Image source: The Motley Fool.
Teladoc Health (TDOC -2.40%)
Q4 2021 Earnings Call
Feb 22, 2022, 4:30 p.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Good afternoon, and thank you for attending today's Teladoc Health fourth-quarter '21 earnings call. My name is Sam, and I will be your moderator for today's call. [Operator instructions] At this time, I would now like to pass the conference over to our host, Patrick Feeley, head of investor relations. Patrick, please proceed.
Patrick Feeley -- Head of Investor Relations
Thank you, and good afternoon. Today, after the market closed, we issued a press release announcing our fourth quarter and full year 2021 financial results. This press release and the accompanying slide presentation are available in the Investor Relations section of the teladochealth.com website. On this call to discuss the results are Jason Gorevic, chief executive officer; and Mala Murthy, chief financial officer.
During this call, we will also provide our first quarter and full year 2022 outlook, and our prepared remarks will be followed by a question-and-answer session. Please note that we will be discussing certain non-GAAP financial measures that we believe are important in evaluating Teladoc Health's performance. Details on the relationship between these non-GAAP measures to the most comparable GAAP measures and reconciliations thereof can be found in the press release that is posted on our website. Also, please note that certain statements made during this call will be forward-looking statements as defined by the Private Securities Litigation Reform Act of 1995.
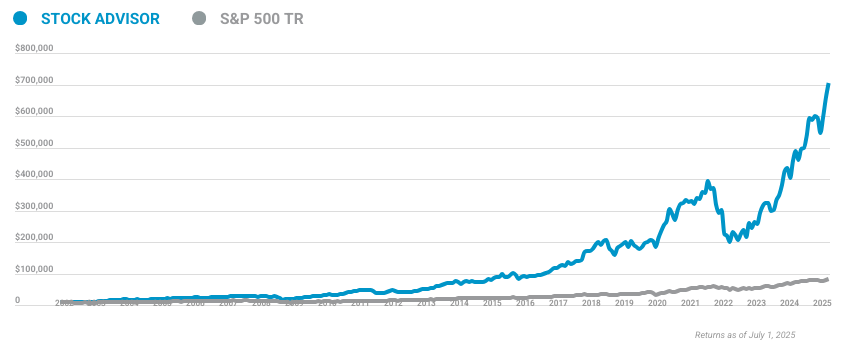
10 stocks we like better than Teladoc Health
When our award-winning analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Teladoc Health wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of January 20, 2022
Such forward-looking statements are subject to risks, uncertainties, and other factors that could cause the actual results for Teladoc Health to differ materially from those expressed or implied on this call. For additional information, please refer to our cautionary statement in our press release and our filings with the SEC, all of which are available on our website. I'd now like to turn the call over to Jason.
Jason Gorevic -- Chief Executive Officer
Thanks, Patrick. Good afternoon, everyone, and thank you for joining us. 2021 marked another record year for Teladoc Health in terms of both financial performance as well as the impact we are having on our members' lives. We launched our next-generation mental health product, myStrength Complete, combining the best of Livongo and Teladoc capabilities, and announced significant new deals for our virtual primary care product, Primary360.
In the direct-to-consumer market, our BetterHelp product posted another year of record growth, exceeding $700 million in global revenue. We exited 2021 with significant sales momentum with fourth-quarter bookings showing strong growth both sequentially and over the prior year. Notably, multiproduct sales represented 80% of full-year bookings. For the fourth quarter, Teladoc Health posted another strong quarter of financial performance, as we continue to deepen member relationships and increase the care delivered to consumers.
The broad-based strength across the business drove revenue of $554 million in the fourth quarter, representing an increase of 45% over the prior year, including organic growth of 32%. Our vision is to become the first stop in the consumer healthcare journey regardless of need by delivering whole-person care to meet the complex needs of our members from physical to mental, acute to episodic, and chronic to complex. To advance this vision, we continue to focus on our key strategic priorities that we believe underpin the next phase of significant growth for our company. Those priorities include expanding adoption of our integrated virtual primary care product, Primary360; expanding our mental health services to meet growing demand; and enhancing our chronic care capabilities in order to be even more impactful for clients and members.
Importantly, we will continue to build upon the integrated Teladoc experience that unifies all our products and services, making it easier for patients, care providers, and clients to realize the full value of our whole-person approach. Primary360, our virtual primary care product, enables Teladoc to become the front door to the healthcare system for our members. We believe our unmatched depth and breadth of capabilities positions the company as the global leader in whole-person virtual care. While it remains early, I am very pleased with the enrollment and engagement we're seeing in Primary360 so far.
I was just reviewing data from one of our partners that recently launched a Virtual First plan supported by our Primary360 product. And the number of people choosing the plan has significantly exceeded our initial forecasts. And 75% of the members who have enrolled in that plan are entirely new to that insurer. So Primary360 is clearly proving to be a differentiating factor in the marketplace for our health plan clients.
Virtual First plan offerings are increasingly being viewed as strategic necessities among insurers and is the leader in the space with the most robust and comprehensive offering. We're well-positioned to partner with those plans. We now have over 50 clients live on Primary360, including several Fortune 500 employers and our pipeline of opportunities continues to build. Our Primary360 offering is resonating in the employer market due not only to the breadth and depth of our product but because of our ability to scale and integrate with an employer's benefit design.
Large employers need a virtual primary care offering that can both serve an employee base spread across geographies and integrate with multiple insurance plans since large employers typically offer plans from more than one insurance carrier. We're uniquely positioned to be that partner given our track record of working across multiple national and regional payers. We expect to launch Primary360 with several new clients over the course of the year across channels, including a newly signed partnership to launch a Virtual First health plan with a large provider-sponsored organization in the Midwest. This integrated health system deal is notable as we beat out an incumbent telemedicine provider in the process, demonstrating the power of our industry-leading suite of services.
It also demonstrates progress against our strategy to bring our entire suite of products across all of our channels, including health systems. In chronic care, the number of individuals enrolled in our suite of solutions grew 22% year over year to 729,000 at the end of the fourth quarter. Over 40% of adults in the U.S. are living with multiple chronic conditions.
And as you've heard me say in the past, individuals don't view themselves as just a person with a chronic disease. They view themselves as a person who needs help accessing care and managing their entire health. Importantly, our approach of focusing on the whole person as opposed to a single condition continues to pay off. The percentage of chronic care members enrolled in more than one program has doubled over the prior year, resulting in total chronic care program enrollment growth of over 30%.
Last week, we announced the launch of our new Chronic Care Complete product line, which incorporates data-driven outreach to connect enrollees in our chronic care programs with Teladoc physicians. This will, for example, enable us to leverage the Teladoc physician network based on real-time data to better engage with chronic care members who may be struggling to control their disease and provide services such as adjusting care plans or optimizing medications. Chronic Care Complete will allow us to leverage our data capabilities, including the billions of data points we've collected to date to make intelligent interventions, drive better outcomes for our members, and lower cost for our clients. This integration of our telemedicine capabilities, our digital chronic care management programs, and our robust data capabilities represents the latest example of our integrated stepped care approach and follows on the heels of the launch of our myStrength Complete mental health offering last year.
Mental health remains another key priority for us and an area where we continue to see tremendous demand for care. In the direct-to-consumer channel, our BetterHelp brand continues to drive significant growth, both in the U.S. and international markets. In the B2B channel, our new flagship myStrength Complete product, which offers both digital capabilities and virtual interactions is gaining momentum.
We find that since mental health is a longitudinal relationship where members typically have several visits with their therapist or psychiatrists, it acts like a gateway for other Teladoc services. And we also find that our members who utilize mental health, combined with another Teladoc service, such as general medical or dermatology, generate revenue that's 20% to 60% higher on average than those who utilize mental health services alone. So not only does multiservice usage enable better access to care and drive cost savings for our clients, but it also enables us to efficiently drive higher engagement and revenue growth. Before I turn the call over to Mala to discuss our results and financial guidance in more detail, I want to talk briefly about our outlook for 2022.
For the full year, we expect revenue to be in the range of $2.55 billion to $2.65 billion, representing growth of 25% to 30%. Our expectations for strong growth are a result of the broad-based momentum we continue to see across our suite of products and services and across geographies. We have over 90 million total individuals with access to the Teladoc platform today, and we see a significant opportunity for long-term growth by expanding our relationships and going deeper with our existing clients and members as we execute against our key strategic priorities across primary care, mental health and chronic care solutions. With that, I'll turn the call over to Mala for a review of fourth quarter as well as detailed '22 guidance.
Mala Murthy -- Chief Financial Officer
Thank you, Jason, and good afternoon, everyone. During the fourth quarter, total revenue increased 45% year over year to $554 million, including 32% organic growth. Access fee revenue for the fourth quarter increased 51% year over year to $470 million and represented 85% of total revenue, up from 81% in the prior year's quarter. We ended the quarter with U.S.
paid membership of 53.6 million members, above the high end of our guidance range and an increase of 1.1 million members over the third quarter. Individuals with visit fee only access was 24.2 million at the end of the fourth quarter, representing an increase of 600,000 individuals. Total unique members enrolled in one or more of our chronic care programs was 729,000 members as of the fourth quarter, an increase of 133,000 enrollees over the prior year's quarter and in line with our expectations. Average revenue per member per month was $2.49 in the fourth quarter, up 52% from $1.63 in the prior year's quarter and up 4% sequentially from $2.40 in the third quarter of 2021.
Please note that as of the fourth quarter, BetterHelp revenue from international markets is now included in the international revenue line item and is therefore excluded from our reported U.S. revenue per member per month. Please see the schedule at the end of the earnings press release for prior period numbers recast for this change. Visit fee revenue for the fourth quarter of $69 million increased 21% year over year.
During the fourth quarter, we provided 4.4 million visits through our network of clinicians. The visit count in the fourth quarter includes the benefit of approximately 187,000 visits in the international markets that were previously excluded from the visit count. Excluding these visits, our total visits in the fourth quarter would have been just over 4.2 million, above the high end of our prior guidance range. Also, please note that the BetterHelp visits from individuals located outside the U.S.
have moved from the U.S. visit count to the international visit count. And this shift impacts our reported utilization rate, which is a U.S.-specific metric. Please see the schedule at the end of the press release for prior period numbers recast for this change.
Fully adjusted, total visits grew 41% over the prior year's quarter. The annualized utilization rate for our members was 22.7% in the fourth quarter, a 670-basis-point increase over the prior year's quarter and a 170-basis-point increase sequentially. Contributing to the strong growth was persistent strength in mental health utilization as visits more than doubled in each of the direct-to-consumer and B2B channels in 2021. After a period of low overall transmission of infectious disease due to social distancing and PPE usage, we have also begun to see infectious disease volumes rebound in the second half of 2021, growing more than 35% in the second half of the year as compared to the first half of the year and contributing to strong fourth-quarter total visit growth.
Adjusted EBITDA was $77.1 million in the fourth quarter, compared to $50.4 million in the prior year's quarter. Net loss per share in the fourth quarter was $0.07, compared to a net loss per share of $3.07 in the year-ago period. Net loss per share in the fourth quarter included stock-based compensation expense of $0.39 per share, amortization of acquired intangibles of $0.28 per share and a noncash income tax benefit of $0.31 per share. The company generated strong operating cash flow in the quarter of $83 million, and operating cash flow for the full year was $194 million.
We ended the year with $893 million in cash on the balance sheet. Now turning to forward guidance. For the full year 2022, we expect revenue to be in the range of $2.55 billion to $2.65 billion, representing growth of 25% to 30% over the prior year. We expect total membership of 54 million to 56 million members, representing growth of 1% to 5% year over year, with the remainder of revenue growth driven by expanding revenue per member driven both by increased product penetration and product mix.
We expect adjusted EBITDA in 2022 to be in the range of $330 million to $355 million, representing a 12.9% to 13.4% adjusted EBITDA margin and an expansion of approximately 90 to 140 basis points over 2021 after normalizing for last year's purchase price accounting benefit. We expect total visits in 2022 to be between 18.5 million and 20 million visits, representing growth of 20% to 30% over the prior year. For the first quarter of 2022, we expect revenue of $565 million to $571 million, representing growth of 25% to 26% over the prior year's quarter. We expect total paid membership in the range of 54 million to 54.5 million in the first quarter.
Total first-quarter visits are expected to be between 4.3 million and 4.5 million visits representing year-over-year growth of 29% to 35% driven in part by a surge in COVID-related visits seen during January. We expect first-quarter adjusted EBITDA to be in the range of $51 million to $55 million. Included in first-quarter adjusted EBITDA is an expected $4 million drag from incentive payments made to our network of physicians during the recent omicron spike. Provider payments have largely normalized by the start of February, and we do not expect the increased level of incentive payments to recur.
I would like to talk briefly about the expected cadence of revenue and adjusted EBITDA growth over the course of this year. On the revenue side, we expect the timing of new chronic care client onboardings to be more heavily weighted toward the second half of this year. This includes the launch of large new health plan clients signed over the past several months, including HCSC and another regional Blue plan, which are scheduled to onboard in the second half of this year. We, therefore, expect to see strong sequential growth in revenue over the course of the year.
Specific to the second quarter, we expect an approximate $40 million to $50 million step-up in revenue from 1Q to 2Q. On the expense side, we normally see higher engagement marketing spend in the first half of the year as we prepare to onboard new clients and members. It's also typical for us to see higher advertising spend early in the year as we take advantage of lower media pricing in the market following the conclusion of the more expensive holiday season. We expect that to be the case again this year, as we have seen a more advantageous media buying landscape early this year, which has resulted in a slightly lower customer acquisition cost.
This will impact the quarterly cadence of adjusted EBITDA, and we expect will result in a significant margin expansion progression over the course of 2022, particularly in the second half due to our expected revenue and enrollment ramp for the chronic care programs launching later this year as well as the typical seasonality of advertising spend over the course of the year. It's important to note that the revenue and EBITDA ramp described is not dependent on significant new sales. The deals mentioned are contracts that have been signed over the past several months but are disproportionately scheduled to onboard in the second half. And we, therefore, have good visibility into the second half revenue and EBITDA progression.
With that, I will turn the call back to Jason for closing remarks.
Jason Gorevic -- Chief Executive Officer
Thanks, Mala. We remain confident in the long-term revenue and profitability outlook that we provided at our Investor Day in November. Specifically, our confidence in delivering substantial growth in '22 comes from our proven ability to have impact by improving people's lives. This morning, Teladoc Health published our second annual Corporate Social Responsibility Report, which highlights how we, as a company, seek to have an impact beyond our business and live our values in the communities we serve.
The report highlights our commitment to taking care of people, building trust, operating responsibly, and having a positive impact globally. And I'm pleased that it shows tremendous progress in 2021, including a new employee volunteerism program that delivered more than 12,000 hours of support for employee-chosen charities and making meaningful progress in hiring a more diverse workforce. I encourage you to check it out on our website and learn more about how Teladoc Health is giving back to our communities and building a sustainable enterprise. As always, thank you for your continued interest in Teladoc Health.
And with that, we'll open the call for questions. Operator?
Questions & Answers:
Operator
[Operator instructions] Our first question is from the line of Ryan Daniels with William Blair. Ryan, your line is connected. Please proceed.
Ryan Daniels -- William Blair -- Analyst
Yes. Thanks for taking the questions. I guess, can you speak a little bit more to the revenue cadence and kind of the visibility you have there? With the new plan starting up, are they kind of guaranteed, if you will, to start in the second half of the year? And do you have pretty good visibility on the number of members in PMPM, etc., to ensure that that ramp occurs? Thanks.
Mala Murthy -- Chief Financial Officer
Thanks, Ryan, for your question. Yes. So let me give you a little bit of color on how we see the revenue ramp sort of progressing through the year. So first is if you think about the guidance range that we just gave of 25% to 30% growth, that is consistent with the overall outlook that we provided back in November at Investor Day.
As we said in our prepared remarks, Ryan, we do expect to see a meaningful ramp in revenue over the course of the year. We talked about the ramp that we are seeing in the second quarter, the $40 million to $50 million. And then we see a further ramp from there into the second half. So it's definitely more back half weighted as our -- as we look at the revenue progression, and we've talked about the key drivers of it, right? One is that we have multiple health plan clients that will onboard in the second half.
As we talked about the ramp that we're seeing isn't dependent so much on new sales. These are deals that we have already contracted. So we have really good visibility into the sales and the revenue, it is just really a question of timing. The onboarding is going to happen in the beginning of the second half and as we start that and as you see the normal enrollments of curve and the ramp hit its stride, you will see the revenue come through more in the back half than in the first half.
So that's sort of how we are thinking about our overall revenue cadence for the year.
Operator
Thank you, Ryan. Our next question is from Lisa Gill of J.P. Morgan. Lisa, your line is connected.
Please proceed.
Lisa Gill -- J.P. Morgan -- Analyst
Thanks very much. Good afternoon. Jason, thanks for the comments on BetterHelp, $700 million you talked about for BetterHelp this year. Can you maybe just help me to understand just a couple of things.
One, when we think about BetterHelp, Mala made the comment of slightly lower acquisition costs, is that particular to BetterHelp? Are you talking about in general? Two, when we think about clinician costs, again, you talked about $4 million of incremental incentive payments, but we hear a lot about the ability to attract and retain clinicians in the marketplace right now because we are in a mental health crisis here in the U.S. So can you talk about those things? And then thirdly, when we think about BetterHelp in 2022, how do we think about how that business is growing. And you talked about those that use mental health use other services, but how do we think about retaining that member when we think about behavioral health services?
Jason Gorevic -- Chief Executive Officer
Lisa, thanks for the questions. I think those were three, but we'll cram them into one question. With respect to the customer acquisition costs and Mala's commentary, what she was talking about is the overall media landscape, in particular about BetterHelp. Our customer acquisition costs are down slightly as we look at this year versus the same period last year.
In addition, we're seeing benefit of BetterHelp's brand awareness and really market-leading brand, which enables us to see an increase in the number of members who are signing up organically without any acquisition costs. So the combination of those two things have been very favorable and gives us a strong outlook for the BetterHelp product specifically, but also across all of our mental health offerings. With respect to the clinician costs and the $4 million of incremental spend on top of our expectations in January, that was entirely on the physician side and due to the spike in the Omicron variant and higher-than-expected visit volume for our general medical services. So that actually didn't impact mental health at all.
We feel very good about the attraction of new therapists onto our platform. I was just talking to the team, we onboarded over 10,000 therapists last year. And just in January, we were over 1,200 new therapists on the platform. So I feel very good about access to additional talent and capacity as we continue to expand that.
And that -- the combination of those two things, both the continued more effective customer acquisition spend as well as the access to capacity on the supply side, gives me a strong outlook because we are also seeing the benefit of product enhancements to the BetterHelp product, where we roll out things like virtual group sessions that enable us to take advantage of a one-to-many relationship and also, at the same time, increase the lifetime value and retention of our client base. So all of those things together make me very bullish on the outlook for 2022.
Operator
Thank you, Lisa. Our next question is from the line of Jailendra Singh of Credit Suisse. Jailendra, please proceed.
Jailendra Singh -- Credit Suisse -- Analyst
Thank you, and thanks for taking my question. First, a quick clarification. Some of these health plans, including HCSC, you're talking about onboarding in the second half. Were they always planned for second half? Or there were any delays for some reasons? Just trying to make sure that -- are you still maintaining your 25% to 35% growth in chronic care business in 2022? And is it possible for you to give some specific color around chronic enrollment expectations and cadence there? I think historically, you've talked about 70% to 80% additions coming in first half and looks like things will be different this year.
Mala Murthy -- Chief Financial Officer
Yes. So Jailendra, I'll give you -- answer those questions in order. In terms of the onboarding, I would say, in general, that is true. We do have one significant client that had originally planned to launch Jan 1, but candidly, due to their own internal data delays, we are now going to be launching with that client in the beginning of the second half.
But I would say more broadly for the rest, it is -- the expectation was going to be launching in the start of the second half. In terms of the chronic care question that you asked, we have shared in the past that we won't give you very specific sort of outlooks along each of the different tracks that we had talked about on Investor Day every quarter. We plan to do some kind of updates on occasion once a year. But I would say just generally, we had talked about the revenue growth for chronic care back in Investor Day.
We are seeing all of the right trends as we think about chronic care revenue growth. And if I think about exiting the -- a run rate exit for 2022, I am comfortable with the growth rates that expectations that we had set back in November.
Operator
Thank you, Jailendra. Our next question is from Richard Close of Canaccord Genuity. Richard, please proceed.
Richard Close -- Canaccord Genuity -- Analyst
Great. Thanks for the question. Given the change in classification in the BetterHelp international visits and the impact -- I guess, the adjustment on utilization, what would be a good target to think about in terms of utilization rates increasing year over year? I think you provided some internal targets before.
Mala Murthy -- Chief Financial Officer
So if you look at the guidance that we have talked about in terms of how we see our revenue -- our visit volume growth for the full year, right, we gave you guidance for full year, you look at the strength of visit volume momentum in 4Q and for the full year. What, Richard, that gives you is sort of the key elements and ingredients of how -- we've essentially given you all the ingredients and elements on how to think about utilization for full year 2022 as compared to 2021. So I feel very comfortable with the progress we are making in terms of the strong visit volume growth. And just some further color, just to sort of segue from the comments that Jason made on mental health overall.
We have talked about the strength that we are seeing in specialty visit volume, right? Specialty visit volume in 4Q grew 50% year on year. We've also seen -- as we talked about in our prepared remarks, we are beginning to see growth again in infectious disease volumes, right? Like that was something that was more muted through COVID with social distancing and PPE, etc. So these are the inputs that go into the momentum that we are seeing in our visit volume overall for '22, and you can see that in the guidance that we put out there.
Operator
Thank you for that question. Our next question is from Sean Dodge of RBC Capital Markets. Sean, your line is connected. Please proceed.
Sean Dodge -- RBC Capital Markets --- Analyst
Thanks. Good afternoon. Maybe going back to chronic care. On the launching of the new Chronic Care Complete program, Jason, can you give us just a quick rundown of how that is going to be commercialized? Does that get automatically offered or built into existing chronic condition customers? Or is this something that's going to have to be sold, I guess, maybe more from scratch.
And then the revenue model with the sharing elements of Livongo and legacy Teladoc, is this something that prices like a fixed monthly charge per enrollee? Or is there going to be a variable usage component to it as well?
Jason Gorevic -- Chief Executive Officer
Yes. Thanks, Sean. We're in the market now with our Chronic Care Complete product line. When you think about the full package, it bundles our diabetes, hypertension, and pre-diabetes programs into a comprehensive package for clients which includes physician-based care.
The nice thing about that, and I think the unique thing is it not only addresses multiple chronic conditions, but also targets individuals who have -- are having a hard time controlling their A1c or blood pressure, and it helps them to get back on track by optimizing their medications. So only a targeted subset of the members will be engaging with the physician component of that. When we look at it, it's I think the next step in us rolling out our stepped care approach. And of course, myStrength Complete was the prototype for that.
The Chronic Care Complete offering will also have individual sort of single condition offerings into the market. So if you think about diabetes complete or hypertension complete, those will be available with the physician component and we believe that the Chronic Care Complete that's multi-condition will be the most popular option. It ends up being a fixed per participant per month fee that is sort of a composite, if you will, of the various components where diabetes is a little bit on the higher side than the composite price, hypertension is a little bit on the lower side and pre-diabetes is sort of right in line but it ends up being a very healthy revenue stream and really incent buyers to adopt a multi-condition approach. So I feel very optimistic that, that will be our lead chronic care program in the portfolio as we go through the 2022 selling season.
Operator
Thank you, Sean. Our next question is from Charles Rhyee of Cowen. Charles, your line is connected. Please go ahead.
Charles Rhyee -- Cowen and Company -- Analyst
Yes. Thanks for taking the questions. Maybe, Mala, I wanted to talk about the first-quarter EBITDA guidance. And just trying to understand, as we think about maybe costs related to starting up Primary360 and Chronic Care Complete, etc.
What percent of those costs would you say are sort of nonrecurring in the sense that now that once you get those programs off the ground, they would not necessarily recur going forward? And just to clarify, I think maybe from Jailendra's question earlier, this chronic care management membership, like what percent of the chronic care membership, that 25% to 35%, is going to be coming from the second half?
Mala Murthy -- Chief Financial Officer
Yes. So -- the way I would think about the profit progression, the adjusted EBITDA progression, and how you should think about the investments really is what you're asking, Charles. So the way it is going to unfold as we go through the year is as follows. First of all, as I said, you will see expansion in adjusted EBITDA margins as we go through the year.
Why is that? Because it is sort of following the revenue ramping that we are seeing in the second half of the year, especially as you think about chronic care ramping through the second half of the year. If you think about the operating expense lines into which the investments are folded, I would say we expect to see A&M spend sort of -- as we've talked about in the prepared remarks, we are -- there is seasonality in it. And we are spending in the first half of the year as we take advantage of the low media costs and the buying opportunities it provides us, I would say, overall, for the year, I do expect A&M to be slightly higher as a percentage of revenue on a full-year basis as we drive the strong growth that we have on the mental health side. I do expect us to get leverage as we go through the year on the rest of operating expense, including G&A and selling.
And I would say on technology and development, so on the R&D investments that we are making, I think you will see that sort of -- expected to say almost steady, if you will, in terms of percentage of revenue. So they're all slightly different in terms of how we are seeing it ramp through the year. But overall, I would say all of that is what is getting us to the profit margin expansion as we go through the year.
Operator
Thank you, Charles. Our next question is from Jessica Tassan of Piper Sandler. Jessica, please proceed.
Jessica Tassan -- Piper Sandler -- Analyst
Hi. Thank you so much for taking the question. So I think we were really impressed to hear that BetterHelp customer acquisition cost is down. Can you maybe help us understand how some of the consumer privacy initiatives from Apple and Google, specifically Apple's app tracking transparency policy might be impacting your DTC advertising cost and productivity? And kind of what are you guys doing to mitigate the impact of those policies.
Jason Gorevic -- Chief Executive Officer
Yes. Jess, thanks for the question. We've actually taken those all into account as we've built our models. Our team is very closely monitoring all of the developments there.
I would say that we are ahead of the curve with respect to understanding what's going on there and modeling anything that would or potentially have any impact on our strategies. But with the current situation and our insight there, we don't see any significant impact on our outlook.
Operator
Thank you, Jess. Our next question is from Daniel Grosslight of Citi. Daniel, please proceed.
Daniel Grosslight -- Citi -- Analyst
Yes. Thanks for taking the question. I want to stick with BetterHelp here. Some of your competitors have had difficulties with churn and retention.
Are you seeing any degradation in LTVs for 2022 in the DTC channel? And then in the B2B channel, I think it's a little less apparent, but BetterHelp is actually growing quite nicely in the EAP channel. I notice Citi is now offering BetterHelp through our EAP. Can you talk about growth of BetterHelp in the enterprise channel apart from the DTC channel?
Jason Gorevic -- Chief Executive Officer
Sure. We're actually seeing improvement in our LTV. I'm aware of some of the other players in the market. I would say our team has a tremendous track record of continuing to improve LTV.
That's a combination of optimizing pricing and driving product enhancements that increase the longevity of those members. I feel like sometimes having others out there who aren't performing at the same level, casts a negative shadow. And to be honest, we just outperformed in that market and in that regard. With respect to BetterHelp in the B2B channel, we are finding a fertile environment among EAP plans, the model there is sort of a B2B2C customer acquisition strategy, where BetterHelp gets embedded in an EAP plan and a certain set of interactions are included in the EAP expense.
And then after that, there's a warm transition into a direct paying consumer as the consumer exhausts the EAP benefit. We're finding that as an efficient not only customer acquisition strategy, but one that provides more value than the typical EAP plan of the past and is therefore valuable both to the consumer and to the sponsoring employer.
Operator
Thank you, Daniel. Our next question is from George Hill of Deutsche Bank. George, please go ahead.
George Hill -- Deutsche Bank -- Analyst
Yes. Good morning. I'm going to come back to BetterHelp one more time. And I guess, Mala, I'd ask -- you used the word persistency in your prepared comments.
I guess, could you provide a little bit more color as it relates to the behavioral product of how much of it is growth of new members and kind of how much of it is growth of revenue per member? And kind of what is the right way to think about that as we think about the contribution of the growth of the behavioral product over time?
Mala Murthy -- Chief Financial Officer
Yes. So, George, I would say it's all of those. So if you think about the -- let me address it from both the DTC side as well as the B2B side. On the direct-to-consumer side, as we think about the momentum that we are seeing in BetterHelp, we are absolutely seeing all of the, what I would call, the operating metrics make a tremendous amount of healthy progress, whether it be the number of members, whether it be better -- lower churn and greater retention that is feeding the increasing LTV.
Jason just talked about what is fueling that in terms of product innovation, etc. And whether it be customer acquisition costs, right? And again, we have talked about why are our customer acquisition costs being managed as tightly and efficiently as it is. It is about continuously innovating with new media channels. It's things like that that is getting us to really strong execution on the operating metrics.
So I would say on the direct-to-consumer side, George, to answer your question, it is both more membership. It is greater LTV. And all of that is what feeds our growing revenue per member, if you will. The other thing to not underestimate is the fact that if you think about just BetterHelp as a direct-to-consumer business, the ability for us to price through in terms of the innovation that we are seeing, etc., is much more dynamic.
And we use data -- our data science capabilities, etc., in a very, very dynamic way, such that we can manage our overall margins and profitability for that business. I would say, very similar dynamic that we are seeing on the B2B side, right? Whether it be starting with the tremendous visit volume momentum that we are seeing in mental health -- in sort of our legacy mental health business. And the progress that we are making as I look at the pipeline for our myStrength Complete product that, as you know, we launched in the middle of last year, once again, we are seeing tremendous traction in the demand for our B2B mental health product. Unsurprisingly, just given the total addressable market that is out there and the fact that we are absolutely the leader in mental health, the scale that we have in mental health is something that is helpful for us in attracting providers in getting to the economics and the execution that we are demonstrating in our numbers.
So it's all of the above.
Operator
Thank you for that question. Our next question is from Stephanie Davis of SVB. Stephanie, please proceed.
Stephanie Davis -- SVB Leerink -- Analyst
Hey, guys. Thank you for taking my question. I'm going to go a little bit away from the BetterHelp side of the world and actually ask more about Primary360. As this product scales up a bit more, I'd be curious in your thoughts on care navigation, how that ties in or if there is some investments to internal care navigation as you kind of build it out.
Jason Gorevic -- Chief Executive Officer
Yes. Stephanie, thanks for the question. We're really excited by the progress we're making with Primary360. The market adoption has been very strong.
Consumer experience data is off the charts with 95% member satisfaction. And what we're finding is the clinical impact that we make is very significant, identifying large populations of first diagnosis for chronic conditions, either adding or altering prescriptions, and to your question about helping consumers find the right care when they need to be seen in-person. When people talk about care navigation, they mean a lot of different things. And so I want to tell -- explain what we mean by that.
We mean helping the consumer get the care they need in the course of their overall healthcare. That does not mean administrative navigation to us. What it does mean is using the data that we have about the consumer, the actual delivery of care and deep interaction we have with the consumer to make sure that they get to the right site of care the first time. Given the combination of our digital interactions with them using devices and their interactions with our platform, the care delivery interactions we have driven out of our virtual visits, both on the mental and physical side and given our unique capabilities when it comes to expert medical opinions from our depth of experience there, we feel like we are uniquely positioned because we deeply integrate with the health plan to be able to make the most efficient referral for them when they need to be seen in-person and then act as almost a concierge on their behalf.
So when we talk about care navigation, that's what we mean because we think that's the highest value form of care navigation.
Operator
Thank you, Stephanie. Our next question is from Ryan MacDonald of Needham. Ryan, please proceed.
Ryan MacDonald -- Needham and Company -- Analyst
Thanks for taking my question. On Primary360, I wanted to touch on the insurer channel. And you talked about the relevance that you're seeing for the offering within Virtual First plan. Just curious if you think that this is -- the growth of that product is dependent on the proliferation and addition of additional Virtual First plan? Or do you think that you can actually start to weave this into traditional plans as well?
Jason Gorevic -- Chief Executive Officer
Yes. I think the answer is both. Virtual First plan designs can be an accelerator because, of course, they provide financial incentives to the consumer to engage in a virtual primary care relationship. But I don't think that the success of Primary360 is dependent on the proliferation of Virtual First plan designs.
What we see with the clinical impact that we're having as well as the member experience that we're having is one where I believe, over time, it will be a sought-after relationship and a sought-after product that driven as much by the consumer as by the plan design because of the opportunity to have more frequent interactions, to have access to a full care team, to have access to digital interactions and to get the power of the underlying data science to help drive a more personalized and better healthcare outcome.
Operator
Thank you, Ryan. Our next question is from Stan Berenshteyn of Wells Fargo. Stan, please proceed.
Stan Berenshteyn -- Wells Fargo Securities -- Analyst
Hi. Thanks for taking my questions. Jason, maybe on chronic care, can you give us an update on where you stand in regards to chronic care products that are outside of the diabetic/hypertension verticals?
Jason Gorevic -- Chief Executive Officer
Yes. So as you know, we launched a CKD product for chronic kidney disease. You could make the argument that that's on the same continuum, but it's a different manifestation, and obviously, a more severely ill and higher-cost population as well. You've heard us talk about continuing on the cardiometabolic continuum and branching out into other areas.
I'm not going to sort of preannounce where we're going to go in our next set of chronic conditions. But what I can say is that our team is actively working on several expansion opportunities as we consistently look to expand the scope of our clinical offerings to be able to take care of the entirety of an individual and access additional populations.
Operator
Thank you, Stand. Our next question comes from Steven Valiquette of Barclays. Steven, please proceed.
Steven Valiquette -- Barclays Capital -- Analyst
Thanks. Good afternoon, everybody. So all the color on the quarterly progression of the revenues and EBITDA was helpful. But with the 1Q '22 EBITDA margin guide in the 9% to 9.5% range and then just thinking about what you said about the revenue ramp happening in the back half of the year, just kind of playing around the model, it seems like the EBITDA margin would have to be somewhere in the high teens for the fourth quarter, maybe 17% or so, which is really the margin that I think consensus wouldn't really reflect the company hitting on a full-year basis for another three, four years or so from the 13% jump-off point from last year.
I guess I just want to make sure that we're not missing anything in relation to what seems like that margin -- EBITDA margin again in the kind of high teens for the fourth quarter as we kind of just sort of build out all -- everything that you talked about.
Mala Murthy -- Chief Financial Officer
Yes. So as you think about -- as we think about the ramp, you are right. What I would say is you are in the right ballpark. We have talked about the seasonality of revenue ramping in the second half, especially on the chronic care side.
You know the margins that come with chronic care revenue. So it's not surprising that we are -- the ramp of profit and the expansion of margin is going to be back half weighted. So yes, you are in the right ballpark, absolutely, on seasonality.
Operator
Thank you, Steven. Our next question comes from the line of David Larsen of BTIG. David, please proceed with your question.
David Larsen -- BTIG -- Analyst
Hi. Can you talk about the impact, if any, that -- and to the public health emergency might have on the overall business. I think it's scheduled to go through mid-April, like April 16. So if we actually get through that and it's not extended again, what impact could that have on the business? Like, for example, like reimbursement for telehealth visits at parity with in-person visits, how could that change, if at all, and then also plan designs with like co-pays and deductibles being waived for COVID patients? Just any thoughts there, along with expected trends from COVID in '22 would be helpful.
Jason Gorevic -- Chief Executive Officer
Yes. I don't think it will have any real impact on our outlook. Most of the plan designs that had waived co-pays on virtual visits have reverted back to charging co-pays for those visits. Most of the states who had waived licensure requirements have reverted back to requiring in-state licensure.
Almost none of our business is Medicare fee-for-service. And therefore, we're really not sensitive to Medicare reimbursement. We don't get reimbursed at parity when we provide visits for our populations, we get reimbursed for our agreed-upon fees which are not at parity with an in-person visit and part of the attraction of them, quite frankly. So I actually don't see any real impact.
The other part where I think we're beyond any questions about sort of the national health emergency is reimbursement for chronic care management, the impact of value-based care and value-based reimbursement aligns us with both the payer as well as the provider when they're taking risk. So I see really only tailwinds going forward. And as you probably know, there are several movements within Congress to continue to expand the support for both from a regulatory as well as reimbursement perspective the continued expansion of virtual care.
Operator
Thank you, David. Our next question is from Dev Weerasuriya of Berenberg. Dev, please proceed.
Dev Weerasuriya -- Berenberg Capital Markets -- Analyst
Hey. Good evening. Thanks for taking my questions. Want to circle back to the operating margins and just margins in general in relation to kind of the customer acquisition costs and related sales and marketing spend required to keep patients engaged.
And I'm just trying to get some color around how these differ -- we got a lot of color around BetterHelp, but maybe for P360 as well as chronic care, kind of how the cadence moves from, let's say, the quarter that you onboard the client toward kind of Q4 or the subsequent quarters? And then kind of the second question in relation to that is, so we see this sequential ramp-up in margin, some leverage on, I would assume, on the sales and marketing side and as well as other operating leverage through the year. How would that -- or what kind of changes are there from a year-to-year basis instead of within a year as well?
Mala Murthy -- Chief Financial Officer
OK. So I'll address them in turn, Dev. If you think about the sales and marketing, as you talked about for Primary360 and chronic care, again, what I would say is that is where we look to the ramping of our B2B engagement marketing spend. And we have thought about the ramping of that as we -- ahead of the launches, so that, again, we are looking at pacing the timing of our A&M spend for visit volumes as we go through the year.
This is on the legacy telehealth side. But as we really scale -- as the populations launch for chronic care, think of the spend -- the marketing spend on that roughly sort of consistent and pacing that, right? So we need the program to launch. We need the clients to launch, and then we will do the work we do on engaging with those so that we get the appropriate enrollment sort of ramping up once those clients launch on the chronic care side. And I'd say similarly on Primary360.
So think of the client launches and the spend on the B2B marketing side as sort of consistent with that -- the marketing spend that we do on our other telehealth -- normal telehealth visit volumes, whether it be infectious diseases or specialty, think of that consistent with prior years. I think we have plenty of history, demonstrated history on the spend we do on that and the success we have on driving the momentum on that. On your second question in terms of year over year, as I said a few minutes ago, there's no question. We are investing in our A&M spend as we -- especially on the direct-to-consumer side, and so we do expect to see growth in A&M spend.
I sort of talked about the relation of that with our revenue. And I want to be clear, that is with the fact that we are seeing sort of the customer acquisition costs continue to be very efficient. So we continue to see the efficiencies in our marketing spend on that. We do expect to see G&A leverage.
We have done that in prior years, and I would expect to continue to get operating leverage on the G&A line as our revenue ramps. And as I said a few minutes ago, we will invest, as we have shared on Investor Day, on our technology road map, on our product innovation road map and therefore, in R&D. So there are sort of -- hopefully, that gives you more color on the different line items within operating expense in '22 and how that compares to prior year.
Operator
[Operator signoff]
Duration: 63 minutes
Call participants:
Patrick Feeley -- Head of Investor Relations
Jason Gorevic -- Chief Executive Officer
Mala Murthy -- Chief Financial Officer
Ryan Daniels -- William Blair -- Analyst
Lisa Gill -- J.P. Morgan -- Analyst
Jailendra Singh -- Credit Suisse -- Analyst
Richard Close -- Canaccord Genuity -- Analyst
Sean Dodge -- RBC Capital Markets --- Analyst
Charles Rhyee -- Cowen and Company -- Analyst
Jessica Tassan -- Piper Sandler -- Analyst
Daniel Grosslight -- Citi -- Analyst
George Hill -- Deutsche Bank -- Analyst
Stephanie Davis -- SVB Leerink -- Analyst
Ryan MacDonald -- Needham and Company -- Analyst
Stan Berenshteyn -- Wells Fargo Securities -- Analyst
Steven Valiquette -- Barclays Capital -- Analyst
David Larsen -- BTIG -- Analyst
Dev Weerasuriya -- Berenberg Capital Markets -- Analyst