Image source: The Motley Fool.
Teladoc Health (TDOC 2.46%)
Q4 2022 Earnings Call
Feb 22, 2023, 4:30 p.m. ET
Contents:
- Prepared Remarks
- Questions and Answers
- Call Participants
Prepared Remarks:
Operator
Good afternoon, and thank you for attending today's Teladoc fourth quarter 2022 earnings conference call. My name is Daniel, and I will be the moderator for today's call. [Operator instructions] It is now my pleasure to pass the conference over to our host, Patrick Feeley, head of investor relations. Patrick, the floor is yours.
Patrick Feeley -- Vice President, Investor Relations
Thank you, and good afternoon. Today, after the market closed, we issued a press release announcing our fourth quarter and full year 2022 financial results. This press release and the accompanying slide presentation are available on the Investor Relations section of the teladochealth.com website. On this call to discuss the results are Jason Gorevic, chief executive officer; and Mala Murthy, chief financial officer.
During this call, we will also provide our first quarter and full year 2023 outlook, and our prepared remarks will be followed by a question-and-answer session. Please note that we'll be discussing certain non-GAAP financial measures that we believe are important in evaluating Teladoc Health's performance. Details on the relationship between these non-GAAP measures to the most comparable GAAP measures and reconciliations thereof can be found in the press release that is posted on our website. Also, please note that certain statements made during this call will be forward-looking statements as defined by the Private Securities Litigation Reform Act of 1995.
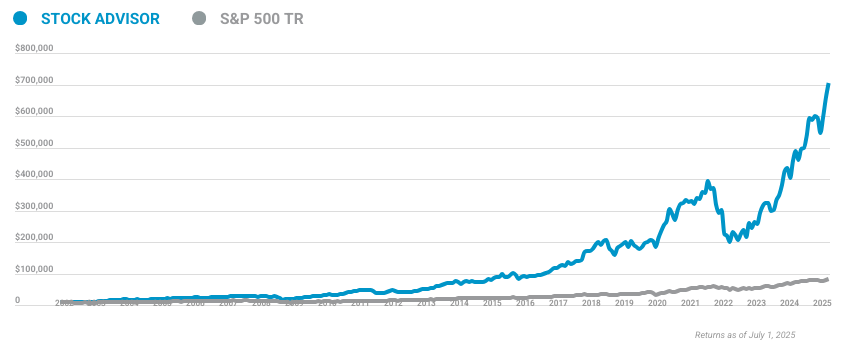
10 stocks we like better than Teladoc Health
When our award-winning analyst team has a stock tip, it can pay to listen. After all, the newsletter they have run for over a decade, Motley Fool Stock Advisor, has tripled the market.*
They just revealed what they believe are the ten best stocks for investors to buy right now... and Teladoc Health wasn't one of them! That's right -- they think these 10 stocks are even better buys.
*Stock Advisor returns as of February 8, 2023
Such forward-looking statements are subject to risks, uncertainties, and other factors that could cause the actual results for Teladoc Health to differ materially from those expressed or implied on this call. For additional information, please refer to our cautionary statement in our press release and our filings with the SEC, all of which are available on our website. I would now like to turn the call over to Jason.
Jason Gorevic -- Chief Executive Officer
Thank you, Patrick. Good afternoon, and thanks for joining us. This afternoon, I'm pleased to share strong fourth quarter results to finish what was undoubtedly a challenging year. Today, we're providing our 2023 guidance, which reflects a balanced approach to top and bottom-line growth, and we'll speak to changes to our reporting that will help you better track our progress.
First, let's start with a brief recap of the past quarter and year. Overall, despite a more challenging macro environment, our underlying business continues to perform with positive momentum, demonstrated by our ability to continue driving solid full year revenue growth. Fourth quarter consolidated revenue grew 15% year over year to $638 million, near the high end of our guidance range. For the full year, total revenue grew 18% to more than $2.4 billion.
Fourth quarter consolidated adjusted EBITDA of $94 million was in line with the outlook we provided in October, delivering upon our expectation for a significant margin increase in the quarter. We're pleased with the performance of our BetterHelp business, which grew 29% year over year in the fourth quarter, while delivering on our profitability target. We also remain excited about the momentum we're seeing for our integrated whole-person platform, which includes chronic care, mental health, and Primary360, now all accessible through a single login and account in our new unified app. Looking to 2023 and beyond, our leadership position in whole-person virtual care is clear.
The breadth and depth of our market-leading portfolio of products and services provides a strong platform for growth and expansion. I'm very pleased with our progress as we continue to deliver on our mission and realize our vision of making virtual care the first step on any healthcare journey. Top of mind, as we begin the new fiscal year is vendor consolidation. We hear a growing desire from our clients to shift away from point solutions and toward multiproduct integrated, virtual, and digital platforms.
At the same time, we're seeing clients increasingly focused on demonstrated results. Teladoc Health has been at the forefront of the adoption curve, and we believe that our scale, breadth of product offering, and proven outcomes will enable us to maintain and expand our position in the market. While there remains a healthy demand for solutions that promise better access and outcomes, while lowering the cost of healthcare, the challenging macro environment is likely to persist. This is particularly the case with regard to ongoing economic uncertainty as well as a moderation in overall market growth rates.
Given the current operating environment as well as the larger scale at which we now operate, you should expect us to balance growth and margin with an increased focus on efficiency going forward. Part of that approach is rightsizing the cost structure to reflect the current growth rates of the business. As such, the management team has been working diligently on ways to optimize the cost structure of the organization, which includes beginning the year with some tough decisions regarding layoffs and the restructuring of some teams. This restructuring will enable us to improve efficiency while still allowing us to effectively build upon our integrated virtual care offering in a market that remains in the early innings.
These actions are reflected in our Q1 and full year 2023 outlook. This more balanced approach does not mean that we will stop relentlessly pursuing growth and increased adoption of virtual care across the industry. Virtual care's role within the healthcare industry remains underpenetrated, and we will continue to invest to expand our leadership position. Our key strategic priorities remain our whole-person suite of services, including our virtual primary care offering, Primary360, our suite of chronic care management solutions and our mental health products, and continued growth in our BetterHelp consumer brand.
Access to our platform is available to over 80 million individuals in the U.S. today, primarily through our relationships with employers and health plans. Over 50% of that population has access to more than one of our products. And when I look at our suite of chronic care solutions, 30% of enrollees are now utilizing more than one chronic care product.
Our BetterHelp offering provided over 1 million individuals with access to mental healthcare over the past year, many of whom are unlikely to have received any care at all, if not for our services. Our platform enabled over 22 million visits across specialties last year and over 0.5 billion digital health interactions with an unmatched consumer experience and a Net Promoter Score over 60. That breadth and scale is unrivaled in the industry and gives us a strong foundation on which to expand. With the more balanced approach I referenced a moment ago, we will pursue growth in a more focused way with the goal of expanding our margins consistently over the next several years, as we march toward GAAP profitability while still achieving attractive and sustainable top-line growth rates.
You see this more balanced approach reflected in our 2023 guidance today. For the full year 2023, we expect revenue of $2.55 billion to $2.675 billion, representing year-over-year growth of 6% to 11%. We expect adjusted EBITDA of $275 million to $325 million, representing growth of 12% to 32%. You'll also notice some changes in the way that we report our results in today's press release, reflective of the way we are managing the business going forward.
As our BetterHelp direct-to-consumer brand has scaled up rapidly over the past few years, we also felt it is the appropriate time to provide increased disclosure for this business. As such, you will now see our results reported along two segments. Teladoc Health integrated care, which primarily consists of our B2B distribution channels including business sold through employers, health plans, and providers, both domestically and internationally; and BetterHelp, which primarily consists of mental health services sold through our direct-to-consumer distribution channel. Mala will discuss some of the additional assumptions underpinning our guidance in a moment, including how we're thinking about performance between these two segments.
Hopefully, you'll find this new disclosure helpful in modeling the business going forward. Let me end by saying, the company remains strongly positioned both strategically and financially. Our vision to deliver integrated whole-person virtual care and our multiproduct strategy continues to resonate in the marketplace. And from a financial perspective, we continue to generate positive free cash flow and maintain a strong balance sheet.
This is a clear differentiator for Teladoc Health, and provides us with the ability to invest in the expansion of our leadership position at a time when many of our smaller competitors are facing significant financial stress. With that, I'll turn the call over to Mala for a review of the fourth quarter and our forward guidance.
Mala Murthy -- Chief Financial Officer
Thank you, Jason, and good afternoon, everyone. Before I turn to the results for the quarter. I want to take a moment to discuss our new reporting structure. As Jason noted, you will see in today's release that we are now reporting along two new segments: Teladoc Health integrated care and BetterHelp.
On Page 7 of the press release, you will find segment results and metrics from the prior five quarters to help in your modeling. For the integrated care segment, in addition to revenue and adjusted EBITDA, we are reporting total U.S. membership with access to our suite of virtual program across our B2B distribution channels. This combines the prior categories of paid members, visit fee only members, and chronic care enrollees.
We believe the distinction between these member types is becoming less meaningful as the revenue models of our products have become more diverse over time and as we move toward more whole-person bundled and value-based arrangements. Revenue per U.S. integrated care member represents total segment revenue divided by reported U.S. integrated care membership.
We are also providing total chronic care program enrollment, which represents the total number of programs in which our members are actively enrolled. We believe program enrollment is more reflective of growth in chronic care revenue, as we continue to drive multi-program enrollment among our members. For the BetterHelp segment, in addition to revenue and adjusted EBITDA, we are reporting total BetterHelp users, which represents the average number of monthly paying users of the services during the period. Turning to results.
During the fourth quarter, consolidated revenue increased 15% year over year to $638 million. Fourth quarter adjusted EBITDA of $94 million was in line with the outlook we provided in October and represents a $43 million increase sequentially, primarily a reflection of the advertising spend seasonality in the direct-to-consumer business as we have discussed throughout 2022. Integrated care segment revenue increased 6% year over year to $357 million in the quarter, driven primarily by growth in Chronic Care Management and Telemedicine product revenue. integrated care added 5.8 million U.S.
members over the prior year, representing 7% year-over-year growth and 1.4 million sequentially to end the year with 83.3 million total U.S. members. Paid members were 58.7 million for the quarter, which exceeded the high end of our prior guidance range of 57 million to 58 million members. Total Chronic Care program enrollment exceeded 1 million programs in the fourth quarter, representing growth of 16% over the prior year's fourth quarter.
The total number of individuals enrolled in one of our Chronic Care programs was 805,000 during the quarter, an increase of 10% over the prior year's fourth quarter. Average integrated care segment revenue per U.S. member of $1.44 was down $0.02 over the prior year's fourth quarter due to the impact of new members onboarded over the course of the year. Excluding the dilutive impact of new member additions over the course of the year, revenue per U.S.
member would have increased by over 2% versus the prior year's quarter. Revenue per U.S. member increased $0.04 sequentially over the third quarter. Fourth quarter adjusted EBITDA from the integrated care segment grew 31% year over year to $43.7 million, while margins expanded 230 basis points to 12.2%.
Adjusted EBITDA growth was driven primarily by revenue growth and leverage over G&A expense. For the full year, Integrated segment revenue grew 6% to $1.4 billion, adjusted EBITDA declined 6% to $135 million driven primarily by increased technology and development expense. BetterHelp segment's revenue increased 29% year over year in the fourth quarter to $277 million, primarily driven by growth in BetterHelp membership. BetterHelp adjusted EBITDA grew 22% year over year to $52.8 million in the quarter.
Sequentially, adjusted EBITDA margin expanded 15 percentage points to 19.1%. This margin expansion was driven in large part by the seasonality of advertising spend, as we've discussed on prior calls. For the full year, BetterHelp segment revenue grew 41% to $1 billion. Adjusted EBITDA declined 6% to $114 million representing a margin of 11.2%, a reflection of the advertising market headwinds discussed last year.
Consolidated net loss per share in the fourth quarter was $23.49, compared to a net loss per share of $0.07 in the fourth quarter of 2021. Net loss per share in the fourth quarter includes a noncash goodwill impairment charge of $3.8 billion or $23.26 per share, stock-based compensation expense of $0.31 per share, and amortization of acquired intangibles of $0.30 per share. The goodwill impairment charge reflects the overall operating environment, including the lower rate of growth reflected in our guidance today, and overall financial market conditions, including decreased market multiples. This goodwill write-off is noncash and has no impact on our financial position or our ability to invest in the business going forward.
During the fourth quarter and full year, the company generated free cash flow of $12 million and $17 million, respectively. We ended the year with $918 million in cash and short-term investments on the balance sheet. Now turning to forward guidance. For the full year 2023, we expect revenue to be in the range of $2.55 billion to $2.675 billion representing revenue growth of 6% to 11%.
This revenue outlook contemplates mid- to high single-digit percentage growth in our integrated care segment, and low double-digit to mid-teen percentage growth in our BetterHelp segment. We expect total integrated care segment U.S. membership of 84 million to 86 million members. We expect consolidated adjusted EBITDA for the full year to be in the range of $275 million to $325 million or growth of 22% at the midpoint.
Consolidated guidance assumes year-over-year adjusted EBITDA margin of flat to up 50 basis points for the integrated care segment, and an increase of 100 to 300 basis points for the BetterHelp segment. We expect to generate free cash flow of at least $100 million in 2023, driven by both the growth in adjusted EBITDA, and an expected decline in capitalized software development costs. For the first quarter of 2023, we expect revenue of $610 million to $625 million, representing growth of 8% to 11% year over year. We expect adjusted EBITDA of $42 million to $50 million.
First quarter consolidated guidance contemplates low- to mid-single-digit revenue growth for the integrated care segment, and mid-to-high-teens revenue growth for the BetterHelp segment. Total integrated care segment U.S. membership is expected to increase to 84 million to 85 million members. We expect integrated care segment margins to be slightly higher than BetterHelp segment margins in the first quarter due to typical margin seasonality.
It's important to remind you of the seasonality dynamic in the BetterHelp business. As we have discussed throughout 2022, we typically see slower advertising spend in the fourth quarter during the holiday season. This drives lower customer acquisition in the back half of the fourth quarter and results in the strongest seasonal margin quarter of the year for BetterHelp. It also results in the seasonally weakest sequential growth and margins of the year in the first quarter as advertising spend is ramped up and the customer acquisition funnel rebuild.
As such, our guidance assumes the first quarter to be the low point of the year for BetterHelp margins, and we expect consistent margin progression over the course of 2023. With that, I will turn the call back to Jason.
Jason Gorevic -- Chief Executive Officer
Thanks, Mala. Before we go to Q&A, I also wanted to call your attention to our Third Annual Corporate Social Responsibility Report, we issued a few weeks ago. While all of our work is mission-driven, the fact that our 5,000 colleagues take giving back to the community as seriously as delivering for our members is a source of tremendous pride. The report covers a wide range of areas where we've had an impact in the past year from delivering more than 16,000 volunteer hours, 33% more than last year, to deploying 18 autonomous telehealth devices to Ukraine in cooperation with the World Telehealth initiative.
I'm grateful to my colleagues for demonstrating once again our core corporate value. We're passionate about taking care of people, and I encourage you to check out the report. With that, we're happy to take your questions. Operator?
Questions & Answers:
Operator
[Operator instructions] Please stand by. We are having some technical difficulties with the management team. Our first question comes from the line of Ryan Daniels of William Blair. Please proceed.
Jack Senft -- William Blair and Company -- Analyst
This is Jack Senft on for Ryan Daniels. I know you're not giving guidance specifically for the BetterHelp segment. But based on the BetterHelp users you outlined in your presentation deck, I'm curious on your expectations when it comes to growth within the user base more longer term. It looks like year-over-year fourth quarter increased pretty significantly.
So do you kind of expect BetterHelp to contribute more as a percent of total revenue over time? And just if you have any longer-term expectations on growth rates? That would be much appreciated. Thank you.
Mala Murthy -- Chief Financial Officer
Yeah. So thank you for the question. We're not in a position to give any outlook beyond 2023. We have given you hopefully, plenty of disclosure and detail for how we expect the BetterHelp business to be in 2023.
Look, it's -- at this point, BetterHelp is over a $1 billion business. I don't think you're going to see it return to the type of hyper growth that this business has seen over the past few years where it grew in -- well over 100% in the past few years. But we do think, importantly, that there remains a long runway for growth in this market. If you think about virtual therapy, it's still underpenetrated and a lot of the structural issues are on access and costs aren't getting addressed in other places.
So the tailwinds for this business are still very strong. The other important thing to note is, as Jason said in his remarks -- prepared remarks, we are making a choice this year to grow a little bit slower and drive margin improvement. We have talked about the 100 to 300 basis points of margin improvement in this business. And then the last thing, I'd say is BetterHelp is still likely to add more incremental revenue this year than, frankly, most of our competitors generate in total annual revenue.
It's just there is a lot of scale in this business, and there's a lot of scale advantage to take advantage of in this business.
Operator
Thank you. The next question comes from the line of Lisa Gill with J.P. Morgan. Please proceed.
Lisa Gill -- JPMorgan Chase and Company -- Analyst
Great. Thanks very much and good afternoon. Just really want to start with two things. Mala, you made an interesting comment around how the business is progressing going forward and you said whole-person value-based bundles.
So that's my question for Jason. Can you talk to me about what you're seeing for 2023? How do we think about how value-based bundles will work and what that means to revenue and profit? And then secondly, Mala, you talked about the improvement in the margin and by my math, it's like 130 basis points at the midpoint of what you've given. Can you maybe just talk about like what are some of the key drivers to that margin improvement? Is it mix? Is it the realignment of the business? Like what are some of the things that we should think about that maybe are specific to '23 or things that potentially will impact the margins as we think about beyond '23?
Jason Gorevic -- Chief Executive Officer
Yeah. Thanks, Lisa. There's no question that, especially health plans, but also increasingly large employers are looking for us to provide value-based arrangements. And value-based arrangements can take the form of being based on clinical outcomes, being based on bending the cost curve or some combination of the two of them.
In many cases, they are multiproduct bundles of services from us. And so if I look back at the last year, the interest from health plans and deals with value-based components is up about four x year over year. And that, I think, really plays well to us. Our outcomes proof points are clear, where we are driving significantly better outcomes when consumers engage in more than one of our clinical products.
And we're in a fortunate position now where for our chronic care solutions, 30% of our members, who are engaging with a chronic care solution, are engaging with more than one of them. But it's also true that we're driving significant return on investment for our clients, and that obviously lends itself well to value-based arrangements. On average, our diabetes program delivers a return on investment of three to one for our clients. For those who are significantly hypertensive, meaning over 140 systolic, we're driving $58 PPPM cost avoidance and so again, those lend themselves really well to aligning us with our clients in value-based arrangements.
Mala Murthy -- Chief Financial Officer
And then, Lisa, for your second question, if I think about our margin progression, I'd bring it down to a few key factors, right? First is, if you think about the better health margin improvement, it's really around the leverage we will get from A&M, improving the yield, the productivity of our A&M. More broadly, if you think about integrated care, it's about technology and development expense leverage and as well as G&A. As you know, we took some very difficult decisions earlier this year in terms of doing a layoff. And so if you think about the measures we are taking in controlling our costs, it is around driving G&A efficiency.
It's about things such as real estate consolidation. And internally, we are also driving efficiencies in our structure. We have centers of excellence now, etc, all of that essentially to rightsize our cost base relative to the growth rate of the business.
Operator
Thank you. The next question comes from Jailendra Singh of Truist Securities. Please proceed.
Jailendra Singh -- Truist Securities -- Analyst
Thank you and thanks for taking my questions. First, a quick clarification to your comment, Mala. Are you willing to quantify, how much benefit does your guidance assume from the recent restructuring for 2023? And my main question, Jason, you talked about the demand for multiproduct digital health platform increasing, employees moving away from point solutions. As you look across your solutions and offerings, are there certain areas or solutions where you would like to expand into to respond to that demand? And how do you plan to approach that in terms of like build, buy or partner?
Mala Murthy -- Chief Financial Officer
So we'll take it in order. We've given you all enough transparency on the restructuring we did. We've reduced our head count by approximately 6%, over 300 individuals during the first quarter. To be clear, the significant majority of that has been completed during the first quarter.
And it's fully incorporated in both our first quarter and full year guidance, Jailendra. And the only thing I would add to that is these actions that we are taking or we have taken, it follows a period of growing investment and they will moderate the pace of expense growth for 2023. And we believe this cost structure is reflective of the current growth rate of the business. It will allow us to improve the efficiency of the organization and importantly, while still allowing us to continue to innovate in the market.
That's still in relatively early innings.
Jason Gorevic -- Chief Executive Officer
And Jailendra, with respect to your question about multiproduct sales, there's no question that, that dominates both our pipeline and our bookings. About 70% of our bookings last year were multiproduct bookings. We continue to see that. I think it's also reflected in the success of our Primary360 product, which acts as a hub for multiple other products and clinical services.
Our Primary360 product continues to get significant traction. And although it's off a small base, we'll probably triple the revenue in '23 from Primary360 versus '22. So if you think about continued expansion of clinical products and services, we'll look to add additional products and services that are clinical capabilities that are complementary to both our existing chronic care portfolio as well as our Primary360 product and the full sort of primary care spectrum, if you will. In terms of build versus buy, we'll continue to look opportunistically across the market.
We look at both, a, speed to market; and b, financial return on those investments with respect to deciding whether we're going to build, buy or partner those. As I think has been well documented. There are a number of companies out there who are struggling in the current financial environment, and the cost of capital is significantly higher as other companies go out and have to raise money. We're staying closely attuned to that, but we're not stopping our pace of internal innovation.
And so you see that, for example, with the launch of our one app, which provides a single interface and a single consumer experience for all of our products and services and enables us to rapidly and relatively easily deploy additional products and clinical capabilities.
Operator
Thank you. The next question comes from the line of Stephanie Davis of SVB Securities. Please proceed.
Stephanie Davis -- SVB Securities -- Analyst
Hey, guys. Thanks for taking my questions. So I've been hearing about a lot of market growth outside of you guys for virtual primary care. So that would be helpful to walk through just the basics of the model for Primary360.
How you're charging for it? What you're seeing for RFP activity recently versus last year? And if we should view these wins as all incremental or if there's some cannibalization risk, as folks move to whole-person care versus virtual urgent care?
Jason Gorevic -- Chief Executive Officer
Yeah. Thanks, Stephanie. As I said, we're very excited about the growth in Primary360. I mentioned we expect triple the revenue in '23 that we saw in '22.
We have completed several thousand primary care visits already this year, and it's growing rapidly. We will deliver, I don't know, somewhere between five and 10x the visits in primary care in 2023 that we did in '22 and the pipeline is rich with opportunities. So I feel very good about where we are. In terms of cannibalization, we really don't see cannibalization of our general medical services by our Primary360 product.
They are really serving very different purposes. One is a longitudinal relationship that's really holistic and incorporates multiple of our products and services. The other is much more episodic and acute in nature. But I think what's encouraging for us, is that the combination of our chronic care solutions and mental health solutions come together with our Primary360 service to really provide that whole-person care.
Over half of our P360 members are using more than two of our Teladoc services, including our chronic care solutions. And we really see that members with chronic disease are four x as likely to engage with our Primary360 product. I think lastly, all of that is driving Net Promoter Scores in the 70s for our P360 product, which is not only providing new opportunities for us, but also expansion opportunities with existing clients.
Mala Murthy -- Chief Financial Officer
Yes. The thing I'll add is we are in the very early innings for virtual primary care. But we do think, based on the momentum we are seeing, over time, it has the potential to certainly become a much larger portion of the business. The pace of adoption over the next several years is certainly going to have an impact on the integrated care segment growth in particular.
Stephanie Davis -- SVB Securities -- Analyst
So taking that comment in line with the tripling of revenues for Primary360, how can we bridge to your guidance? You've got $200 million of incremental revenue dollars. It's on a base with a tripling Primary360, BetterHelp ending your double-digit growth, is there anything to call out that would prevent you from benefiting from those growth rates?
Jason Gorevic -- Chief Executive Officer
Well, remember, Stephanie, that Primary360 is off a very small base in '22, which I think we were consistent about saying over the course of last year, and we've given an indication of the growth rates of both the integrated care segment as well as the BetterHelp segment. So I think you can bring those together to look at what the overall guidance we've given for '23 is.
Operator
Thank you. The next question comes from the line of Richard Close. [Operator instructions] Richard, your line is now open. You may proceed with your question.
Richard Close -- Canaccord Genuity -- Analyst
Great. Thanks for the question. Appreciate that. Mala, can you talk a little bit more about the integrated margins, what you're seeing and what you're expecting? I guess, flat to 50 base improvements.
Just maybe a little bit more detail in the expansion opportunities maybe beyond 2023 in this business?
Mala Murthy -- Chief Financial Officer
Yeah. So here's what I would say, if you think about the integrated care segment. We will drive leverage in our expense base as our revenue continues to grow and scale. If you think about what the elements of that business are, and you'll see much more in the press release about what's in the integrated care segment.
But it's essentially think of it as growth across chronic care, Primary360, as we have talked about, our telemedicine business including mental health on the B2B side, and then growth in our hospital and health system business. So if you just think of the diversity of growth opportunities across all of these -- and I'm sorry, the last important one is international, right? Because again, this is a global integrated care segment. So again, if you think about the growth opportunities across all of these, the margin progression will come from driving revenue and scaling revenue, number one. And number two, as we've talked about, just being much more efficient in our costs and expenses in that segment, whether it be technology and development expense, we are going to drive leverage in T&D expense this year.
And we expect -- we will expect to continue to do that in future years. We are still investing to be clear in the business given the fact that we are still in the early innings, but we do expect to drive leverage there. And as I said, in SG&A as well. So it's the combination of those that will drive the margin progression in the integrated care segment.
Operator
Thank you. The next question comes from George Hill of Deutsche Bank. Please proceed.
Unknown speaker
It's Maxi on for George. Your provider model has been gradually changing from a pure contracting model to more of a hybrid model. Can you give us some color on where you are now in terms of contracted versus employed providers? And how do you -- how do the restructuring and cost-saving initiatives change this ratio and the pace of hiring to support membership growth? Thank you.
Jason Gorevic -- Chief Executive Officer
Yeah. So we're in the process. We haven't given out a percentage of the total visits that are being taken by employed versus independent contractor physicians, but we are in the process of shifting. I think you will see us go to north of 50% of our visit volume ultimately being taken by employed physicians.
What we've proven now is that we can drive actually greater physician productivity at higher consumer Net Promoter Scores and equal to better clinical integration of all of our products when we do that with an employed physician model. We'll never get to 100%, and that wouldn't be prudent, because it's not -- you get beyond the efficiency frontier at some point. And more and more, we are also moving to employed physicians for both our general medical, more episodic visits, as well as, of course, for our more longitudinal relationships in Primary360. I wouldn't point you to that transition when we talked about the restructuring that we did at the beginning of this year.
That was really not oriented around our physician staffing model, more it was around our opex and around our nonclinical staff.
Operator
Thank you. The next question comes from Jessica Tassan of Piper Sandler. Please proceed.
Jessica Tassan -- Piper Sandler -- Analyst
Hi. Thank you guys for taking the question. So I just was hoping you could help us square the increase in multiproduct sales with the kind of flattish average revenue per U.S. integrated care member over the course of 2022 relative to that 4Q '21 number you presented? And then just secondarily, Jason, if you could just remind us what's the level or type of behavioral care and care navigation that's embedded in the Primary360 offering?
Mala Murthy -- Chief Financial Officer
So if you -- what we said in our prepared remarks, Jess, is if you think about the revenue per member and you talk about flattish. Again, remember, we onboarded a lot of new members in 2022, and there is a dilutive impact of that. If you think about the growth in membership last year, it was about a 6% to 7% growth in members. So there is a dilutive impact.
If you normalize for that impact, as we said, on a year-over-year basis, we did see an increase in revenue per member of about 2% increase and it translated to about $0.04 sequentially. The point being that we are actually seeing the impact of the revenue growth, and the different elements and components of that in our revenue per member. And again, if you think about what is included in that revenue per member, it is increases in enrollment, it's increases in visit utilization. It is increases in the growth in our hospital and health systems business.
As we said, it is overall segment revenue growth and the different components of that, that will drive the increase in revenue per member.
Jason Gorevic -- Chief Executive Officer
And then with respect to Primary360, our standard offering for Primary360 60 delivers mental health along with virtual primary care, that mental health is -- tends to be therapy as well as access to psychiatry for medication management. Having said that, not every client takes our standard or full bundle of services. And so while that is our lead offering, I just caution you that not every product -- every client takes the same bundle of services.
Operator
Thank you. The next question comes from the line of Daniel Grosslight of Citi. Please proceed.
Daniel Grosslight -- Citi -- Analyst
Hi, guys. Thanks for taking my question. As we talk to benefits managers around virtual primary care, it seems like the integration of virtual and physical clinics has become increasingly important. I'm sure you hear the same thing.
Can you remind us how you guys integrate with in-person care and if your integration strategy has changed at all?
Jason Gorevic -- Chief Executive Officer
Yeah, Daniel. Thanks for the question. I think about it in terms of sort of three concentric circles. At the center is what we can deliver virtually for the consumer along all of the dimensions, including primary care, mental health, chronic care in a longitudinal and holistic manner.
The second ring is around what can be delivered in the home. And so more and more, we're driving care into the home and helping to facilitate care that can be delivered in the home, whether that's diagnostic testing or actual delivery of care in the home. And then the third ring is referrals into the delivery system. And we always work with our clients to strive to create the most efficient referral into the physical delivery system when someone needs to be referred.
The question of do -- I think that sometimes is behind that is do you want to own brick-and-mortar, so that you can refer into your own brick-and-mortar facilities. And I really don't -- I don't think that that's a highly scalable model. And I think in some cases, it can provide perverse incentives to fill your own beds and fill your own brick-and-mortar capacity rather -- I'd rather be in the business of making sure that we are making the best referral the first time for the highest clinical outcomes and the greatest impact on cost of care.
Operator
Thank you. The next question comes from Stan Berenshteyn of Wells Fargo. Please proceed.
Stan Berenshteyn -- Wells Fargo Securities -- Analyst
Hi. Thanks for taking my questions. I appreciate the additional color on BetterHelp, very helpful. Maybe on chronic care since nobody asked, 2020 was a pretty big enrollment year for chronic care.
I'm just wondering, are any of those contracts coming up for renewal? And maybe if you can comment on what your visibility is in that segment over the next year or two? Thanks.
Mala Murthy -- Chief Financial Officer
So as we have done our very detailed planning, as we always do for 2023, I would say, we have a high degree of visibility into our chronic care contracts. Importantly, as we have set guidance, we have been reasonably prudent about how much in your revenue to expect from -- on the integrated care segment including chronic care. So I would say that the level of visibility that we have is high.
Jason Gorevic -- Chief Executive Officer
And I wouldn't point to any significant contracts that are up over the course of this year.
Operator
Thank you. The next question comes from the line of Sandy Draper of Guggenheim. Please proceed.
Mitchell Ostrovsky -- Guggenheim Partners -- Analyst
Hi. Thanks. This is Mitchell on for Sandy. Just a few quick ones.
How are you thinking about the macro environment impact on your sales cycle? And also, are you seeing any impact to underlying membership of customers from the recent job cuts? Thanks.
Jason Gorevic -- Chief Executive Officer
Yeah. I'll take the first one -- the second one first. We haven't really seen an impact on our membership from anything that might be going on in the labor market. We're always attuned to that.
I'm very cognizant of the question, but we really haven't seen an impact. In some cases, we're balanced, because we participate in the commercial segments, exchange segments as well as the Medicaid segments. So sometimes we're insulated because we see a flow from one to the other, but we're really not seeing any significant impact. With respect to the buying behavior, we're more attuned to it in the BetterHelp segment and oriented around the sensitivity of the consumer, given the macroeconomic uncertainty.
And certainly, we've factored that into our outlook over the course of this year. I think in the B2B segment, it really has the effect of sometimes slowing down the buying process or the decision-making process, but doesn't necessarily stop it all together. I think if anything, it focuses the buyer on where they're getting the most value. And we believe that we rise to the top in that kind of an environment.
Operator
Thank you. The next question comes from Elizabeth Anderson of Evercore. Please proceed.
Elizabeth Anderson -- Evercore ISI -- Analyst
Hey, guys, Thanks so much for the question. I was wondering if you could give us a little bit more detail on BetterHelp. Like how are you sort of seeing any -- are you seeing any changes to retention compared to a year ago versus the macro environment and your change in ad spend? And then I was wondering if you could also give us an update on the group therapy sessions and how those are continuing to trend?
Mala Murthy -- Chief Financial Officer
Yes. So no changes really in any of those underlying metrics. If I think about [Technical difficulty]
Operator
One moment, we are experiencing technical difficulties. The management team will be back in a few moments. The Teladoc team is back. You may now resume.
Mala Murthy -- Chief Financial Officer
Sorry, Elizabeth, we are having network issues in our offices. We do apologize. But just to finish up on your question, what I would say is if you think about the underlying operating metrics of the BetterHelp business, they have remained steady as we have exited the year into this year whether it be LTV, retention, churn, etc. And we have also seen stability thus far in terms of ad pricing.
Now obviously, we are continuing to monitor that. And as we've talked about all of last year, that certainly is one of many swing factors in the BetterHelp business. But thus far, we have essentially seen a degree of stability in that market.
Operator
[Operator signoff]
Duration: 0 minutes
Call participants:
Patrick Feeley -- Vice President, Investor Relations
Jason Gorevic -- Chief Executive Officer
Mala Murthy -- Chief Financial Officer
Jack Senft -- William Blair and Company -- Analyst
Lisa Gill -- JPMorgan Chase and Company -- Analyst
Jailendra Singh -- Truist Securities -- Analyst
Stephanie Davis -- SVB Securities -- Analyst
Richard Close -- Canaccord Genuity -- Analyst
Unknown speaker
Jessica Tassan -- Piper Sandler -- Analyst
Daniel Grosslight -- Citi -- Analyst
Stan Berenshteyn -- Wells Fargo Securities -- Analyst
Mitchell Ostrovsky -- Guggenheim Partners -- Analyst
Elizabeth Anderson -- Evercore ISI -- Analyst