the pace of mitigation efforts that you're putting through or the change you're putting through, and then are we changing the strategy at all in terms of the cost or revenue mitigation efforts that you've contemplated?
Keith Myers
I mean it's just, it's a simple no Brian, I mean it doesn't change anything. The only thing -- I guess the only thing it changes for us is in all the areas around the things we're doing on innovation especially payer innovation to prepare to be, to more quickly move to more value-based type arrangements, I mean those kind of investments. That's what allowed us to do, but the clinical model is down alluded to earlier. That was a year-long process and if that had everything to do with going to 432 categories and 230-day payment models and that's the same playbook regardless of what the outcome and the rule would have been.
Brian Tanquilut -- Vice President, Healthcare Services Equity Research
Alright. I appreciate it. Thanks Keith.
Operator
Thank you. Our next question comes from Joanna Gajuk of Bank of America. Your line is open.
Joanna Gajuk -- Bank of America -- Analyst
Thank you. So just to stay on this topic for just a little bit more, PDGM in terms of your preparations, how quickly I guess can you just kind of phrase to us versus how you were talking about this last quarter in terms of how quickly you can adjust things around staffing or how do you think about any changes to utilization of visits per episode? I appreciate your comment about using more telemedicine to help with patient, patient I guess facing visits. So can you kind of frame for us how do you think about all these changes pacing into 2020 now? How quickly you can make these changes in terms of the staffing and any other changes you plan to make?
Keith Myers
Yes. That's a great question. Thank you Joanna. It's Keith. I'll just start with a few high-level comments and Don and Joshua, they'll chime in. So I mean I would say that we're as fully prepared as as I could imagine we could be at this point be implemented. And that's because in January, we were, we were absolutely certain that PDGM would be a reality and and we were certain about -- we were certain that we would see 30-day payment periods and we're certainly would see the expansion of the categories. So we went -- we accepted that and went to work with the development of a drastically new model that we've not changed this significantly in over 20 years as I said in my prepared comments since [Indecipherable] 97.
So we were switching to that model. We prepared for it, we piloted and we're ready to deploy it. The only unknown was what the rates would be for the model, but we knew what the model would be. So that's how I would say about it. So we've -- all of the training and education for the deployment of that model and I mentioned the new technology in our proprietary model, now, it's going to, it's going to put the benchmarks in the hands of the clinicians in the field, at the bedside. All of that training and deployment is already under way, so we weren't waiting for the final rule to do any of those things. So Don maybe you first and Josh?
Donald D. Stelly -- President and Chief Operating Officer
Yeah, it is a good question. I'll go back to what I said on the last call. And here's the why we think that by mid-2020, we are fully deployed and how we're going to mitigate all of the things to the clinical model. That does not mean we're not going to begin in January, but first you know, Joanna, as that you've got crossover episodes that are already in play right there, those care plans, etc. So when you're going to reassert or when you do some of those things, there's some of that behavior that will transfer on. Number two, Keith talked about the readiness to deploy the education and training and that is a fact. But there's also a balancing act operationally because both Keith, Josh and myself talk about 32,000 people out there need to perform this education, be deemed competent and really get an understanding. At the same time, we're also balancing things like SWB and G&A. So all told, as I said last call, I'll reiterate we're fully ready and we're fully committed to the deployment. But it's going to really take hold and gain steam somewhere around April, May and June. Josh?
Joshua L. Proffitt -- Chief Financial Officer
Yeah, no, Keith and Don you both really summarized it well. The only thing I would maybe highlight is Keith referenced the training that has been going on and the feedback that we have been receiving here at the home office from
Donald D. Stelly -- President and Chief Operating Officer
from the trainings that have already occurred throughout the country has been extremely positive. So the receptivity to the clinical focus and the clinical pathways that have been developed and are being deployed has really been a great thing to see which gives us even more confidence, that as you start going through next year, you're really going to see it picking up in Q2 and as Don alluded to, I'd say the back half of the year we'd be fully deployed.
Joanna Gajuk -- Bank of America -- Analyst
Okay. And then just to close that topic on the RAP reductions or I guess in 2020, what the impact would be to your cash flows in Q1?
Joshua L. Proffitt -- Chief Financial Officer
Yeah, Joanna, great question. The impact, I think I talked about this on the last call, but just maybe touch on it again. Cash flows will be impacted really in the first quarter, probably call it January through March, maybe with an increase of DSO's around five days or so. And then heading into the Q2, it would get back to a normalized level.
So for us, we don't envision any issues from a cash flow perspective just because of our size and the strength of our balance sheet. And only five days of DSO's isn't going to really make that big of a difference. However, when we talk about the impact of some of the smaller folks in the industry, that will definitely continue to accelerate the consolidation that Keith and I, both talk about in the prepared remarks.
Joanna Gajuk -- Bank of America -- Analyst
Okay, great. So I just want to make sure there's no updated views there. So thank you for these comments on PDGM. And just the next I guess topic next for home health in terms of contracting with Medicare Advantage plan. So any update there in terms of any incremental, I guess contracts you enter into any update on those that have been running? And kind of to wrap it up, can you just talk about the sort of the delta between the MA rate versus fee-for-service, with that you currently seeing any kind of rate increases going forward? Thank you.
Keith Myers
Sure. Thanks, Joanna. And I'm glad you brought this one up. I didn't know if the whole call would be PDGM and growth for next year, which we are extremely excited about both. But I'm happy to speak about our continued efforts on the managed care front. We have continued to have those conversations as I've alluded to on each call, it's a journey and there is not a light switch or anything that's going to flip overnight.
But incrementally, we do continue to see rate improvement even in just our contracts that were either newly negotiating or updating. And that's just on the base rate so that gap you alluded to between Medicare and Managed Care continues to shrink. And I think I've mentioned this before, but we are probably somewhere between 8% and 10% rate increase from around 2015, '16 to where we sit today, just in our average rate per visit. We're also better marginalizing that business which I've talked about in the past where we've got lower bad debt on that business, as well as just leveraging G&A and better operationalizing it at the field level. On the more value-based side, we have entered into two more pilots since our last call that have value-based parameters around them, and we've also increased the number of preferred provider agreements that we have entered into with ACOs across the country, up to now around 40 of those. So we've got a lot of activity going on in that area.
Operator
Thanks for the Sky, I appreciate. I'll go back to the queue. Thank you. Our next question comes from Scott Fidel of Stephens. Your line is open.
Scott Fidel -- Stephens -- Analyst
Hi, thanks, good morning. First question, just was hoping maybe to get some more meat on the bone or just sort of clarity on the comment in the press release in terms of the growth acceleration that's expected for 2020. I know that you highlighted a number of different tailwinds around growth that you're expecting during the prepared remarks but, but maybe just to specify around that, is there any specific sort of framework in terms of revenue growth, EBITDA growth, organic growth, sort of M&A or just sort of all these different factors? Just want to make sure I sort of fully explain that -- understand that comment in the press release.
Keith Myers
So, yes. So this is Keith. I'll take that. So that comment was really speaking to M&A growth and and market share growth in existing market. The contributing factors to that are of course the the prediction by industry consultants and experts as like to consensus out there that belief that approximately 30% of the roughly 12,000 providers are likely not to survive under the new PDGM rule, given the elimination of RAP which is -- which usually impacts small providers. I mean to the point of they depend on that for their financing, but then also all of the complexities. So we think the -- when that, when that market consolidation occurs because of our quality scores and reputation in the industry and all those things combined, we think we are well positioned to pick up a significant portion of that disruption in patient flow.
With regard to M&A, the providers that don't, that don't close our go out of business are more interested in exploring alternatives of perhaps selling and where they find a good home for their people. And some of the people who were previous owners and some of these agencies quite often, I mean I don't know if it's 50% of the time, but I would bet it somewhere in the 40% range or so, they come on as an employee of LHC in different roles. They're experienced leaders in the industry.
So that's all part of consolidation. That's slowed tremendously for us in 2019 because of the uncertainty. They didn't know -- they didn't know what their financial picture would look like in 2020, and we couldn't negotiate based on trailing financials because we didn't know how to model going forward. So this closure around PDGM brings clarity to all those -- all of those things. So we have -- there are a number of transactions that are in our pipeline so to speak, that we've had deep discussions with, but we're on hold for because we couldn't come to terms on pricing. So now that barriers out of the way. So I believe that we're going to see record growth in both those areas, especially in M&A over the next several years and I would wrap this part up by saying there's evidence to support that. So I'm a big data guy, and if I look back at the history of LHC Group, there is a significant spike in M&A activity in the two to three years following a significant change and reimbursement like this.
And this one is the most significant we've seen since BBA 97. The change of BB BBA 97 led to our public offering in 2005. So that's how significant these things can be so Don or Josh, you all want to add?
Joshua L. Proffitt -- Chief Financial Officer
Yeah, Scott. This is Josh. The only thing I would add, so Keith did a great job of highlighting the PDGM and its effect and then the M&A pipeline. I want to double down and highlight AFAM, which we talked about in our prepared remarks. When we wrap up the conversions toward the end of this quarter and go into next year, not only with the quality momentum that Don spoke about earlier, but we're already seeing the evidence of the growth momentum as we put some nuggets out around the sequential growth quarter-over-quarter, not only in the agencies that converted, but also just in the whole book of business. I think you're going to really see some good growth and Almost Family in 2020 that will continue to bolster our overall growth for next year.
Donald D. Stelly -- President and Chief Operating Officer
Yes, Scott, just the last comment on that. I mean if you look back, remember, even prior to the merger, Almost Family hadn't grown in quite some time. So we've got the agent population, the lack of growth that lead us to a real high level of confidence that we can go grow these things.
Scott Fidel -- Stephens -- Analyst
Got it, understood. Thanks for all that color. And then my follow-up question, just on the hospice segment. Just I was hoping for some color on a couple of drivers told to get the revenues around the $3 million of benefit from the implicit price concession. Maybe can you talk a bit about sort of what you're seeing on length of stay trends? it seems like those might be rising over the course of the year, but just want to clarify that. And then on the cost of services, it looks like that's been down nicely year-over-year. So maybe just on length of stay and cost of services, sort of underlying trends there and sort of what sort of organic and what's being impacted by M&A and that's it for me. Thank you.
Keith Myers
Well thanks, what's been impacted by M&A. I'll throw that to Josh because you're spot on there. What I would say in short, is on the legacy side, we've not seen a lot of that change because we still have the same nursing home versus non-mix as well as the GIP side. So from a model standpoint, that's not going to move the bar a lot, but you just talked about M&A and Josh I want you to enlighten there.
Joshua L. Proffitt -- Chief Financial Officer
Yeah, no, a very, very intuitive question and as Don mentioned our based length of stay for our kind of core hospice patient population, if you will, is not changing, the change really lives in -- and I think we've talked about this in the past, but in a lot of our recent acquisitions, especially in our joint ventures with hospitals and health systems, if the majority of their hospice patient population were coming out of their systems at the time we joint ventured and they didn't really have a growth strategy out in the marketplace, you tend to have a lower length of stay for hospice patients that come out of hospitals.
So we continue to take those patients as appropriate, but have also then gone out and added feet on the street with new sales efforts to grow other hospice business and it's a different patient type that you get from the market which typically would have a little bit longer length of stay. So I think you've got that dynamic in place as well. But I do want to just overall tip my hat to our hospice operations team. We've been talking about incremental improvement in hospice margin for the better part of the last probably 18 months or so, and we hit a good milestone earlier this year at the 10% EBITDA margin mark, and we had been signaling to you guys that the goal was to get it to 12% or above. And now that we're there over the first nine months, I just want to recognize everybody's hard work and effort that have contributed to making that happen.
Scott Fidel -- Stephens -- Analyst
Got it, thank you.
Operator
Thank you and next question comes from Justin Bowers of Deutsche Bank. Your line is open.
Justin Bowers -- Deutsche Bank -- Analyst
Hey, good morning. So just a two-part question on kind of PDGM. One, Keith, can you just give us a sense of some of the dialogue that you're having with Congress and some of the constituents of the partnership post the rule? And then part two, is just operationally appreciate all the color on the pilots. Can you just tell us about some of the things you're seeing in terms of -- or some of the outcomes you're seeing in terms of quality and then also maybe put some brackets around the cost savings on those sites since July?
Keith Myers
Sure, I can certainly take the first part, and I'll ask Don and Josh to help out in the second part. So we're still early in the process of digesting the final rule from CMS as I said in my prepared remarks. So we are pleased with the improvement in the reduction. And because of the relief, if you will, that it gives the industry in working through this adjustment to this is drastically different model for home health. It's hard work to digest this. I mean we said we've been working on this a year and and we've poured a lot of resources into that this year, and we'll be doing teaching and training next year. I think it's hard for me to even understand how a smaller provider would begin to prepare for that. And as an industry advocate, I mean of course we are an LHC advocate, but have been in this so long, I consider myself an industry advocates. So I think about how it affects all of our colleagues that are smaller. So I say all of that to say that so while this provide some relief, we're still grappling with the issue of assumed behavioral changes that are not based on evidence and are not transparent where we have data that we can analyze and understand how CMS gets to -- gets to its conclusions around reimbursement. And we're concerned about future changes in reimbursement if that same approach is used. So all of the sponsors that have stood up in such strong support for the home health industry are concerned about that very thing with us, and so we're thinking through ways that we might advance something that would protect the industry from those type of changes being made in the future.
I want to make a real strong point to say that I don't want what I just said to be interpreted as reluctance or resistant to change. I mean changes is inevitable. Change is good and necessary when done in the right way, and we participate in anything were invited to participate in by CMS on technical expert panels and we love having dialogue and bringing the benefit of our experience to the table. And I so appreciated that in this process from administrators, Seema Verma and all of her staff. And so we'd like to see continuation of that more transparency, more involvement, so that we can further perfect the reimbursement methodology, protect the Medicare Trust Fund and at the same time not put those we serve at risk by overreaching or doing something that we later regret.
Donald D. Stelly -- President and Chief Operating Officer
So Keith, now I'll follow on with the quality question and Josh, you can go with the financials. First, let me ground you, remember in my prepared comments I talked about LHC legacy being at 4.65 and that our pilots were either improving or staying the same. I want to make sure that we believe that and you know that staying the same is a very good thing because if you're a 4.5 or 5 star agency, the ceiling is near and the ground quite far. So you don't want to fall back. And so as such a high performing organization, we are looking at this in two domains. One is inner episode when a patient gets admitted, does the patient get better from which the primary emission disease was in fact there.
In other words, if they couldn't walk because of a total hip or they're getting better and those outcomes demonstrable of increased activity. That answer is yes, and across the spectrum for what those patients have been admitted. But the bigger that we're focusing on is emerging care, rerehospitalization, acute hospitalizations. That actually is coming down, which is an embedded star, if you would, inside of the overall star ratings. So from my quality perspective, let me put a bow around this. We first if we are 5 star agency have to ensure that the things that we do and how we do it don't put us further back and that is in fact happening.
And then lastly, especially with what Keith and Josh talked about about going at risk and value-based programing, we have to prevent non -- unnecessary emerging care and that's also happening. The key Josh will talk about is, we're doing it in a very efficient manner. So, Josh, go to the financials.
Joshua L. Proffitt -- Chief Financial Officer
Yeah. Justin, and I'll try to be brief on how to respond to this part. As we said, the pilots have been going on since mid-July. So you're only three or four months in and as we've alluded to, even as we go into next year, it's a gradual improvement from the financial perspective. So we're seeing evidence of that which is what gives us so much confidence to say some of the things I did in my prepared remarks about offsetting the cut and having margin expansion.
So don't want to give any specific nuggets because if you think about the four pilots, we chose those very deliberately. You've got certain ones in urban markets, rural markets, high therapy locations, lower therapy locations. So the learnings we've gained from that are, we will be able to extrapolate across the company for purposes of not only our budgeting for next year, but for when we issue guidance. But we're still and month four of those pilots and harvesting those learnings. So I would just tell you, we've got the confidence that there will be margin expansion and more to come on the details.
Justin Bowers -- Deutsche Bank -- Analyst
Got it. I appreciate. I appreciate that color. And Don. Yeah, I mean I think it's, from the outside it's definitely difficult to appreciate how hard it is to maintain those scores when the bias is definitely toward the lower scoring facilities or at least the gains that they can make. But, OK, so -- and then just a quick follow-up, the organic growth numbers and home health just been impressive and grow and just expanding sequentially this year.
So just trying to get a sense of what -- are you guys seeing anything in the market like are we already seeing like some impact from PDGM in terms of some of your competitors out there in the market?
Just trying to get a little sense, a better sense of of kind of what else is driving the gains or if that's having any impact, and I'll leave you with that.
Keith Myers
Yes. So it is having, it is having so the consolidation of market because of PDGM. We are beginning to see a slight impact. So I don't, I never like to say those kind of things without giving you evidence to support it. Our Rev Cycle, the department reported to be -- I first heard this a couple of months ago that there are, there are small consultants that do billing or billing and collections for smaller home health agencies around the country, but there are some in our region. And Kimberly see more that runs our Rev Cycle department, came to me and said that she was -- she was having the opportunity to pick up some really good staff members from some of these smaller billing organizations that were reaching out to her to ask if she had positions because they had really good people and they were planning to either reduce the size of their staffing or some closed their doors because their smaller clients were telling them that they were planning to either sell or shut down in the fourth quarter as a result of PDGM just being too much.
So that was a, that was a very real signal that is actually happening. So she is picking up some of those quality people. And so I don't have that level of detail direct contact why some of the shift is happening in the field where we see our locations picking up market share, and we see that incrementally trending month-over-month in a direction. But there is -- I think there is, there is also a movement within referral sources, especially hospitals and health systems of a narrowing of networks around quality providers and not just in terms of star ratings around rehospitalization rates and those things that affect the financial performance and potential penalties in hospitals. I just think all, all of those, all of those things are becoming important at the same time that we are having a rule that's going to cause consolidation in industry.
Justin Bowers -- Deutsche Bank -- Analyst
Got it. Thank you. Appreciate it.
Operator
Thank you. Our next question comes from Matt Larew of William Blair. Your line is open.
Matt Larew -- William Blair & Company -- Analyst
Good morning. I appreciate squeezing in. Just wanted to actually follow-up on the pilots again and ask a little bit more, if you could give us detail in terms of what it looks like in a pilot practice that sort of care at those pilot locations versus the control in terms of how you're deploying the telemedicine and telephonic interactions with technologies you're deploying? And then, give a sense of whether this will increase or decrease your total cost per episode?
Donald D. Stelly -- President and Chief Operating Officer
So this is done, it's a really good question. So let me take you back. The first thing that we did, when we mapped over the patient characteristics in PDGM to the existing population is look at, what did we do for those patients in today's world that led to the outcomes we're experiencing. Once we looked at that. For example, did we teach and train, did we [Indecipherable], did we change medications, did we ambulate of patient who couldn't walk. Next, we said how often do we need to do that statistically to correlate to the outcome.
And then last, how can we do it, and for what discipline must go out? So the pilot locations and what we've alluded to have higher touches, whether it's through telephony, with the telephone, teaching and training, whether it's in telemonitoring, whether it's through other adjunctive methods that I kind of not like to go out there right now, because, it's going to be a competitive advantage for us. And then, the skill mix in the disciplines.
When you add all of that up, we are touching the patient more so than we ever have. So that gives us the confidence that we've talked about in our call. But of course, we have to do that in the most efficient manner in it it's not increasing cost. Josh was very careful not to go out with a number, but our first goal was to mitigate all of this in a net neutral fashion. And that was, when we were looking at 8%.
So when you wrap all that up, we like where we are and again even offline we can get more granular if you need to give you specificity. But the bottom line is, it looks different because not, it's no longer-centric to just visiting a patient and stepping inside of the home.
Joshua L. Proffitt -- Chief Financial Officer
Yeah, Matt. This is Josh. We've talked a lot about substitutionary types of visits and that could be substituting a tech or an aid for a PT or a PTA today. That could be substituting a teaching and training with more telephonic touches and encounters as Don's describing. So each of those levers that you pull, have a cost reduction component to them. So I definitely want you to make sure that from the financial standpoint, in the margin expansion standpoint, that's where that's coming from.
Matt Larew -- William Blair & Company -- Analyst
And thanks for that. And I have to imagine that these, the capabilities and the new approaches to episodes you're developing have to be of interest certainly to you at this point but eventually to payers. That's a point, your ability to incorporate different skill levels, technologies, capabilities and to driving down cost of care while improving your quality.
Keith Myers
Absolutely Matt, I mean from -- the conversation is finally maturing to one where you're discussing total cost of care. I'm glad you just used that phrase. And in order to do that, the managed care payer can no longer just pay you per visit for every time you walk in the front door. They've got to start allowing us to utilize technology and some of these other things that we are starting to have some evidence based results off of that will really go toward being able to go negotiate more pilots and more opportunities with them, because when you're having those conversations, they want to see some level of evidence that you've done it before and not just a trust me approach. So the PDGM efforts that we're using will also very much so play into that progression.
Matt Larew -- William Blair & Company -- Analyst
Okay. I appreciate it. Thank you.
Operator
Thank you. Our next question comes from Frank Morgan of RBC Capital Markets. Your line is open.
Frank Morgan -- RBC Capital Markets -- Analyst
Good morning. I'll be brief, I know this is a very long, but just for the record, since you've gotten this somewhat of a relief in the final rule, are you going to pursue or is this legislative approach is this officially dead now?
Keith Myers
I wouldn't, I wouldn't say it's officially it's officially there. So I think there is a, there is a possibility that the legislation might be modified and might move forward, but more targeted on how future reimbursement changes or may specifically around transparency and being more evidence based, and things that -- I'm not sure if that, if that, if that's going to be the direction our if legislations are moved forward. 'I'm only -- I'm only saying that those are the discussions, I'm hearing about that are ongoing now, just trying to decide, because there was -- the good news about that is that we had such strong support and such clear understanding of the issue by leadership and by top leadership on both sides and by leaders within the different committees that they're concerned about it and they are concerned about are we going to be facing the same type of thing again next year.
So no decisions have been made. But those conversations are ongoing. And I would imagine within the next several weeks, we will have some direction of where they want to go. I'll just close by this we're really blessed to have this strong support and who are we to now go and say to them to pencils down. I mean this is still a serious issue. We have relief from the cuts but the underlying problem still remains and if their ability-if CMS has ability to make these type of changes without evidence or transparency of process.
Frank Morgan -- RBC Capital Markets -- Analyst
One more on PDGM, just I think you called that 5 days of DSO's. One of your another competitor hits it something in that range around 6 or 7 days, and then we've had sort of an outlier number of 20, but it is the 5 days to 6 days that you're talking about is that, assuming kind of a perfectly frictionless transition and could that DSO number actually be higher? And is that in 5 days of that roughly $28 million to $30 million bucks?
Keith Myers
Yeah, Brian, that's about right, and frictionless. I guess that's a good way to put it. I would say that based on how we expect this to roll out and for the government and others to be prepared because you've got not only the governmental payers but certain other players that are going to be rolling through as well. So I mean if there is some significant hiccup from their end on their systems, obviously we're not making that in. But if that's the definition of friction was then, yeah, I would say that's probably the way we're modeling it.
Frank Morgan -- RBC Capital Markets -- Analyst
Got you. Okay, one last, a non-PDGM question. Just I don't know if you call this out, but in terms of this new joint venture rolling in the regional care facilities or agencies, did you size up what maybe the revenue opportunity is and the growth opportunity is there? And I'll hop off. Thanks.
Keith Myers
Sure. The one that we press released earlier this week is a little over $3 million in current revenues. There's three locations. And then there is a few more that will be coming on the heels of that. Hopefully, we'll be able to announce and discuss here in the next month or so as we get closer to finalizing the addition of those into the fold. So not a significant immediate revenue, but if you look at how the LifePoint assets have been growing since we've brought them into the JV, as with most, we think there are some real upside in growing these as well.
Frank Morgan -- RBC Capital Markets -- Analyst
Thank you.
Operator
Thank you. Our next question comes from Whit Mayo of UBS. Your line is open.
Whit Mayo -- UBS -- Analyst
Hey, thanks. I'll just keep it at one given that we're well over the hour mark. How much EBITDA do you think that Almost Family contributes this year, just in the home health segment, either with or without synergies? Just trying to put a finer point on this question.
Joshua L. Proffitt -- Chief Financial Officer
With -- this is Josh. With synergies that would be hard for me to try and come up with off the cuff here because a lot of our margin expansion throughout the whole business this year has been the realization and acceleration of our synergy capture. If I think about just at a-a segment level, AFAM's $140 million, $145 million of home health revenue and if you applied a 10% to 11% EBITDA margin, those assets still aren't quite probably at the full 11 that the rest of the business is running. That would give you a kind of a range from a EBITDA margin contribution from AFAM,
And then when you look at the HCBS segment, I mean that's almost all exclusively all AFAM because our HCBS segment was relatively immaterial prior to that. So all of that margin is directly attributable to AFAM.
So I guess, long-winded way of saying it really has been a major contributor to our success story this year from a margin perspective, and then I'll triple down, since I doubled down earlier on the growth trajectory and increased contribution from AFAM into 2020.
Whit Mayo -- UBS -- Analyst
Yeah, so 10% to 11% margin in the home health segment that somewhere in that range, inclusive of the synergies that you capture this year. And any way to think through either the dollar contribution from anticipated efficiencies and synergies next year?
Joshua L. Proffitt -- Chief Financial Officer
I would say Whit from a synergy perspective in any material way they are in our run rate now.
Whit Mayo -- UBS -- Analyst
Yeah.
Joshua L. Proffitt -- Chief Financial Officer
We have well north of $30 million of AFAM synergies and that's kind of in our run rate. There will always be some incremental opportunities in the AFAM business that we continue to marshall through. Part of that frankly in the third quarter was in HCBS segment,
As you see that margin lift, we've really better operationalized and if you want to say synergize that business even at the back office in the local level. So I think in a material way we've already captured it and then you will see a little bit more maybe as we move forward.
Whit Mayo -- UBS -- Analyst
Okay. And then just on-on that question, may be a second point, sorry just Florida I know it's been a little bit more disruptive of the market versus your average state that you operate in. And it that getting better at this point, is it not making any improvement? Any qualitative commentary would be helpful. Thanks.
Keith Myers
Sure, sure. So Florida is really likely to be one of the underpinning success stories as we go into 2020. If you think back to Almost Family prior to our coming together, they tended to really either call Florida out in a negative way or accept them out. We've put a lot of intense focus on that state. First and foremost from a clinical and a quality product perspective and making sure that we differentiate ourselves in that market. And just like we have with all of AFAM, Florida is really coming on strong from a quality standpoint. Then we had to frankly get better margins out of the state of Florida. Florida wasn't just a issue from a lack of growth over the years, but it really was not running anywhere near corporate margins for LHC Group. And I can very much affirm that over the course of this year, we have much more marginalized the business, and it's contributing more to the bottom line. And then lastly from a growth perspective, as I mentioned, AFAM in general is showing signs of sequential positive growth from Q3 into Q4, and Florida is one of the big contributors to that. So we are finally starting to get kind of Hershey legs under her with some growth momentum in the State of Florida. So from a quality standpoint and margin standpoint and growth, I'm looking forward to talking to you more about Florida as we head into next year.
Whit Mayo -- UBS -- Analyst
Perfect, thanks.
Operator
At this time, I'd like to turn the call back over to Keith Myers for closing remarks.
Keith Myers
Okay. Thank -- as always, thank you everyone for dialing in this morning and for all of the questions. As always between calls if you would like to speak to myself or any members of the management team, please contact Eric Elliott. We will always make ourselves available to you. Thank you so much for dialing in. And thanks for your support and confidence in LHC.
Operator
[Operator Closing Remarks].
Duration: 80 minutes
Call participants:
Eric Elliott
Keith Myers
Joshua L. Proffitt -- Chief Financial Officer
Donald D. Stelly -- President and Chief Operating Officer
Brian Tanquilut -- Vice President, Healthcare Services Equity Research
Joanna Gajuk -- Bank of America -- Analyst
Scott Fidel -- Stephens -- Analyst
Justin Bowers -- Deutsche Bank -- Analyst
Matt Larew -- William Blair & Company -- Analyst
Frank Morgan -- RBC Capital Markets -- Analyst
Whit Mayo -- UBS -- Analyst